Large Recurrent Esophageal Fibrovascular Polyp
By Flanagan JC, Nabhan A, Batz R
Case Summary
An elderly patient presented to the emergency room with worsening dysphagia to solids, neck pain, retrosternal discomfort, and 30-lb weight loss in the previous three months. The patient had a remote history of a transcervical esophageal polyp resection. Esophagogastroduodenoscopy (EGD) performed 15 years later revealed a recurrent, 20 cm esophageal polyp. The polyp was not removed at that time. The patient reported coughing up the polyp and biting it several years earlier.
Imaging Findings
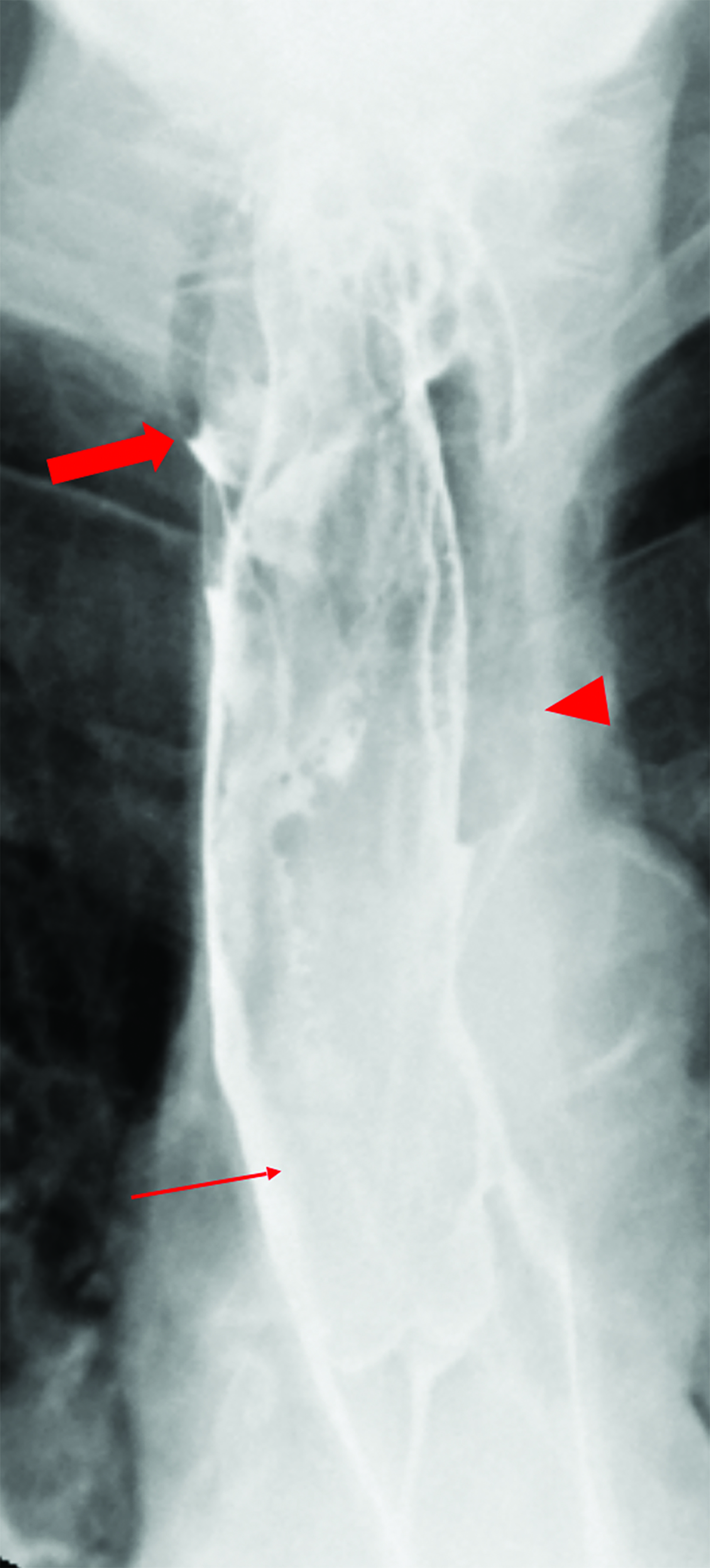
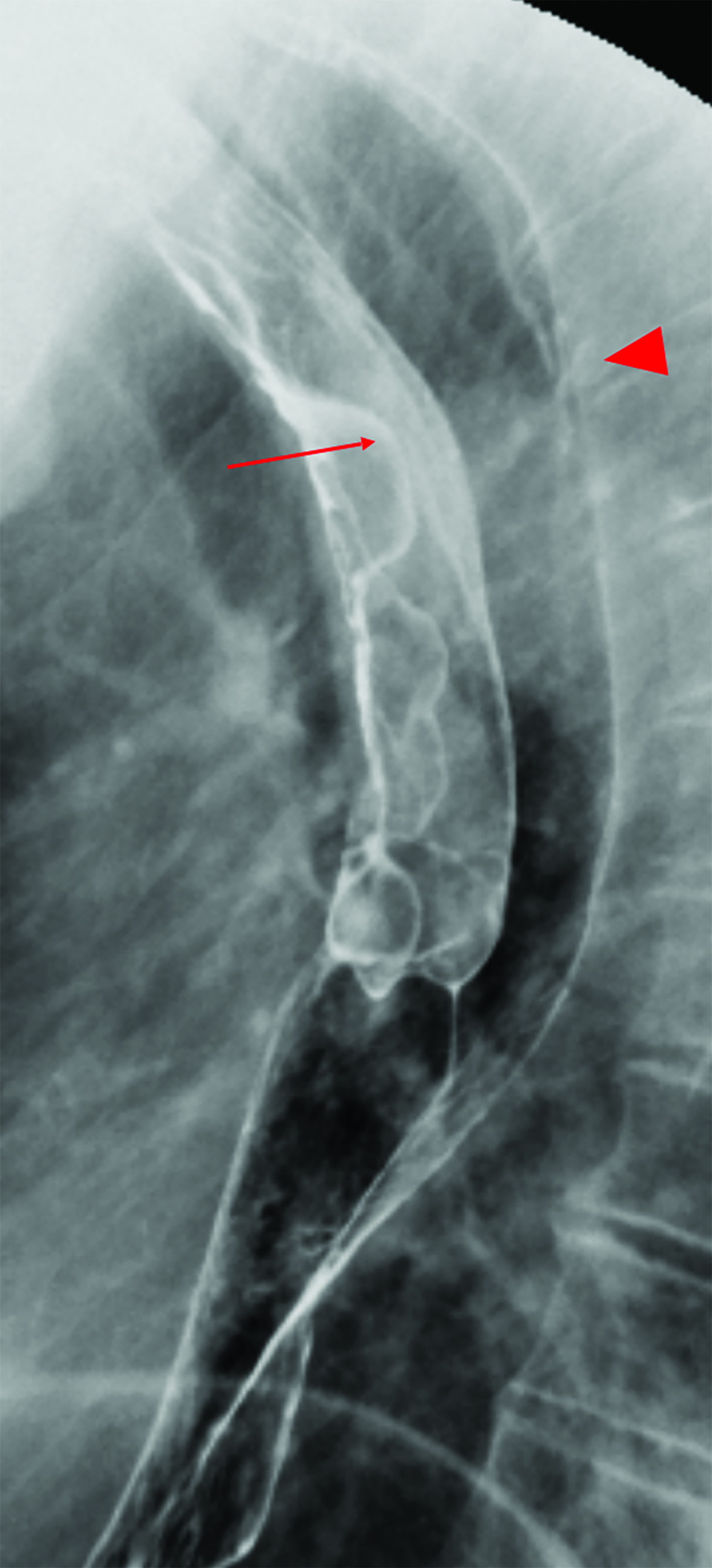
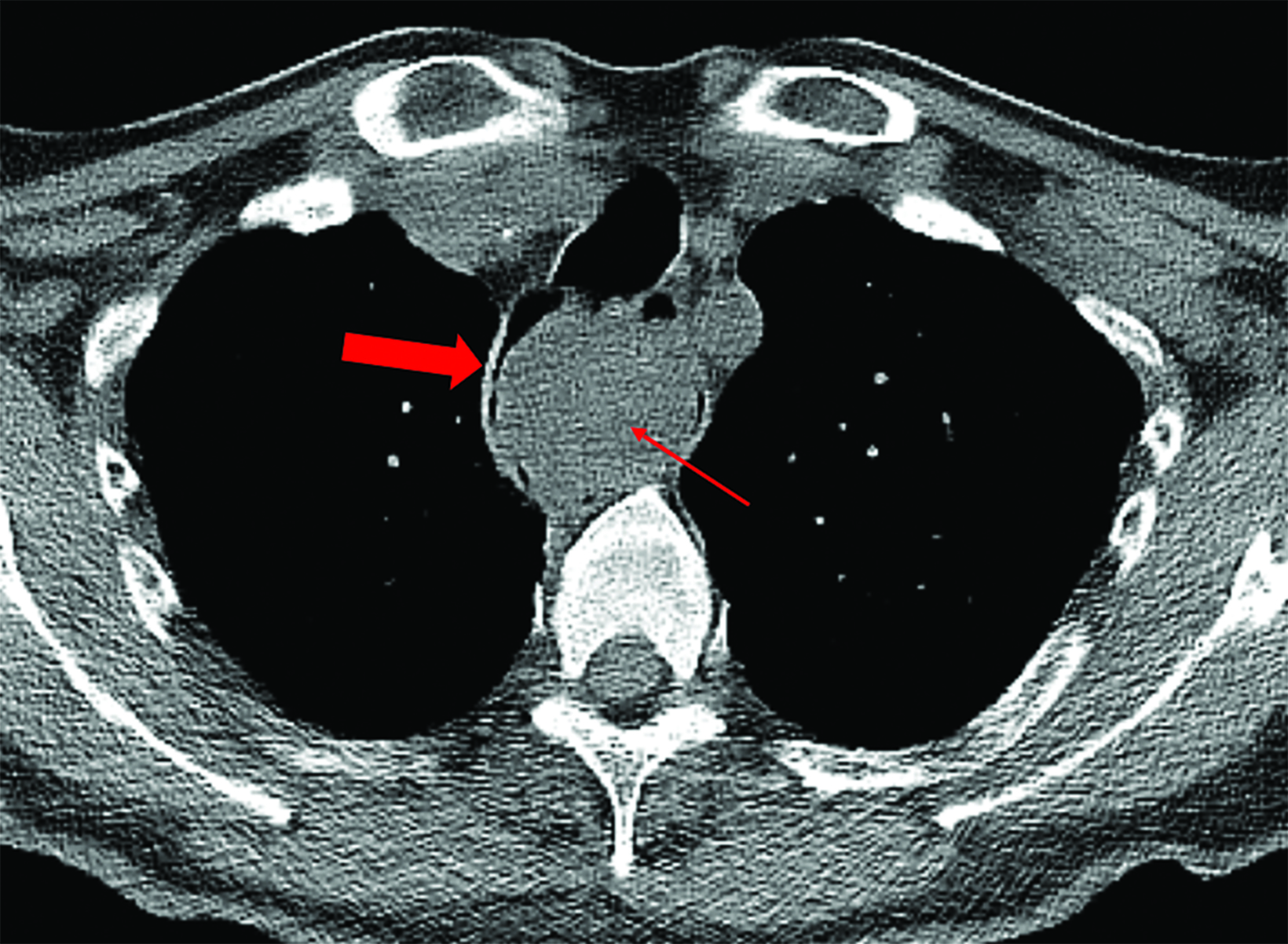
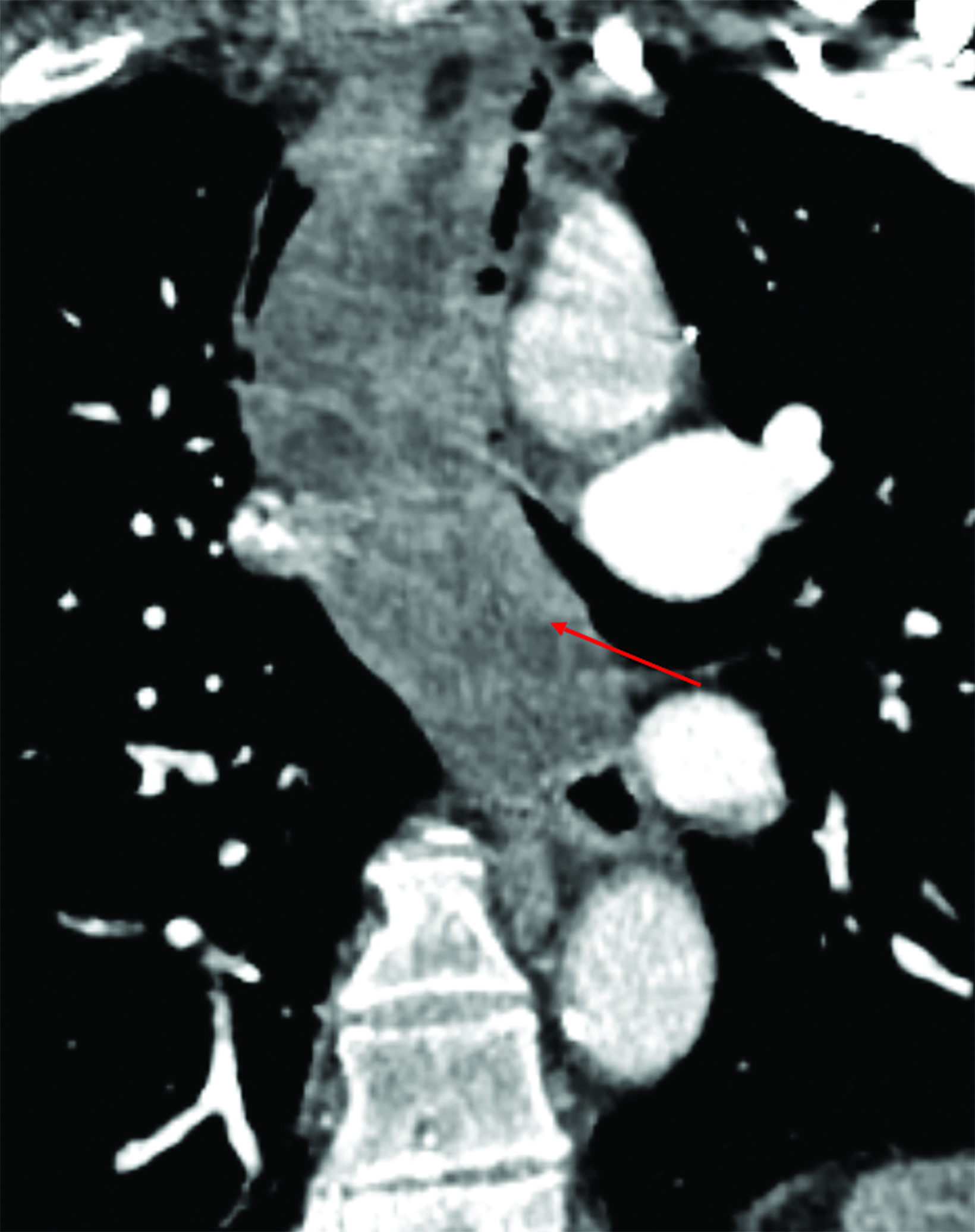
An esophagram demonstrated a large, smooth, pedunculated, mass-like filling defect arising from the cervical esophagus with extension to the lower thoracic esophagus. The polyp measured more than 50% of the transverse diameter of the esophagus. A second, but significantly smaller, mass-like filling defect was seen in the upper thoracic esophagus near the thoracic inlet (Figure 1). A subsequent noncontrast computed tomography (CT) scan of the chest demonstrated a large, polypoid, esophageal mass spanning at least 15 cm in the cervical and thoracic segments (Figure 2). The proximal segment of the mass, which almost entirely occluded the esophageal lumen, contained macroscopic fat.
Diagnosis
Recurrent esophageal fibrovascular polyp
Discussion
Fibrovascular polyps are benign, extremely rare esophageal tumors that represent fewer than 2% of all esophageal tumors.1 To date ~100 cases have been reported in the literature.2 They commonly originate near the cricopharyngeous muscle and rarely in the hypopharynx.3 The polyps comprise a mixture of lipomatous tissue among fibrous elements with an abundant network of vessels. Fibrovascular polyps are covered in normal squamous epithelium, rendering them easily missed by EGD.3,4 They are slow growing and often go undiagnosed until they are very large. Complications from fibrovascular polyps, such as bleeding or asphyxiation, can be lethal.3
Fibrovascular polyps occur predominantly in older men ranging from 60 to 70 years old with a male-to-female incidence ratio of 3:1. However, Paik, et al, reported a case of fibrovascular polyp in a 5-month-old female.2,5 The most common symptoms and signs include dysphagia to solids (87%), respiratory symptoms (25%), and regurgitation of the polyp (12%).2,3 Other nonspecific symptoms and signs include epigastric pain, odynophagia, substernal chest pain, weight loss, persistent cough, fever, anemia, and GI bleeding.1,3
Esophagram, CT, magnetic resonance imaging (MRI) and endoscopic ultrasonography (US) may be useful for diagnosis and preoperative planning. Computed tomography and MRI provide valuable information such as the polyp’s size and location, as well as the location of the pedicle attachment. Computed tomography can delineate the lipomatous and fibrous components of the polyp as well as identify feeding vessels.6 MRI is useful for identifying the precise location of the stalk, which is critical for surgical resection.2,3
Endoscopic US can determine origin of the stalk as well as the size and vascularity of the polyp.3. Endoscopic US also provides a means for a fine-needle aspiration biopsy to exclude liposarcoma, the main differential diagnosis.7,8
Surgical excision is the mainstay of treatment; the approach is determined by the individual characteristics of the polyp. Recurrence rate is high, up to 50%, especially if complete excision is not achieved.7
Conclusion
Fibrovascular polyps are extremely rare, benign tumors that may be easily missed on initial evaluation. Diagnosis is often made through various imaging studies in conjunction with the patient’s history. Fluoroscopy, CT, MRI, and endoscopic US can provide information for initial diagnosis as well as critical information for preoperative planning.
References
- Endara SA, Davalos GA, Yepez RJ, Luna DF, Corral FB, Molina GA, Cisneros WJ. Asphyxia caused by a giant fibrovascular polyp of the esophagus. ACG Case Rep J. 2019;6:1-4. doi:10.14309/crj.0000000000000126.
- Kumar A, Behari A, Kapoor VK, Verma A, Malhotra KP. Postendoscopic intraoral prolapse of a giant esophageal fibrovascular polyp. Formosan J Surg. 2016;49:165- 168. https://doi.org/10.1016/j.fjs.2016.04.004.
- Lee SY, Chan WH, Sivanandan R, Lim DTH, Wong WK. Recurrent giant fibrovascular polyp of the esophagus. World J Gastroenterol. 2009;15(29):3697-3700. doi:10.3748/ wjg.15.3697.
- Eisenberg RL. Gastrointestinal Radiology: A Pattern Approach. Fourth edition. Philadelphia, PA: Lippincott Williams & Wilkins; 2002.
- Paik HC, Han JW, Jung EK, Bae KM, Lee YH. Fibrovascular polyp of the esophagus in an infant. Yonsei Med J. 2001;42(2):264-266. doi:10.3349/ymj.2001.42.2.264.
- Madhusudhan KS, Kumar P, Dash NR. Giant fibrovascular polyp of the esophagus. J Gastrointest Surg. 2020. Published online. doi:10.1007/s11605-020-04606-6.
- Pinto A, Abastado B, Cattan P. An esophageal tumor unlike others: the fibrovascular polyp. J Visc Surg. 2019;156:271-273. doi:10.1016/j.jviscsurg.2018.11.009.
- Levine M. Radiology of the Esophagus. Philadelphia, PA: W. B. Saunders Company; 1989.
