Radiological Case: Retrorectal cystic hamartoma (Tailgut cyst)

CASE SUMMARY
A 30-year-old asymptomatic female presented for IUD placement 5 months after an uncomplicated C-section. Ultrasound confirmed correct IUD placement but revealed a “complex pelvic mass” in the posterior cul-de-sac. Rectovaginal exam revealed a nontender soft tissue mass, 6-7cm in size, just to the right of the rectum and vaginal apex. Pelvic MRI showed a 7 cm mass deep in the right hemipelvis, felt to possibly represent an endometrioma, which remained unchanged on a 3-month follow-up study. Colonoscopy revealed extrinsic bowel compression but no mucosal changes. Due to recent pelvic surgery, the imaging characteristics of the mass, and the normal appearance of both ovaries, a gossypiboma was considered. Exploratory laparotomy revealed a right perirectal retroperitoneal mass containing copious amounts of keratin. The mass was excised and the patient had an uneventful recovery.
IMAGING FINDINGS
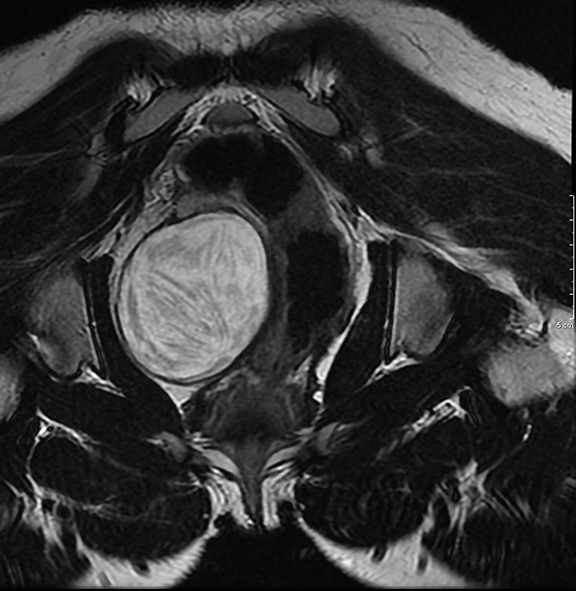
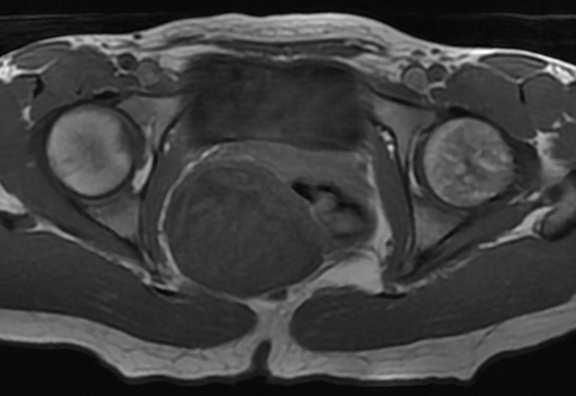
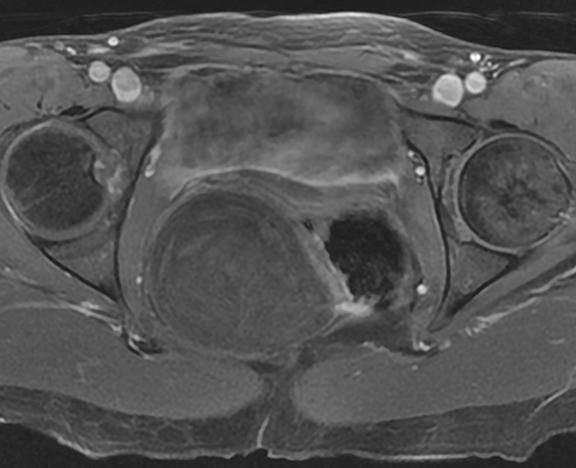
The initial and follow-up pelvic MR images demonstrated a well-defined, non-enhancing, ovoid lesion within the cul-de-sac which exerted mass effect on the uterus (Figure 1) and was distinct from both ovaries. The lesion exhibited high T2 and low T1 signal as well as several areas of linear low T2 signal internally with a somewhat “whorled” appearance (Figure 2). In addition, there was no signal loss on fat saturated images (Figure 3). Given these findings and the patient’s clinical history, the differential diagnosis included gossypiboma, retrorectal cystic hamartoma, epidermal inclusion cyst and endometrioma.
DIAGNOSIS
Retrorectal cystic hamartoma (Tailgut cyst)
DISCUSSION
Tailgut cysts can be diagnosed at all ages but are seen more commonly in middle-age females.1 Most tailgut cysts are found incidentally, as patients are often asymptomatic at presentation.1,2,3 Presenting symptoms are usually secondary to mass effect from an enlarging cyst and may include pelvic and perineal pain, increased urinary frequency, rectal fullness and bleeding, and a change in stool caliber.8 Several different terms have been used in the literature to describe these cysts ranging from tailgut cyst to retrorectal hamartoma, cyst of the postanal intestine, mucus-secreting cyst, retrorectal cyst and enterogenous cyst. Due to confusion in terminology, different papers may use any of the aforementioned terms, especially in papers published before 1988, when Hjermstad and Helwig put together a review of 53 cases bringing the diagnostic term forward.4
Tailgut cysts are believed to originate from the remnants of the embryonic hindgut. On gross evaluation, tailgut cysts tend to be multiloculated with a thin, glistening wall and are filled with mucoid or keratin material. Microscopically, these cysts can be lined with multiple types of epithelium including mucin-secreting columnar epithelium and sometimes areas of squamous and transitional epithelium.5 An incomplete muscle layer is often associated with the cyst wall. Infected cysts may show fibrosis of the cyst wall and breakdown of the epithelial lining. Malignant transformation of tailgut cysts has been very rarely reported but may include adenocarcinomas, carcinoid, neuroendocrine carcinoma, and sarcoma.2,6,7
In addition to tailgut cysts, other differential diagnoses that should be considered when a presacral mass is discovered include epidermoid cyst, dermoid cyst, endometrioma, rectal duplication cyst, anal gland cyst, and anterior meningocele.8 A physical exam, colonoscopy and imaging studies can be helpful in narrowing the differential diagnosis. On CT, these lesions are typically well-marginated, thin-walled, uni- or multilocular, nonenhancing lesions in the retrorectal space. Rare cases of associated thin calcifications have been reported. If secondarily infected, the cyst may be thick walled with surrounding inflammatory changes.8 Uncommonly, the cyst may contain air due to the presence of a fistula. On ultrasound, a developmental cyst appears as a unilocular or multilocular retrorectal cystic lesion, sometimes with internal echoes due to mucoid material or inflammatory debris.6 On MR these are well-circumscribed, thin-walled, hypointense lesions on T1-weighted images and a homogeneous, hyperintense lesion on T2-weighted images. High signal intensity on T1-weighted images is likely secondary to mucoid content. Septa are more conspicuous on T2-weighted images with low signal intensity. Focal irregular wall thickening with intermediate signal intensity on both T1- and T2-weighted images and with enhancement after contrast material injection is suggestive of malignant degeneration.8
Unfortunately, radiographic signs are not specific for this entity and it is often difficult to distinguish tailgut cysts from alternative diagnoses. Therefore, complete surgical resection remains necessary for both diagnosis and definitive treatment.
CONCLUSION
Tailgut cysts represent a rare clinical and radiologic finding that should be considered when a mass is found in the presacral space, particularly in middle-age females. This case highlights both the imaging findings and the importance of surgical exploration in the diagnosis of this entity.
REFERENCES
- Krivokapic Z, Dimitrijevic I, Barisic G, et al. Adenosquamous carcinoma arising within a retrorectal tailgut cyst: Report of a case. World J Gastroenterol. 2005;11(39): 6225-6227.
- Prasad A, Amin M, Randolph T, et al. Retrorectal cystic hamartoma. Arch Pathol Lab Med. 2000;124(5):725-729.
- Jarboui S, Jarraya H, Ben Mihoub M, et al. Retrorectal cystic hamartoma associated with malignant disease. Canadian J Surg, 2008: 51(6); E115-E116.
- Hjermstad B, Helwig E. Tailgut cysts. Report of 53 cases. The Am J Clin Pathol. 1988;89(2): 139-147.
- Marco V, Autonell J, Farre J, et al. Retrorectal cyst-hamartomas. Report of two cases with adenocarcinoma developing in one. Am J Surg Pathol. 1982; 6(8); 707-714.
- Lim K, Hsu W, Wang C. Tailgut cyst with malignancy: MR imaging findings. AJR Am J Roentgenol. 1998;170 (6) 1488-1490.
- Moulopoulos L, Karvouni E, Kehagias D, et al. MR imaging of complex tailgut cysts. Clin Radiol. 1999; 54(2); 118-122.
- Dahan H, Arrive L, Wendum D, et al. Retrorectal developmental cysts in adults: Clinical and radiologic histopathologic review, differential diagnosis, and treatment. Radiographics 2001;21(3);575-584.
