Telangiectatic Osteosarcoma
By Nielsen CS, Towbin RB, Schaefer CM, Towbin AJ, Aria DJ

Case Summary
An adolescent presented with dull, achy pain, swelling, and reduced range of motion of their left shoulder.
Imaging Findings
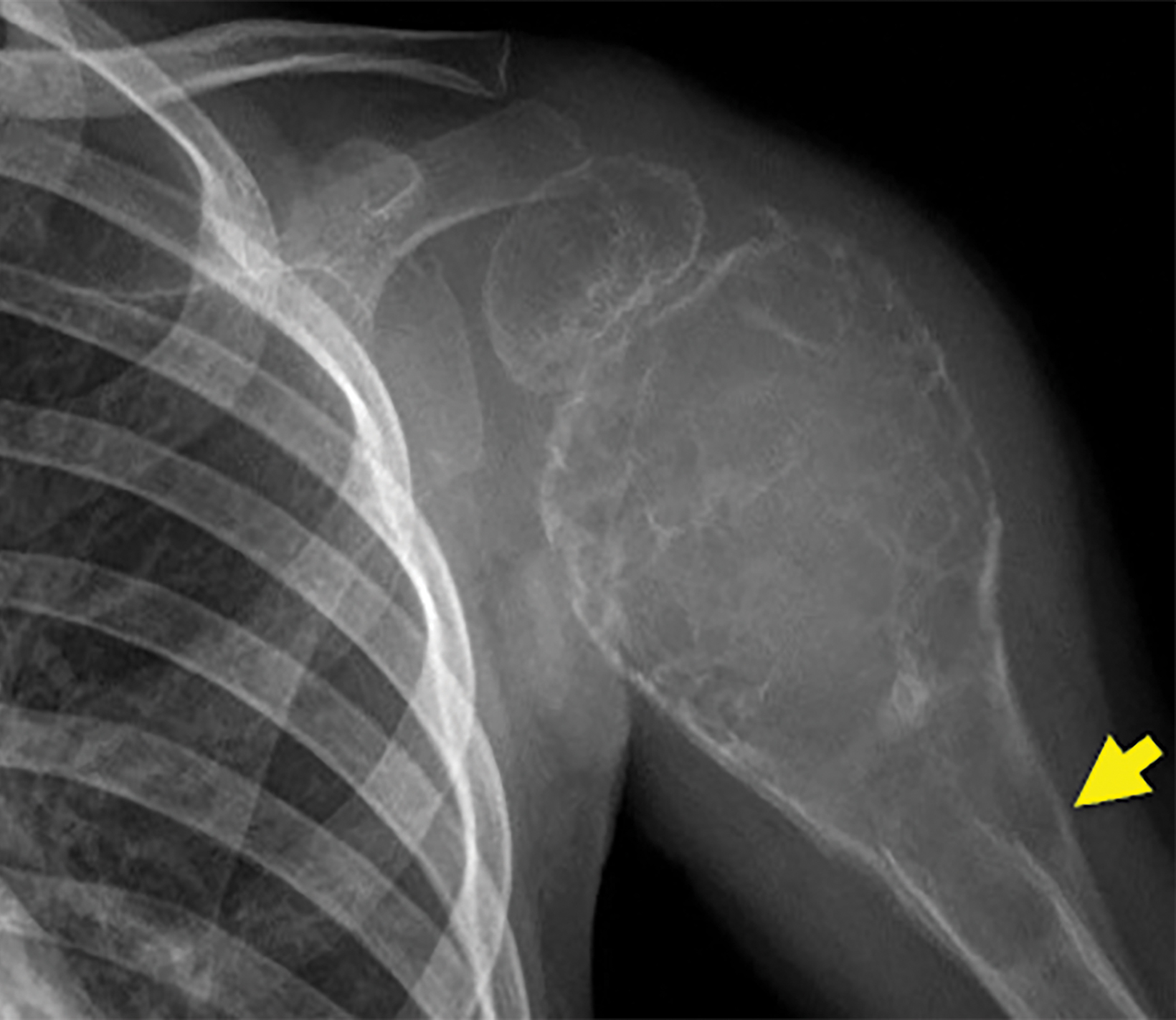
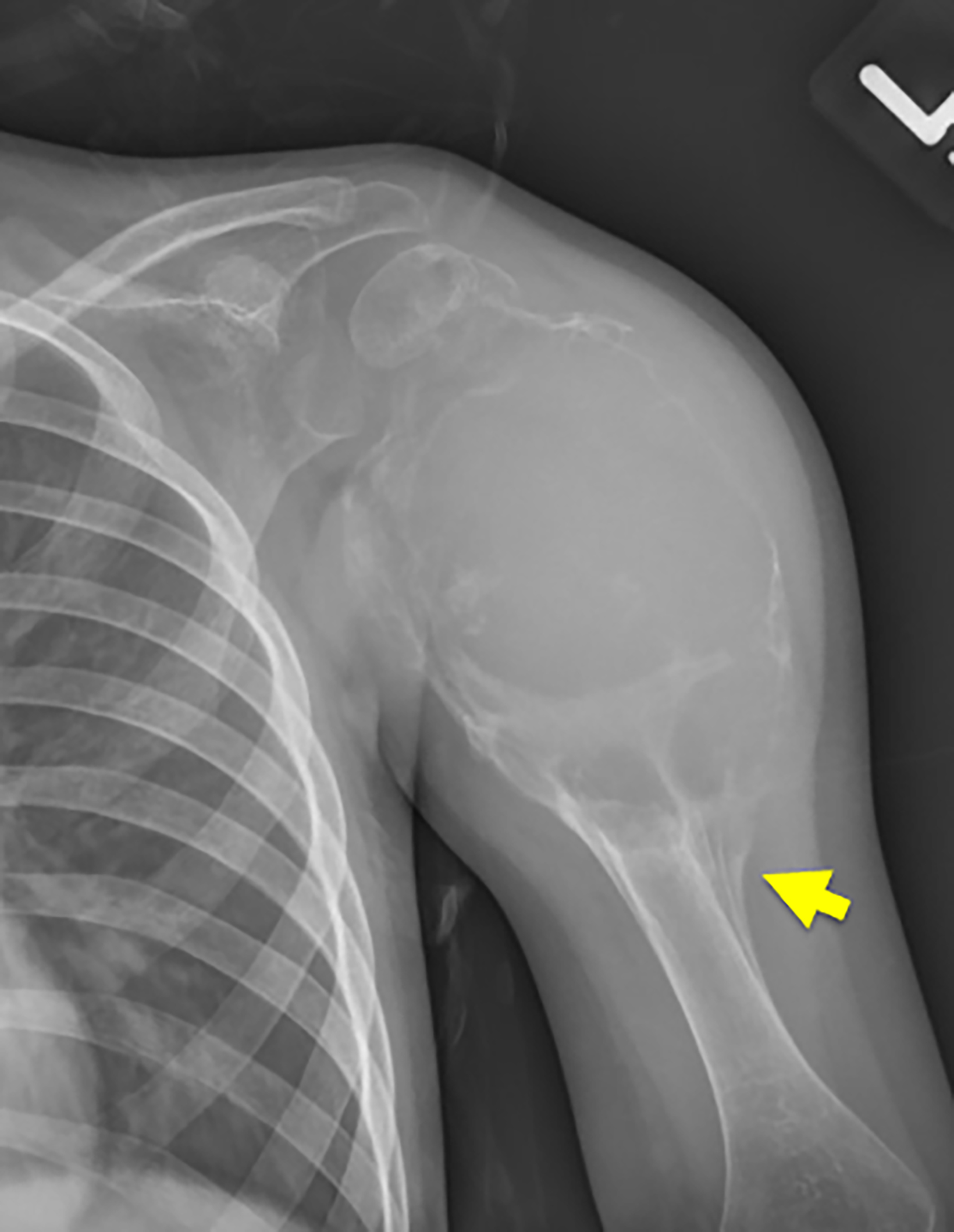
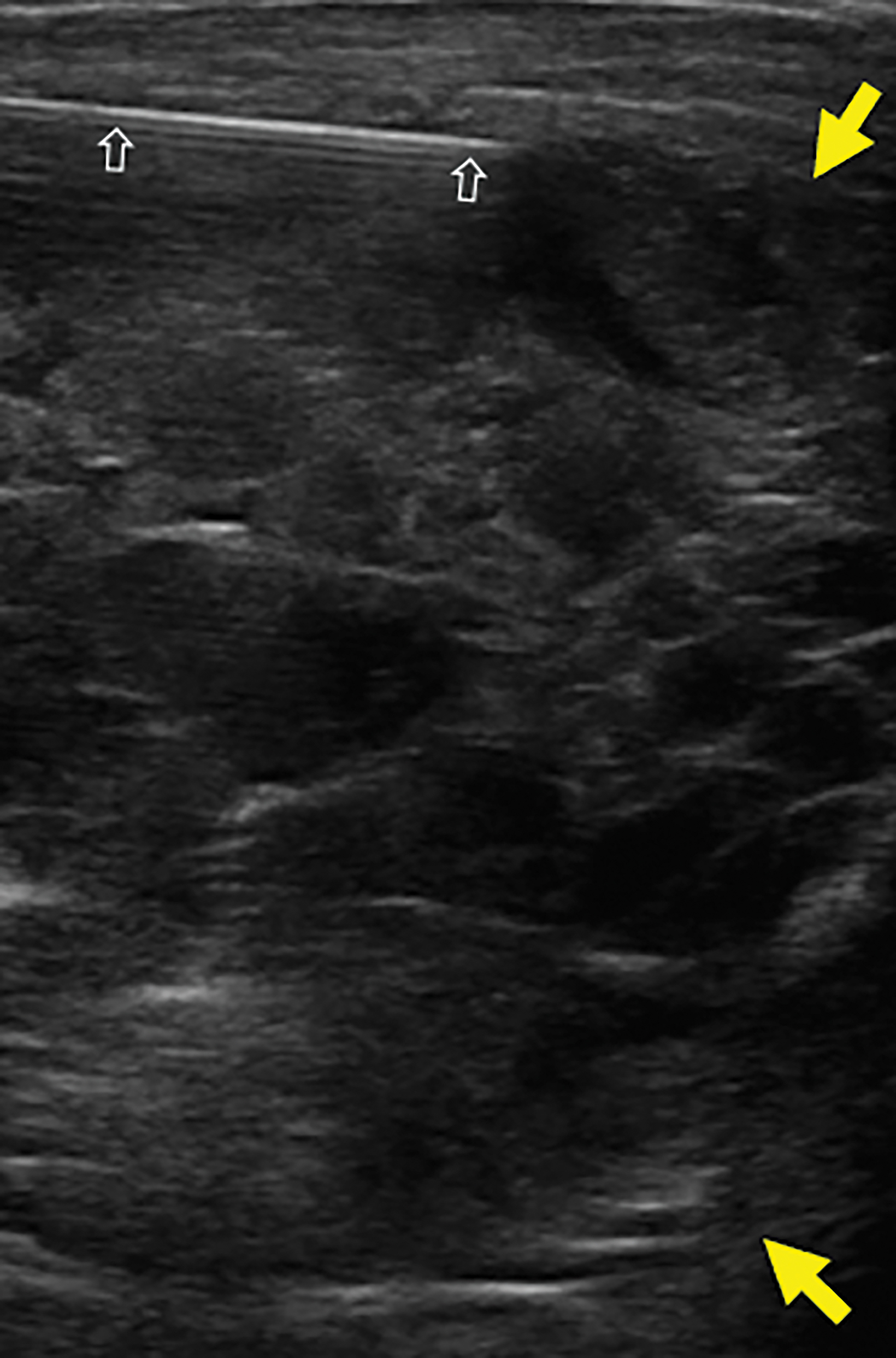
Radiographs of the shoulder demonstrated an expansile, transcortical, lucent lesion that involved the epiphysis, metaphysis, and much of the proximal diaphysis of the left humerus (Figure 1). The tumor had aggressive features with a wide zone of transition, and periosteal new bone formation, creating a Codman triangle, the triangular area of new subperiosteal bone that is created when a lesion, often a tumor, raises the periosteum away from the bone. Magnetic resonance imaging (MRI) of the left humerus showed an expansile, T2 hyperintense lesion with multiple septations and internal fluid-fluid levels (Figure 2). Ultrasound-guided percutaneous needle biopsy (Figure 3) was performed for definitive diagnosis.
Diagnosis
Telangiectatic osteosarcoma (TO). Differential diagnosis includes aneurysmal bone cyst.
Aneurysmal bone cysts can either represent a primary lesion or can occur as a secondary lesion associated with other tumors such as osteosarcoma, giant cell tumor, and chondroblastoma.
Discussion
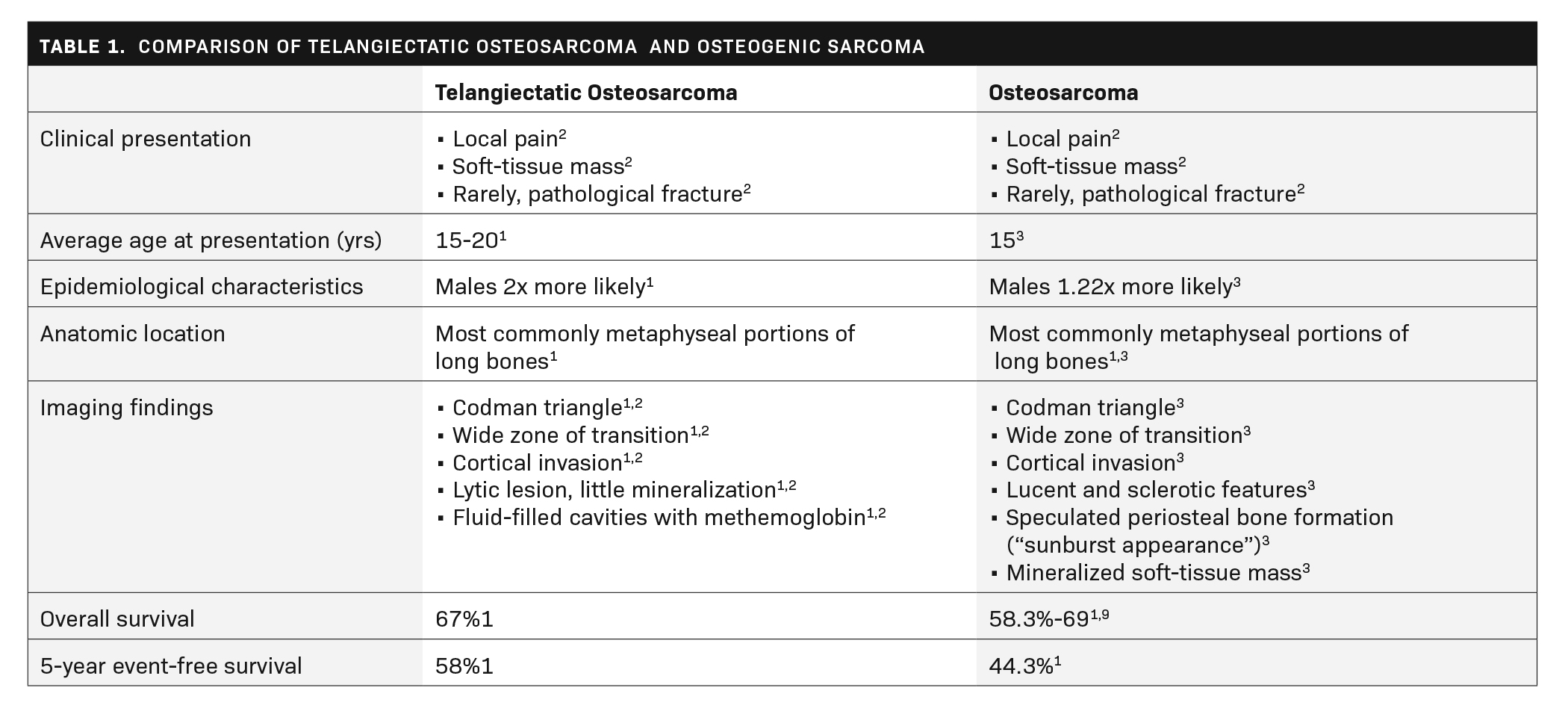
Telangiectatic osteosarcoma (TO) is an uncommon variant of osteosarcoma, occurring in 4% of osteosarcoma cases.1 Patients with TO present with pain, a soft-tissue mass, and/or a pathological fracture.2 Telangiectatic osteosarcoma occurs two times more frequently in males and the average age at diagnosis varies between 15 and 20 years.1 Over 65% of TOs develop in the metaphysis of the femur or the humerus, with the distal femur being the most common location (41.6%). Other reported sites of tumor development include the mid-femur, mid-humerus, mid-tibia, pelvis, fibula, skull, and ribs. Like that of other osteosarcomas, TO diagnosis is made by a combination of skeletal radiographs and computed tomography and/or MRI and confirmed by bone biopsy. TO and conventional osteosarcoma are compared in Table 1.
On imaging, radiographs show a lucent lesion with a destructive growth pattern involving medullary and cortical bone. TO shows little to no periosteal new bone formation, except for isolated regions near the periphery of the tumor and within the septa, where atypical stromal cells may be localized.1 This contrasts with traditional osteosarcoma, in which aggressive periosteal new bone formation is often present.4 A Codman triangle is commonly seen in TO.1
On MRI, T1 images frequently show high-signal intensity regions due to methemoglobin within hemorrhagic spaces. T2 images demonstrate multiple fluid-fluid levels owing to fluids of different densities settling within cystic cavities of the lesion.
Aneurysmal bone cysts are the most common lesions with multiple fluid-fluid levels on imaging. It can be difficult to distinguish an aneurysmal bone cyst from a TO. Other MR imaging features can help to distinguish the two entities, as a TO may have thickened and nodular internal septations owing to the viable sarcomatous cells. A soft-tissue mass may also be present.1
The histologic findings of TO are similar to those of an aneurysmal bone cyst.1 Both lesions are composed mostly of necrotic tissue and clotted blood with thin septa of atypical stromal cells throughout. While identification of malignant cells may be difficult, it is enough to rule out diagnosis of a primary aneurysmal bone cyst. TO may be categorized histologically as low-grade (mild to moderate nuclear atypia and few mitoses) or high-grade (anaplastic cells with high mitotic activity).1
Patients with TO are treated with a combination of neoadjuvant chemotherapy and surgical resection. However, TO appears to be more sensitive to neoadjuvant chemotherapy than conventional osteosarcoma, and some patients can be cured with neoadjuvant therapy alone.6
The patterns of recurrence and metastasis in TO are similar to those of conventional osteosarcoma. In a review of 87 patients with TO at 10 years of follow-up, Angellini et al found local recurrence in 11% of patients, lung metastases in 25%, and bone metastases in 3.4%.7 In conventional osteosarcoma, metastases occur in 25-30% of patients, with 85% in the lungs and 10% in the bone.8
While early reports of TO describe a more aggressive tumor with poorer outcomes than conventional osteosarcoma, more recent literature since the advent of neoadjuvant chemotherapy indicates that TO may now have a similar prognosis.3 The current five-year survival rate of TO is 60-80%, which is like that of conventional osteosarcoma, which has a five-year survival rate of 69%.9
Conclusion
Telangiectatic osteosarcoma represents a rare, malignant bone tumor, typically presenting between the ages of 15 and 20 years. TO often presents as a tender to touch, irregular mass or occasionally a pathological fracture. Notable in the differential diagnosis is aneurysmal bone cyst, from which it is important to differentiate, given that prognosis and treatment differ drastically between each. Thickening and nodularity of septa and the periphery of the lesion as seen on MRI, along with malignant, atypical stromal cells, distinguishes TO.
References
- Sangle NA, Layfield LJ. Telangiectatic osteosarcoma. Arch Pathol Lab Med. 2012 May;136(5):572-6. doi: 10.5858/arpa.2011-0204-RS. PMID: 22540307.
- Limaiem F, Kuhn J, Khaddour K. Cancer, Telangiectatic Osteosarcoma. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2019. http://www.ncbi.nlm.nih.gov/books/NBK537309/. Accessed January 14, 2020.
- Liu J, Liu S, Wang J, et al. Telangiectatic osteosarcoma: a review of literature. Onco Targets Ther. 2013;6:593-602. doi:10.2147/OTT.S41351
- Moore DD, Luu HH. Osteosarcoma. In: Peabody TD, Attar S, eds. Orthopaedic Oncology: Primary and Metastatic Tumors of the Skeletal System. Cancer Treatment and Research. Cham: Springer International Publishing; 2014:65-92. doi:10.1007/978-3-319-07323-1_4
- Keenan S, Bui-Mansfield LT. Musculoskeletal lesions with fluid-fluid level: A pictorial essay. J Comp Assist Tomog. 2006;30(3):517-524.
- Carrasco CH, Charnsangavej C, Richli WR, et al. Osteosarcoma: interventional radiology in diagnosis and management. Semin Roentgenol. 1989;24(3):193-200. doi:10.1016/0037-198X(89)90014-X
- Angelini A, Mavrogenis AF, Trovarelli G, et al. Telangiectatic osteosarcoma: a review of 87 cases. J Cancer Res Clin Oncol. 2016;142(10):2197-2207. doi:10.1007/s00432-016-2210-8
- Poletajew S, Fus L, Wasiutyński A. Current concepts on pathogenesis and biology of metastatic osteosarcoma tumors. J Orthop Tramautol Rehab. 2011;13(6):537-545. doi:10.5604/15093492.971038
- Osteosarcoma - Childhood and Adolescence: Statistics. Cancer.net. https://www.cancer.net/cancer-types/osteosarcoma-childhood-and-adolescence/statistics#:~:text=The%20overall%205%2Dyear%20survival,of%20all%20ages%20is%2077%25. Accessed July 13, 2020.
Affiliations: University of Arizona—Phoenix (Mr Nielsen); Phoenix Children’s Hospital, Phoenix, Arizona (Drs R Towbin, Schaefer, Aria); Cincinnati Children’s Hospital, Cincinnati, Ohio (Dr A Towbin)
