Anaplastic spinal cord ependymoma
Images




Anaplastic spinal cord ependymoma
Findings
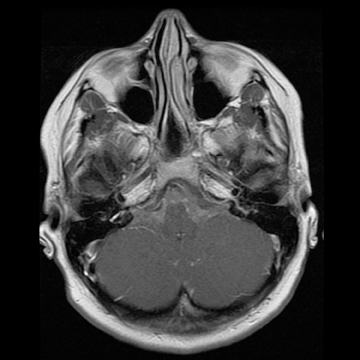
Sagittal T1-weighted and T2-weighted MR images of the lumbar spine demonstrate an enhancing intradural intramedullary mass extending from T10 to the conus medullaris (Figure 1). Sagittal T1 pre- and postcontrast (Figure 2) MR images reveal enhancement throughout the subarachnoid space of the lumbar and thoracic spine extending superiorly to the level of the cervical spine (not shown)and into the basilar cisterns (Figure 2).
Discussion
Some 90% to 95% of spinal cord neoplasms are of glial origin, with ependymomas and astrocytomas accounting for up to 70% all intramedullary neoplasms. Astrocytomas are more common in children, while ependymomas are more common in adults. The mean age at presentation for ependymoma is 38.8 years.1 However, they remain a fairly rare entity, with approximately 227 diagnosed in theUnited States each year.2
Patients most often present with neck or back pain. Sensory deficits, weakness, and bowel and bladder complaints are also common.3 The mean time from presentation to diagnosis is approximately 3 years. Generally, patients with minor preoperative deficits have better outcomes.1 Treatment usually consists of gross total resection. The role of radiation therapy (RT) is controversial, although it is usually given in cases of subtotal resection or recurrence.2 Opponents of RT argue that reoperation becomes very difficult after therapy, and that radiation myelopathy could worsen neurological deficits.3 The 5-year survival rate is approximately 82%.1
Spinal ependymomas demonstrate intense enhancement with intravenous contrast on computed tomography (CT). On T1-weightedMR imaging, ependymomas are isointense to hypointense with respect to the spinal cord, although they may rarely be hyperintense inthe setting of hemorrhage. Ependymomas are isointense to hyperintense on T2-weighted images. Approximately one-third of ependymomas will have a rim of hypointensity at the poles on T2-weighted images. This is known as the “cap sign,” which is believed to be secondary to hemorrhage. Ependymomas will also enhance on MR after contrast administration.1
Three types of cysts are associated with ependymomas. Intratumoral cysts are located within the tumor and are believed to be secondary to degeneration. They are of variable signal intensity, demonstrate peripheral enhancement, and should be surgically excised. Rostral and caudal cysts are the second type and occur above and below the tumor. They are reactive in nature, demonstrate no enhancement,and do not require excision. The third cyst type, dilation of the central canal, is likely reactive in etiology as well, from partial canal obstruction by the tumor. Again, no enhancement is seen, and the dilation resolves after tumor excision.4
The 6 main histologic types of ependymoma are cellular, papillary, tancytic, clear cell, myxopapillary, and melanotic. Cellular is the most common type, and melanotic is the least common. The distinguishing histologic characteristic is perivascular pseudorosette formation. Most ependymomas are classified as either World Health Organization grade I or II, while malignant (grade III) types are rare.1,4
Conclusion
Ependymoma is the most common intramedullary spinal cord neoplasm of glial origin in adults, although its incidence remains relatively rare. Ependymomas are treated with gross total resection, and MRI characteristics of associated cysts are important for surgical planning. The role of adjuvant therapy remains controversial.
- Koeller KK, Rosenblum RS, Morrison AL. Neoplasms of the spinal cord and filum terminale: Radiologic-pathologic correlation. Radiographics. 2000;20:1721-1749.
- Shors SM, Jones TA, Jhaveri MD, Huckman MS. Myxopapillary ependymoma of the sacrum. Radiographics. 2006;26:S111-S116.
- Hanbali F, Fourney DR, Marmor E, et al. Spinal cord ependymoma: Radical surgical resection and outcome. Neurosurgery. 2002;51:1162-1174.
- Kahan H, Sklar EML, Post JD, Bruce JH. MR characteristics of histopathologic subtypes of spinal ependymoma. AJNR Am J Neuroadiol. 1996;17:143-150.