Fibroadenoma within a radial scar


CASE SUMMARY
A 54-year-old woman presented to the breast clinic with a spiculated mass seen at the 12 o’clock position in her right breast. The mass, found on routine mammographic screening, was nonpalpable and not associated with any skin or nipple changes. She had noprevious breast problems and denied any family history of breast cancer. She was postmenopausal and had never been on any hormone replacement therapy.
IMAGING FINDINGS
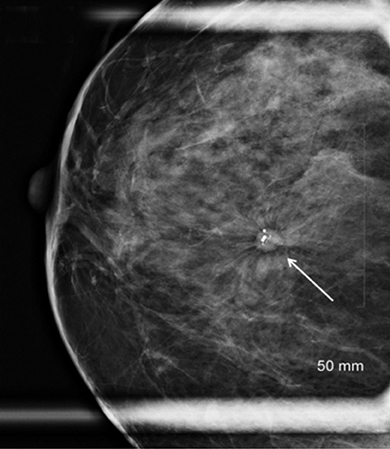
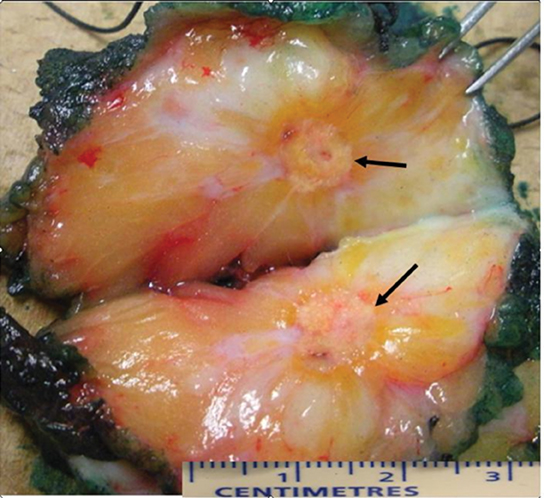
Mammography demonstrated in the craniocaudal and mediolateral planes long spicules surrounding central macrocalcifications contained within a mass (Figure 1). Ultrasound demonstrated the hypoechoic central mass, but the spicules were less obvious (Figure 2). An ultrasound-guided core biopsy was performed. Histological analysis of the percutaneous core biopsy demonstrated a fibroadenoma with large zones of fibrosis intermingled with zones of elastosis. Preliminary diagnosis was consistent with either a hyalinizing fibroadenoma or a fibroadenoma within a radial scar. Surgical excision was recommended. Final pathology confirmed a 0.9-cm fibroadenoma existing within a surrounding area of hyalinised stroma and sclerosing adenosis (Figure 3). There was no evidence of cytologic atypia or carcinoma in either the radial scar or fibroadenoma.
DIAGNOSIS
Fibroadenoma within a radial scar
DISCUSSION
Radial scars (RS) are radiographic and pathologically benign lesions of the breast that have been previously described in the literature under several different names, such as radial sclerosing lesion, scleroelastotic lesion, indurative mastopathy, nonencapsulated sclerosing lesion, sclerosing papillary proliferation, and, if larger than 1.0 cm, complex sclerosing lesion. Previously, most RS was reported as incidental microscopic lesions seen at biopsy for another lesion or at autopsy.1 However, in recent years, introduction of population based mammographic screening programs has led to the increased mammographic diagnosis of RS, with a prevalence of 0.04% in asymptomatic women.1,2
The mammographic appearances of RS are well documented. They are characterized by an area of architectural distortion and are defined according to the criteria of Tabar and Dean:3 (1) The presence of a central radiolucency, (2) the presence of radiating long thin spicules, (3)varying appearance in different projections, (4) radiolucent linear structures parallel to the spicules, and (5) absence of a palpable lesion or skin changes.
However, as many groups have demonstrated,none of these findings are specific, and similar features may be seen in carcinomas. Calcifications can be present or absent. RS may be difficult to see on ultrasound, but in this case the the associated fibroadenoma made it visible.
The exact pathogenesis of RS is unknown. They are benign lesions, but accumulating evidence indicates that they are associated with atypia and/or malignancy, and may be an independent risk factor for carcinoma in either breast.2-10 Pathologic examination of a radial scar often reveals a diverse array of pathologic findings including typical epithelial hyperplasia, sclerosing adenosis, papillomatosis,atypical epithelial hyperplasia, ductal carcinoma in situ (DCIS), and early stage invasive carcinomas. In fact, RS is clinically important as it may present in association with malignancies in 20% to 30% of patients. The relative risk of breast cancer for women with RS is1.88; when atypia is also present, the relative risk increases to 2.81.2,4
A mammographic lesion suggestive of radial scar is generally regarded as an indication for core needle biopsy. However, a percutaneous diagnosis of a radial scar does not exclude associated malignancy at surgical excision.4-7 Mammographic and sonographic features of a lesion diagnosed as a radial scar at percutaneous imaging-guided biopsy do not predict which lesions will have associated malignancy at surgery.5-7 Therefore, all patients with percutaneous diagnosis of a radial scar should undergo surgical excision regardless of mammographic and sonographic appearances, until further criteria can be determined. Recent reports suggest that using larger bore needles (11 gauge or larger) for core biopsy may improve the accuracy of the diagnosis and may potentially obviate the need for surgical excision.8-10 These patients may then be followed by serial mammographic surveillance.
CONCLUSION
Radial scar is a radiologic and pathologically benign entity that can not only be associated with atypia and/or malignancy, but may also be an independent risk factor for breast carcinoma. Its presence on imaging necessitates at the very minimum a percutaneous core biopsy for histologic diagnosis, but the lack of atypia or malignancy does not exclude associated malignancy at surgical excision. In view of this, excisional biopsy is justified in RS, although it has been argued that core biopsy evaluation and surveillance may be appropriate in selected patients.
REFERENCES
- Egyed Z, Péntek Z, Járay B, et al. Radial scar - significant diagnostic challenge. Pathol Oncol Res. 2008;14:123-129.
- Toth D, Sebo E, Sarkadi L., et al. Role of core needle biopsy in the treatment of radial scar. Breast. 2012;21:761-763.
- Kennedy M, Masterson AV, Kerin M et al. Pathology and clinical relevance of radial scars: A review. J Clin Pathol. 2003; 56: 721-724.
- Berg JC, Visscher DW, Vierkant RA, et al. Breast cancer risk in women with radial scars in benign breast biopsies. Breast Cancer Res Treat. 2008;108:167-174.
- Linda A, Zuinai C, Londero V, et al. Radial scars without atypia diagnosed at image-guided needle biopsy: How often is associated malignancy found at subsequent surgical excision and do mammograph and sonography predict which lesions are malignant? AJR.2010;194:1146-1150.
- López-Medina A, Cintora E, Múgica B, et al. Radial scars diagnosed at stereotactic core-needle biopsy: Surgical biopsy findings. Eur Radiol. 2006;16:1803-1810.
- Brenner RJ, Jackman RJ, Parker SH, et al. Percutaneous core needle biopsy of radial scars of the breast: When is excision necessary? AJR Am J Roentgenol. 2002;179:11791184.
- Cawson JN, Malara F, Kavanagh A, et al. Fourteen gauge needle core biopsy of mammographically evident radial scars: Is excision necessary? Cancer. 2003;97:345-351.
- Resetkova E, Edelweiss M, Albarracin CT, Yang WT. Management of radial sclerosing lesions of the breast diagnosed using percutaneous vacuum assisted core needle biopsy: recommendations for excision based on seven years’ of experience at a single institution. Breast Cancer Res Treat. 2011;127:335-343.
- Becker L, Trop I, David J, et al. Management of radial scars found at percutaneous breast biopsy. Can Assoc Radiol J. 2006; 57:72-78.
- Douglas-Jones AG, Denson JL, Cox AC, et al. Radial scar lesions of the breast diagnosed by needle core biopsy: analysis of cases containing occult malignancy. J Clin Pathol. 2007;60:295-298.
