MRI of the wrist












Magnetic resonance imaging represents a relevant way to diagnostically assess the wrist with high-resolution, multiplanar imaging without employing ionizing radiation. It influences clinical and surgical diagnosis and management of wrist pathologies.1 This article will discuss typical indications for advanced imaging of the wrist, including post-traumatic lesions, avascular necrosis, chondral injuries and arthritis,tendon pathologies and internal derangements of ligaments and the triangular fibrocartilage complex (TFCC).
MRI protocol
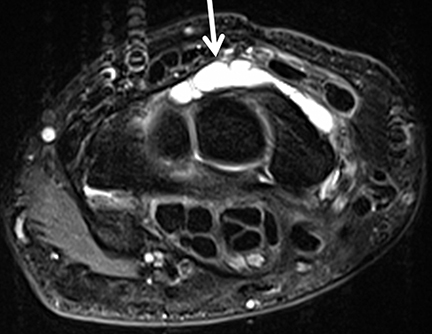
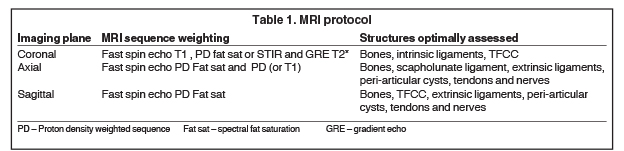
While varying among institutions, a typical wrist MRI protocol is shown in Table 1. It employs a small field of view (8 to 10 cm), and section thickness varies from 2mm to 3mm. A thinner section sequence (up to 1mm) is normally added (2D or 3D GRE T2* or more recent volumetric3D turbo spin echo proton density fat saturation sequences), which allows for multiplanar reconstruction in isotropic acquisitions. 3T MRI is preferable to 1.5T, given the better signal-to-noise ratio, contrast, and resolution of the images, all of which increase diagnostic accuracy.2 Direct or indirect MR arthrography (for both 1.5T and 3T) is employed as the standard of care in many institutions for assessing internal derangement,as multiple studies demonstrate the accuracy advantage of these techniques, particularly of 3T MR arthrography. However, whether arthrography is necessary for all cases remains unclear. Given the technological advances in MRI systems, dedicated coils and new sequences, the authors perform 3T MRI as a default at our institution, and reserve arthrography for selected postoperative cases, or for cases of clinical-radiological mismatch in which surgery is being considered.3-8
Bones and cartilage
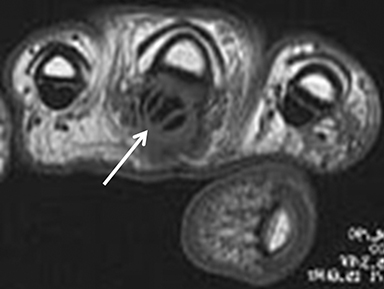
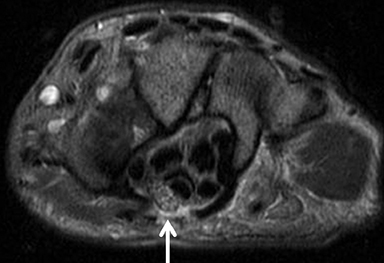
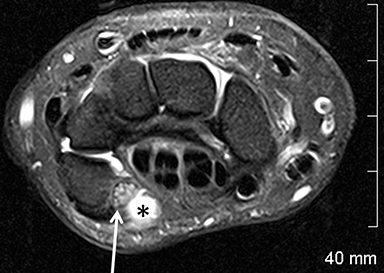
Occult fractures are detected as linear, low signal intensity on the T1-weighted sequence with surrounding bone marrow edema (Figure 1).Areas of bone contusion are differentiated mainly by the absence of a clear fracture line (Figure 2).9 Typical areas include the scaphoid, the tubercle of trapezium (radial-sided pain), the hook of the hamate (ulnar/volar-sided pain) and the distal radius.
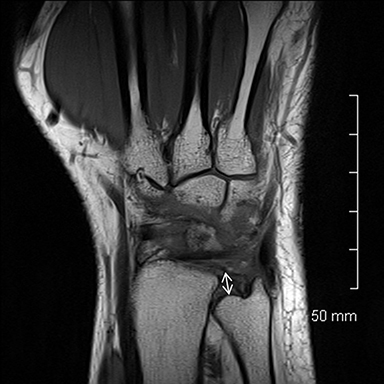
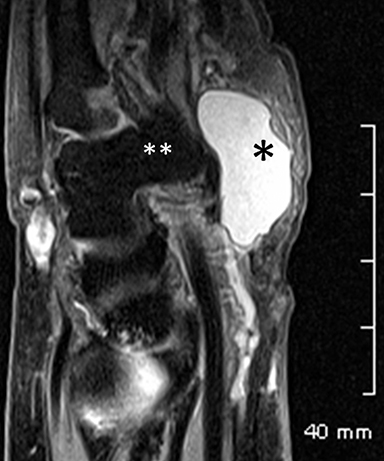
Avascular necrosis (AVN) of the lunate (Kienbock’s disease) is characterized initially by high signal intensity on fluid sensitive sequences,with low signal intensity on all sequences later in disease progression. A typical coronal plane fracture and bone fragmentation may follow, with further progression of OA changes of the carpus (Figure 3).10 AVN of the proximal pole of the scaphoid may happen in 30% of scaphoid waist fractures and up to 100% of proximal pole fractures. It may also present initially as nonspecific increased signal intensity on the fluid sensitive sequences. Enhancement with IV contrast is associated with viability of the fragment,11 while low signal on all sequences (corresponding to sclerosis on radiographs and CT) is compatible with established necrosis (Figure 4).
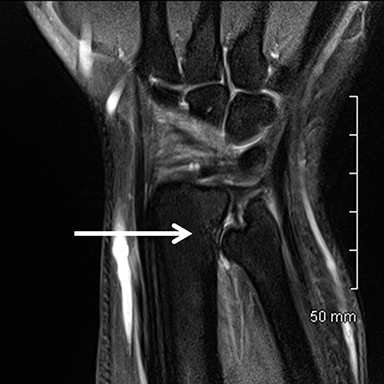
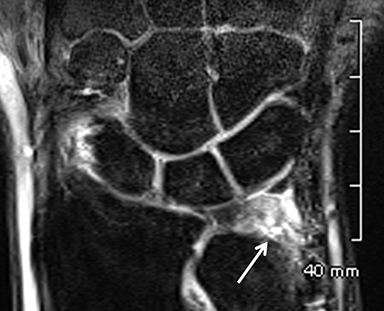
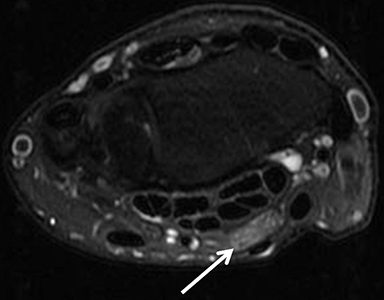
After initial radiographic assessment, ulnar-sided pain with suspected impaction syndromes may be assessed further by MRI, with clear demonstration of the bone anatomy, signal and, eventually, associated internal derangements. Typical findings include:a) ulnocarpal abutment syndrome: subchondral bone marrow edema and cystic changes of the ulnar margin of the lunate, triangular fibrocartilage degeneration or tear, frequently with positive ulnar variance (Figure 5);b) ulnar styloid impaction syndrome: a prominent ulnar styloid, previous styloid non-union or accessory ossicle, as well as edema and cystic changes in the styloid and triquetrum;c) hamatolunate impaction syndrome: a type 2 lunate (anatomical variant lunate defined by a clear articular facet with the hamate), chondropathy and associated subchondral marrow signal alteration (Figure 5); and,d) ulnar impingement syndrome: a shortened and radially convergent distal ulna, with signal changes and remodeling at the radio-ulnar interface (Figure 5).12 MRI often reveals carpal bone cysts, commonly called bone ganglia, and demonstrates their relation to cortical defects, ligament injuries and associated soft tissue ganglia.13 Found most often in the scaphoid and lunate, bone ganglia may be differentiated from subchondral cysts due to associated deep chondropathy.
Ligaments
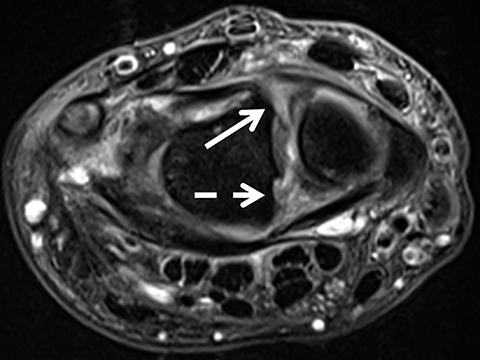
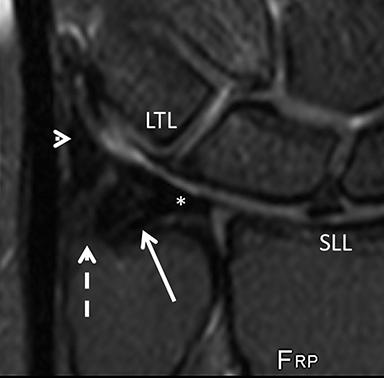
The scapholunate ligament (SLL) is the most relevant intrinsic ligament of the wrist that can be assessed with MRI. The SLL comprises 3 bands, of which the dorsal is mechanically the most important, followed by the volar and central bands. The volar band, protected by a strong adjacent extrinsic ligament, is less prone to injury. The third and less relevant central band, a membranous portion, is frequently perforated in adult individuals without clear consequence for wrist biomechanics. For this reason, communication between the radiocarpal and midcarpal compartments during fluoroscopic or MR arthrograms does not necessarily represent a symptomatic finding or reflect a traumatic tear of the ligament. As a result, the different bands should be assessed separately with MRI.
The dorsal band is easily seen on axial-plane and coronal-plane images, where it often presents some degree of partial-volume artifact.In normal cases, it is a continuous, thin, low-signal-intensity band bridging the chondral margins of the lunate and scaphoid. The insertion in the hyaline cartilage should not be mistaken for a tear. Signal changes and altered thickness may represent degeneration or even previous partial injuries, and are sometimes associated with a ganglion. The accuracy of these findings is, however, controversial.15 Disruption or indistinction of the fibers indicates a full-thickness tear of the component. Tears of the dorsal component or complete tears (disruption of all 3 components) are also more frequently symptomatic and secondary to trauma (Figure 7).16 Widening of the scapholunate interval may be seen, but this finding implies an associated injury of the extrinsic ligaments.17 A similar rationale is applied to the volar component, except that it may demonstrate intermediate signal intensity in normal cases.18
The lunotriquetral ligament (LTL) is also composed of three components, but the volar band is the most relevant for stability. The whole extension of the ligament and its tears may be difficult to detect; the presence of a step-off between the lunate and triquetrum, central tears of the triangular fibrocartilage, and findings compatible with ulnocarpal abutment warrant careful LTL examination.19
The multiple dorsal and volar extrinsic ligaments are low-signal bands overlying the carpal bones and intrinsic ligaments.20 Signal changes along their topography in cases of posttraumatic injury may indicate sprain.19 Often, a ganglion cyst may also be seen traversing ligamentous fibers toward the superficial soft tissues.
Triangular fibrocartilage complex (TFCC)
The TFCC is composed of the triangular fibrocartilage proper (TFC) and its periphery. The TFC demonstrates low signal intensity on all sequences and a smooth, biconcave morphology, attaching to the hyaline cartilage of the radius at one margin, and to the ulnar styloid and fovea at the other margin as two low-signal bands (Figure 8). Between these bands is a moderate-to-high-signal-intensity vascularized fibrous tissue(ligamentum subcruentum).19 The remaining structures of the periphery, including the homologue meniscus, the ulnar collateral ligament, and the sheath of the extensor carpi ulnaris tendon, among others, are more difficult to confidently depict and isolate.
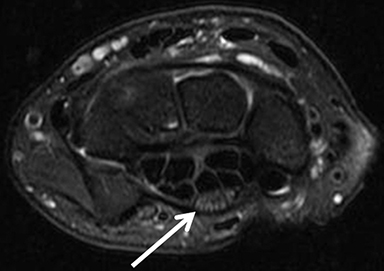
Owing in part to these characteristics, injuries of the TFC proper are confidently depicted by MRI; they include degenerative signal changes,non-communicating defects (or partial tears) of the surfaces, and communicating defects (full-thickness tears). Degeneration and central/membranous tears can be seen in asymptomatic individuals, and their prevalence increases with patient age (Figure 9). Peripheral injuries are less accurately diagnosed. A peripheral tear is suspected if high signal intensity along the ulnar insertions, detachment from the ulna, or synovitis are present. Intravenous contrast or MR arthrography with injection in the distal radio-ulnar joint may be necessary in such cases.21 Note that peripheral non-communicating defects have been more commonly associated with symptoms, typically as localized ulnar-sided wrist pain.22 (Figure10).
Tendons
The flexor and extensor tendons present typical low signal intensity and constant diameter on all sequences. Tendinopathy presents as signal and thickness changes on MRI, and may progress to partial- or full-thickness tears, with or without associated fluid and synovitis of the sheath(tenosynovitis, Figure 11). Note that the magic angle effect may artifactually increase the signal of normal tendons oriented approximately 54° in relation to the main magnetic field on sequences with a short time of echo, such as T1- and PD-weighted sequences. This not infrequently affects the extensor pollicis longus tendon (third extensor compartment).
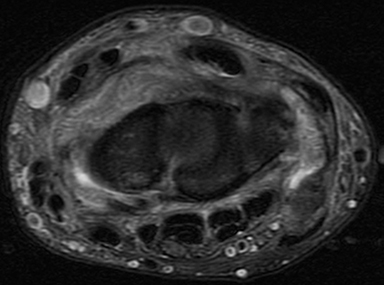
While most cases of tenosynovitis are due to overuse/degenerative changes, other etiologies such as gout, rheumatoid arthritis, amyloidosis, septic and mycobacterial tenosynovitis and sarcoidosis remain in the differential diagnosis. In addition to tenosynovitis, gout is especially known to cause dramatic alterations in tendon signal and caliber (Figure 12).
An intersection syndrome refers to pain and swelling at areas of intersection between the tendon compartments. A proximal intersection syndrome refers to the crossing between the first and second extensor compartments at the distal dorsal radial aspect of the forearm, whereas a distal intersection syndrome refers to the crossing between the third and second compartments at the level of the tubercle of Lister. Findings include focal peritendinous edema, tendon thickening and tenosynovitis.23,24
In cases of trauma with tendon retraction, the tendinous stumps should be identified and the protocol tailored to the clinical question, for example, by enlarging the field of view, substituting the coil, or complementation with forearm MRI.
Nerves
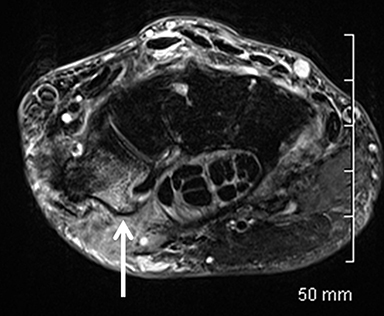
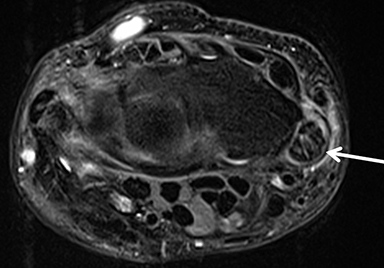
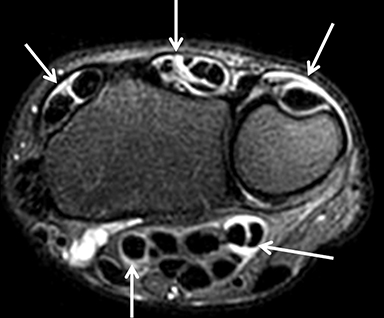
The median nerve travels through the carpal tunnel and normally should not present variations in signal or thickness. Main findings in cases of compressive neuropathy (carpal tunnel syndrome) are thickening of the nerve proximal to the entrance of the tunnel with associated increased signal on the fluid-sensitive sequences (Figure 13). However, the findings may not be specific. More recently, diffusion tensor MRI (DTI) has been studied as a new tool for diagnosing neuropathy.25The role of MRI in carpal tunnel syndrome is to exclude a potential cause for the symptoms, such as flexor tenosynovitis, or masses/cysts within the carpal tunnel.26An incidental bifid median nerve and/or a persistent median artery should also be depicted and reported (Figure 14).27
MRI after carpal tunnel release is sometimes indicated to evaluate recurrence of symptoms. Normal postoperative findings include a complete surgical defect of the flexor retinaculum and volar extrusion of the carpal tunnel components through it, with improvement of neural signal changes. Persistent altered neural thickness may be seen (Figure 15).28 Rarely, median nerve lipomatosis (fibrolipomatous hamartoma) is detected in the investigation of macrodystrophia lipomatosa or carpal tunnel syndrome.29,30 In these situations the nerve presents a “spaghetti-” or “multi-cable-like” appearance, with thickened fascicles and prominent fatty interstitial tissue.
The ulnar nerve travels through the canal of Guyon (ulnar nerve tunnel) along the ulnar aspect of the wrist and is the most ulnar structure in the canal, in close proximity to the pisiform and hook of the hamate. Neuropathy may be associated with ganglia and masses within the tunnel,compression due to accessory muscle slips around the nerve, or even fractures or stress injuries of the hook of the hamate (Figure 16).31
Arthritis
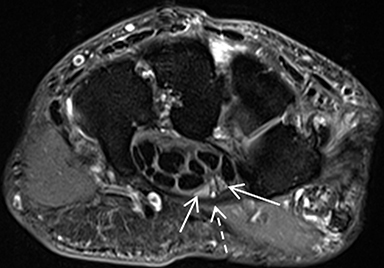
Radiography is the primary modality used to diagnose and stage arthritis of the hands and wrist. Osteoarthritis may incidentally be seen on MRI as areas of chondropathy, bone-marrow edema, cysts, and sclerosis, as well as areas of osteophyte formation, joint effusion and synovial reaction. Internal derangements such as SLL or TFC tears may be associated. Large field-of-view MRI of the hands is employed in many centers to investigate and stage cases of inflammatory arthropathies such as rheumatoid and psoriatic arthritis. Findings include synovitis and marrow edema,bone erosions, periarticular cysts and tenosynovitis (Figure 17).32 Investigating inflammatory arthropathies warrants the use of intravenous gadolinium.33 Acute and subacute carpal infections and tenosynovitis are characterized by synovitis and erosions, as well as by capsular and soft-tissue edema in variable degrees, and also warrant the use of IV contrast (Figure 18).
Ganglia
Ganglia are the most common benign tumors of the soft tissues of the hands, found in both the volar and dorsal periarticular topographies.A ganglion is defined as a cyst in contact with a joint capsule or tendon sheath. It contains thick, gelatinous material and a thin capsule,without internal synovial lining. Ganglia may be connected to injured ligaments or demonstrate intra-osseous extension. However, their etiology is still not clear. They present with high signal intensity on fluid-sensitive sequences and low signal on T1-weighted sequences, and they may be complex, with debris, loculations or septations. Not infrequently, ganglia may be occult or incidental, sometimes insinuating through the extrinsic ligaments of the wrist (Figure 19).34
Conclusion
To sum up, MRI of the wrist is a relevant tool for diagnosis and clinical management of wrist pain, including the evaluation of traumatic injuries and chronic syndromes.
References
- Hobby JL, Dixon AK, Bearcroft PW, et al. MR imaging of the wrist: Effect on clinical diagnosis and patient care. Radiology. 2001;220: 589-593.
- Lenk S, Ludescher B, Martirosan P, et al. 3.0 T high-resolution MR imaging of carpal ligaments and TFCC. Rofo. 2004. 176: 664-667.
- Haims AH, Schweitzer ME, Morrison WE , et al. Internal derangement of the wrist: indirect MR arthrography versus unenhanced MR imaging. Radiology. 2003;227:701-707.
- MageeT. Comparison of 3-T MRI and arthroscopy of intrinsic wrist ligament and TFCC tears. AJR Am J Roentgenol. 2009;192: 80-85.
- Maizlin, ZV, Brown JA, Clement JJ, et al. MR arthrography of the wrist: Controversies and concepts. Hand. 2009;4: 66-73.
- Hobby JL, Tom BD, Bearcroft PW, Dixon AK. Magnetic resonance imaging of the wrist: Diagnostic performance statistics. Clin Radiol. 2001;56: 50-57.
- Lee RK, NG AW, Tong CS, et al. Intrinsic ligament and triangular fibrocartilage complex tears of the wrist: comparison of MDCT arthrography, conventional 3-T MRI, and MR arthrography. Skeletal Radiol. 2013; 42:1277-1285.
- Smith TO, Drew B, Toms AP, et al. Diagnostic accuracy of magnetic resonance imaging and magnetic resonance arthrography for triangular fibrocartilaginous complex injury: a systematic review and meta-analysis. J Bone Joint Surg Am. 2012;94: 824-832.
- Senevirathna S, Rajeev A, Newby M.The value of delayed MRI scans in the assessment of acute wrist injuries. Acta Orthop Belg. 2013; 79:275-279.
- Schmitt R, Heinze A, Fellner F, et al. Imaging and staging of avascular osteonecroses at the wrist and hand. Eur J Radiol.1997; 25: 92-103.
- Schmitt R, Christopoulos G, Wagner M, et al. Avascular necrosis (AVN) of the proximal fragment in scaphoid nonunion: is intravenous contrast agent necessary in MRI? Eur J Radiol. 2011; 77: 222-227.
- Cerezal L, del Piñal F, Abascal F, et al. Imaging findings in ulnar-sided wrist impaction syndromes. Radiographics. 2002; 22: 105-121.
- Uriburu IJ, Levy VD. Intraosseous ganglia of the scaphoid and lunate bones: Report of 15 cases in 13 patients. J Hand Surg Am. 1999; 24: 508-515.
- Conway WF, Destouet JM, Gilula LA, et al. The carpal boss: An overview of radiographic evaluation. Radiology. 1985; 156: 29-31.
- Spaans AJ, Minnen PV, Prins HJ, et al. The value of 3.0-tesla MRI in diagnosing scapholunate ligament injury. J Wrist Surg. 2013; 2:69-72.
- Linkous, M.D., S.D. Pierce, and L.A. Gilula, Scapholunate ligamentous communicating defects in symptomatic and asymptomatic wrists: characteristics. Radiology, 2000. 216: 846-50.
- Theumann NH, Etechami G, Duvoisin B, et al. Association between extrinsic and intrinsic carpal ligament injuries at MR arthrography and carpal instability at radiography: Initial observations. Radiology. 2006; 238: 950-957.
- Totterman SM, Miller RJ. Scapholunate ligament: normal MR appearance on three-dimensional gradient-recalled-echo images. Radiology. 1996; 200:237-241.
- Ringler, MD, MRI of wrist ligaments. J Hand Surg Am, 2013. 38: 2034-2046.
- Theumann NH, Pfirrmann CW, Antonio GE, et al. Extrinsic carpal ligaments: Normal MR arthrographic appearance in cadavers. Radiology. 2003;226: 171-179.
- Ruegger C, Schmid MR, Pfirrmann CW, et al. Peripheral tear of the triangular fibrocartilage: Depiction with MR arthrography of the distal radioulnar joint. AJR Am J Roentgenol. 2007; 188:187-192.
- Zanetti M, Linkous MD, Gilula LA, Hodler J. Characteristics of triangular fibrocartilage defects in symptomatic and contralateral asymptomatic wrists. Radiology. 2000; 216: 840-845.
- Costa CR, Morrison WB, Carrino JA. MRI features of intersection syndrome of the forearm. AJR Am J Roentgenol. 2003; 181:1245-1249.
- Parellada AJ, Gopez AG, Morrison WB, et al. Distal intersection tenosynovitis of the wrist: a lesser-known extensor tendinopathy with characteristic MR imaging features. Skeletal Radiol. 2007;36:203-208.
- Yao L, Gai N. Median nerve cross-sectional area and MRI diffusion characteristics: normative values at the carpal tunnel. Skeletal Radiol. 2009; 38:355-361.
- Allmann KH, Horch R, Uhl M, et al. MR imaging of the carpal tunnel. Eur J Radiol. 1997; 25: 141-514.
- Pierre-Jerome C, Smitson RD Jr, Shah RK, et al. MRI of the median nerve and median artery in the carpal tunnel: prevalence of their anatomical variations and clinical significance. Surg Radiol Anat. 2010;32:315-322.
- Mesgarzadeh M, Schneck CD, Bonakdarpour A, et al. Carpal tunnel: MR imaging. Part II. Carpal tunnel syndrome. Radiology. 1989; 171:749-754.
- Louaste J, Zejjari H, Chkoura M, et al. Carpal tunnel syndrome due to fibrolipomatous hamartoma of the median nerve. Hand. 2011; 6:76-79.
- Blacksin M, Barnes FJ, Lyons MM. MR diagnosis of macrodystrophia lipomatosa. AJR Am J Roentgenol. 1992; 158: 1295-1297.
- Waugh RP, Pellegrini VD. Ulnar tunnel syndrome. Hand Clin. 2007; 23:301-310.
- Navalho M, Resende C, Rodrigues AM, et al. Bilateral MR imaging of the hand and wrist in early and very early inflammatory arthritis: tenosynovitis is associated with progression to rheumatoid arthritis. Radiology. 2012;264:823-833.
- Navalho M, Resende C, Rodrigues AM, et al. Bilateral evaluation of the hand and wrist in untreated early inflammatory arthritis: a comparative study of ultrasonography and magnetic resonance imaging. J. Rheumatol. 2013;40:1282-1292.
- Lowden CM, Attiah M, Garvin G, et al. The prevalence of wrist ganglia in an asymptomatic population: Magnetic resonance evaluation. J Hand Surg Br. 2005;30:302-306.
