Characterizing traumatic spinal injury at the atlantoaxial junction






The craniocervical junction functions as one joint with complex mechanics, and because half of the rotational motion in the cervical spine occurs at the atlantoaxial junction, the joint relies disproportionately on ligamentous integrity.1 Ligamentous injury may be inferred from computed tomography (CT) and radiograph findings, or demonstrated with flexion-extension radiographs. Increasingly, however, ligamentous integrity is evaluated with magnetic resonance imaging (MRI). The radiologic examination is critical for diagnosing and treating cervical spine injuries and in preventing neurologic injury. In this article, the implications of radiologic findings for spinal stability are discussed in the context of surgical treatment planning.
Atlantoaxial stability
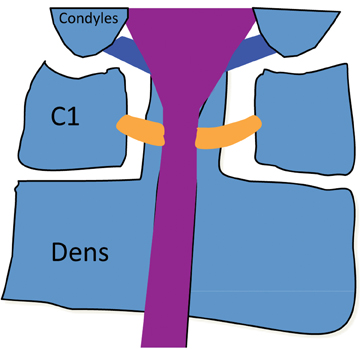
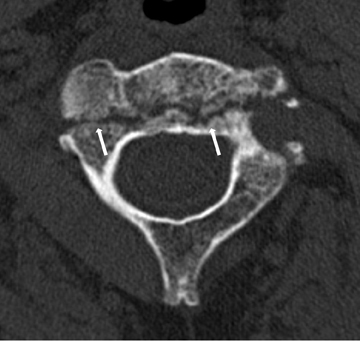
Ligaments stabilizing the atlantoaxial junction (C1-C2 joint), which are shown in Figure 1, include the tectorial membrane, the cranial extension of the posterior longitudinal ligament that limits axial distraction; the alar ligaments, which transfix the dens to the occipital condyles to restrain rotational motion; and the transverse atlantal ligament (TAL), which restricts the dens from impacting the cord in flexion.The TAL is the most important ligament, stabilizing the atlantoaxial joint against translational forces.2 The TAL runs posterior to the dens and anterior to the spinal column. Most surgeons define C1 stability based on the integrity of the TAL ligament.2 A combined lateral displacement of the C1 lateral masses > 6.9 mm in relation to the lateral border of the axis body indicates enough displacement to cause TAL rupture.3
C1 fractures
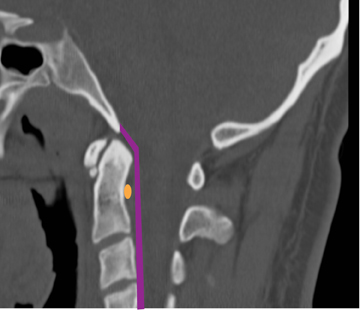
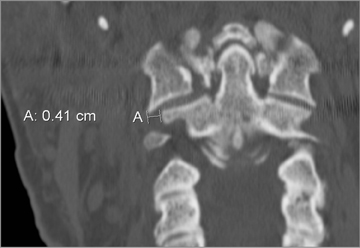
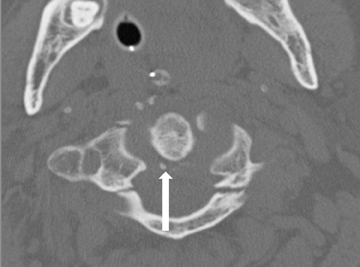
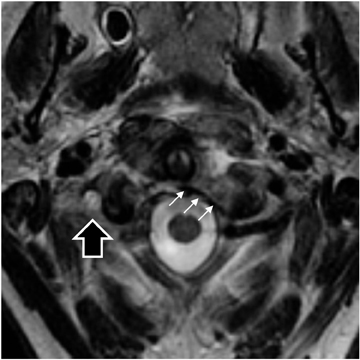
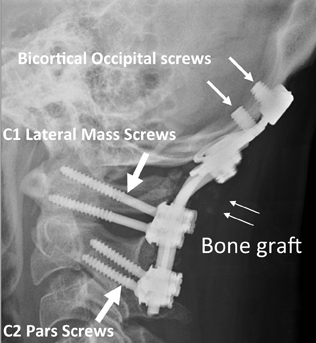
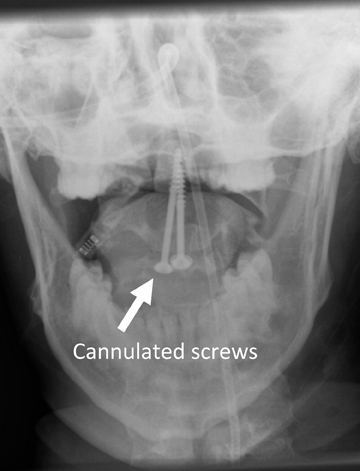
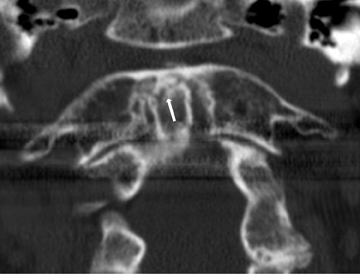
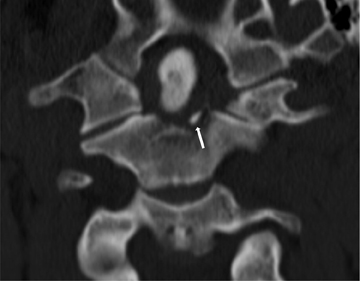
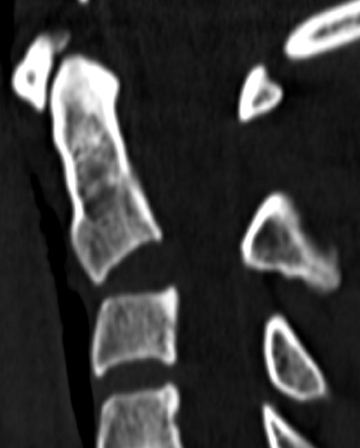
The atlas (C1) is the most “fragile” vertebra. Atlas ring fractures with > 3 parts are characterized as burst fractures, as described byJefferson.4 Stable Jefferson fractures with intact TAL (Figure 2) usually heal with immobilization for 8 to 12 weeks in a rigid cervical brace or halo. When spine trauma is treated in this fashion, serial radiographs starting within 3 weeks of the initial injury are recommended to confirm stability.5 Transverse atlantal rupture with C1 tubercle avulsion (Figure 3) is more likely to heal with nonoperative treatment than is a purely ligamentous TAL injury.6 In adults, the atlantodental interval should be within 3 mm. Anterior widening of > 5 mm in flexion suggests an incompetent TAL requiring posterior surgical instrumented fixation.5 When an atlas fracture is associated with an axis fracture, patients may undergo external immobilization to allow C1 to heal prior to surgical repair of C2. Surgical stabilization of the C1-C2 motion segment is usually achieved through posterior fixation (Figure 4), but can be achieved via a single anterior odontoid screw if the dens fracture is isolated (Figure 5). Regardless of the surgical approach, postoperative assessment of stability with radiographs is required.Vertebral artery injury during posterior craniocervical fusion, which complicates 1.3% to 4.1% of cases, is most common in cases of high-riding vertebral arteries.7
Rotary subluxation of C1 on C2
Atlantoaxial rotary subluxation in adults is rare and typically presents following MVA. The presence and extent of anterior displacement of C1 is important for treatment planning.8 However, dynamic CT for traumatic rotary subluxation of C1 on C2 is rarely indicated.9 Cervical traction in rigid cervical bracing is successful in most cases. Atlantoaxial rotary subluxation in children, an atraumatic injury, which typically occurs following upper pharyngeal infections, is a different entity.
C2 fractures and epidemiology
C2 fractures represented 18.7% of cervical spine fractures in a series of 340 axis fractures.10 Automobile collisions are the most frequent mechanism of injury, followed by falls.10,11 Together these two mechanisms account for 85% of all C2 fractures.10 Overall 34% of patients with C2 fractures have an additional spinal fracture, with C1 fractures the most common.10,12 The distribution of C2 fracture consists of odontoid 59%, hangman’s 22%, and nonodontoid, nonhangman’s fractures 20%.10 Other series have shown similar incidence of the various types of C2 fractures.11,13 Odontoid fractures have increased incidence relative to other C2 fractures with advancing age.10,12 Nonodontoid,nonhangman’s fractures, which encompass fractures of the vertebrae inferior to the dens and anterior to the pedicle, represent an important subset of fractures and differing classification systems exist.14-17 Treatment (surgery versus bracing) and surgical approach (anterior versus posterior) vary greatly depending on the anatomical location of the C2 fracture and degree of fracture displacement or ligamentous disruption. Isolated lamina and spinous process fractures at C2 are rare.16
Dens fractures
The dens fracture classification scheme, which was devised by Anderson and D’Alonzo in 1974, divides dens fractures into types I,II, and III. This system assists in determining prognosis and making treatment decisions.18 The type I fracture is rare, seen in only 2 of 49 cases in the original series and 2 of 340 in the largest series published to date.10,18 The proposed etiology is avulsion of the insertion of the alar ligament on the dens resulting in an oblique fracture of the dens tip as shown in Figure 6.18 Type I fractures heal without operative intervention.10,18 Six weeks of a rigid cervical collar is often utilized.
Type II fractures, the most common dens fracture subtype, extend through the base of the dens (Figure 6).10,11,13,18,19 Type II fractures are the most prone to nonunion with conservative management.13 Odontoid displacement > 6 mm correlates with failure of nonoperative management.10,11,13 The degree of angulation of the odontoid has also been shown to contribute to nonunion.19 Patient age > 60 years and active smoking have shown variable correlation with incidence of nonunion.10,11,13,19 Nondisplaced type II fractures are usually managed with a trial of HALO stabilization. Type II fractures with anterior or posterior translation or angulation that do not reduce in closed traction is an indication for surgical stabilization via posterior occiput-C2, posterior C1-C2 fusion, or anterior odontoid screws. Transverse atlantal-ligament injury may coexist with dens fracture and is associated with nonunion and instability.20 In the setting of TAL injury, posterior C1-C2 fusion is indicated. Anterior odontoid screw fixation does not immobilize the C1-C2 joint and is considered poorly effective for C1-C2 instability arising from TAL injury.21 Some studies have questioned this, however.22
In type III fractures, the fracture orientation is transverse through the superior aspect of the body (Figure 6). Type III fractures have a better outcome with nonoperative management than type II fractures, perhaps due to the large contact area at the fracture line with cancellous bone.10,11,13,18 First-line treatment remains 8 to 12 weeks of cervical hard collar or HALO immobilization.
The type IIA fracture subtype consists of a small bony fragment or fragments at the base of a dens fracture, as shown in Figure 6. This subtype may not heal with nonoperative management.23
Axis ring fractures
Axis ring fractures have been referred to as “hangman’s fractures” due to the similarities with fractures seen in persons executed by judicial hanging.24 However, C2 ring fractures caused by hanging also have a distraction component, which is not a major component of typical traumatic etiology of C2 ring fractures.25 Some authors reserve the term hangman’s fracture for those involving the pars interarticularis, referred to more precisely as traumatic spondylolisthesis.16 C2 ring fractures, which can be due to flexion and extension mechanisms, typically widen the central canal at the C2 level and thus rarely cause permanent paralysis.25-27 Fractures of the C2 ring are nearly always bilateral and frequently asymmetric.26
Effendi was the first to categorize these fractures using the broader definition of the C2 ring.26 This system is still in use with little modification. Francis et al have also proposed a classification system of traumatic spondylolisthesis.25 The systems are similar in that both evaluate angulation and displacement of the C2 body as a way of evaluating the competence of the supporting ligamentous structures and the stability of the fracture. The Effendi classification divides lesions into 3 types:
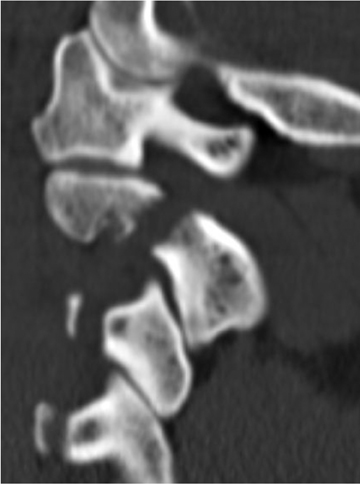
Type I: “hairline” fractures of the C2 ring with minimal C2 body displacement (Figure 7).
Type II: C2 fracture with displacement of the fragment anterior to the ring fracture with flexion, extension, or anterolisthesis (Figure 8).
Type III: C2 fracture with displacement of the anterior fragment with the C2 body in flexion as well as locked C2-C3 facet joints (Figure9).
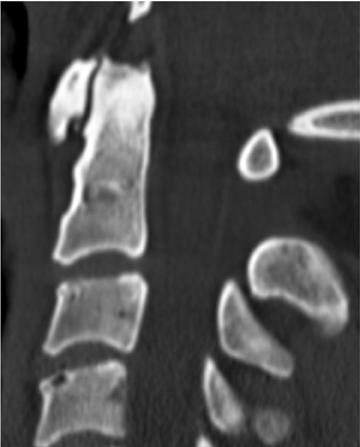
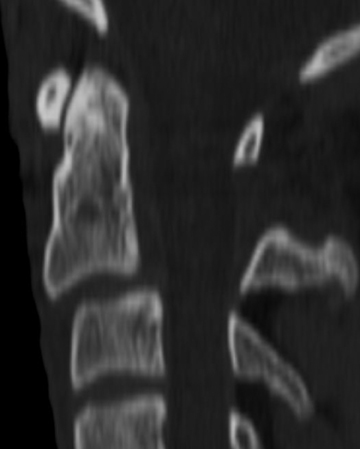
Levine and Edwards subsequently modified the Effendi classification by dividing the type II fractures into type II and type IIA.27 Type II fractures are characterized by both angulation and displacement of the C2 body; and were thought to be caused by initial hyperextension-axial load followed by flexion and compression. The flexion and compression forces resulted in the frequent (22 of 29 cases)coexistence of C3 anterosuperior body fractures.27 Type IIA injuries, which are thought to be due to flexion and distraction, have minimal displacement, but marked angulation, as shown in Figure 10. Type II fractures can be successfully reduced with traction. Type I and Type II fractures can be successfully managed in the vast majority of cases with 8 to 12 weeks of cervical bracing. Type IIA and Type III fractures are indications for surgical stabilization of the C2-C3 motion segment. When the fracture dislocation, angulation, or translation can be reduced in traction, a C2-C3 anterior cervical discectomy and fusion can be performed. Alternatively, posterior cervical fusion with C3 lateral mass screws and lag screws placed through the pars fracture into the C2 body can be utilized to achieve C2-C3 segment stability. However, the application of traction in type IIA injuries results in increased distraction and thus is to be avoided.27
Axis body fractures
While less common than dens and C2 ring fractures, C2 body fractures are not uncommon. Benzel described C2 body fractures from a variety of mechanisms. Type 1 and 2 are both vertically oriented fractures in the coronal and sagittal planes respectively.14 In type 1 fractures(Figure 11), the fracture extends through the posterior C2 vertebral body rather than the pars interarticularis extension of the hangman’s fracture.14,16 Type 2 fractures (Figure 11), which extend through the junction of the body and the pedicle with variable comminution of theC2 body, are due to axial loading, commonly following a blow to the skull vertex.14
Teardrop fractures of C2
“Teardrop” fractures are uncommon injuries of C2.28-30 All result in a triangular fracture fragment at the anteroinferior corner of the vertebral body. The 3 types of C2 teardrop fractures are the extension teardrop fracture, the hyperextension dislocation, and the flexion teardrop. Flexion teardrop injuries are more common in the lower cervical spine and are unstable injuries. They are associated with splaying of the spinous processes and posterior ligamentous injury. The hyperextension teardrop is differentiated from the hyperextension dislocation by the morphology of the avulsed fracture fragment.31 Both fragments avulse from the anteroinferior corner of the vertebral body. In the extension teardrop fracture the craniocaudal length of the fragment is greater or equal to the transverse length.The fracture fragment may be fairly large.30 Conversely, hyperextension dislocations are greater in transverse length. Flexion teardrop injuries almost always represent 3-column ligamentous injury with C2-C3 instability, requiring operative intervention. Either an anterior or posterior approach as described above can be utilized. The extension teardrop fracture of C2 is typically without cord injury and heals with nonoperative management.29,30 Conversely, hyperextension dislocation often causes central cord syndrome.31,32 Of note, the alignment of the vertebral bodies is often normal in hyperextension dislocation in spite of the injury’s seriousness and lack of stability.31
Conclusion
When stabilizing structures fail in the cervical region, devastating neurologic sequelae can occur, including high-level tetraplegia. Tetraplegia occurs in 1:10 spinal cord injuries, but results in 80% of direct medical costs of spinal cord injury. The incidence of trauma-induced spinal injury has not changed significantly over the past 3 decades, and the cervical region is the most commonly injured.33 Given the importance of the atlantoaxial joint and the frequency of cervical region injury, it is essential to recognize subtle differences in fracture patterns which convey critical information regarding spine stability.
References
- Jacobson ME, Khan SN, An HS. C1-C2 posterior fixation: Indications, technique, and results. Orthop Clin North Am. 2012;43:11-18.
- Koller H, Resch H, Tauber M, et al. A biomechanical rationale for C1-ring osteosynthesis as treatment for displaced Jefferson burst fractures with incompetency of the transverse atlantal ligament. Eur Spine J. 2010;19:1288-1298.
- Spence KF Jr, Decker S, Sell KW. Bursting atlantal fracture associated with rupture of the transverse ligament. J Bone Joint Surg Am.1970;52:543-549.
- Jefferson G. Fracture of the atlas vertebra: Report of four cases and a review of those previously recorded. Br J Surg. 1919;7:407-422.
- Canale ST, Beaty JH eds. Campbell’s Operative Orthopaedics, 11th ed. Chapter 35: Fractures, dislocations, and fracture-dislocations of the spine. Maryland Heights, MO: Mosby; 2007:1761-1830.
- Dickman CA, Greene KA, Sonntag VK. Injuries involving the transverse atlantal ligament: Classification and treatment guidelines based upon experience with 39 injuries. Neurosurgery. 1996;38:44-50.
- Lall R, Patel NJ, Resnick DK. A review of complications associated with craniocervical fusion surgery. Neurosurgery. 2010;67:1396-1402; discussion 1402-1403.
- Fielding JW, Hawkins RJ. Atlanto-axial rotatory fixation: Fixed rotatory subluxation of the atlanto-axial joint. J Bone Joint Surg Am. 1977;59:37-44.
- Bono CM, Vaccaro AR, Fehlings M, et al. Measurement techniques for upper cervical spine injuries. Spine. 2007;32:593-600.
- Greene KA, Dickman CA, Marciano FF, et al. Acute axis fractures: Analysis of management and outcome in 340 consecutive cases. Spine.1997;22:1843-1852.
- Hadley MN, Browner C, Sonntag VKH. Axis fractures: A comprehensive review of management and treatment in 107 cases. Neurosurgery. 1985;17:281-290.
- Ryan MD, Henderson JJ. The epidemiology of fractures and fracture-dislocations of the cervical spine. Injury. 1992;21:38-40.
- Hadley MN, Dickman CA, Browner C, Sonntag VK. Acute axis fractures: A review of 229 cases. J Neurosurg. 1989;71:642-647.
- Benzel EC, Hart BL, Ball PA, et al. Fractures of the C-2 vertebral body. J. Neurosurg. 1994; 81:206-212.
- Fujimura Y, Nishi Y, Kobayashi K. Classification and treatment of axis body fractures. J Orthop Trauma. 1996;10:536-540.
- Burke JT, Harris JH. Acute injuries of the axis vertebra. Skeletal Radiol. 1989;18:335-346.
- Jakim I, Sweet MBE. Transverse fracture through the body of the axis. J Bone Joint Surg Br. 1988;70:728-729.
- Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am. 1974;56:1663-1674.
- Clark CR, White AA. Fractures of the dens. A multicenter study. J Bone Joint Surg Am. 1985;67:1340-1348.
- Greene KA, Dickman CA, Marciano FF, et al. Transverse atlantal ligament disruption associated with odontoid fractures. Spine. 1994;19:2307-2314.
- Pryputniewicz DM, Hadley MN. Axis fractures. Neurosurgery. 2010;66:68-82.
- Ebraheim HA, Fow J, Xu R, Yeasting RA. The location of the pedicle and pars interarticularis in the axis. Spine. 2001;26:E34-E37.
- Hadley MN, Browner CM, Liu SS. New subtype of acute odontoid fractures (type IIA). Neurosurgery. 1988;22(1 Pt 1):67-71.
- Schneider RC, Livingston KE, Cave AJE, et al. “Hangman’s fracture” of the cervical spine. J Neurosurgery. 1965;22:141-154.
- Francis WR, Fielding JW, Hawkins RJ, et al. Traumatic spondylolisthesis of the axis. J Bone Joint Surg. 1981;63-B:313-318.
- Effendi B, Roy D, Cornish B, et al. Fractures of the ring of the axis: A classification based on the analysis of 131 cases. J Bone Joint Surg Br. 1981;63-B:319-327.
- Levine AM, Edwards CC. The management of traumatic spondylolisthesis of the axis. J Bone Joint Surg Am. 1985;67:217-226.
- Boran S, Hurson C, Gul R, et al. Functional outcome following teardrop fracture of the axis. Eur J Orthop Surg Traumatol. 2005;15:229-232.
- Korres DS, Zoubos AB, Kavadias, GC, et al. The “tear drop” (or avulsed) fracture of the anterior interior angle of the axis. Eur Spine J. 1994;3:151-154.
- Watanabe M, Sakai D, Yamamoto Y, et al. Clinical features of the extension teardrop fracture of the axis: Review of 13 cases. J Neurosurg Spine. 2011;14:710-714.
- Edeiken-Monroe B, Wagner LK, Harris JH Jr. Hyperextension dislocation of the cervical spine. AJR Am J Roentgenol. 1986;146:803-808.
- Lee JS, Harris JH, Mueller CF. The significance of prevertebral soft tissue swelling in extension teardrop fracture of the cervical spine. Emergency Radiology. 1997;4:132-139.
- Bucholz RW, Heckman JD, Court-Brown CM eds. Rockwood & Green’s Fractures in Adults. 6th edition. Philadelphia, PA: Lippincott, Williams and Wilkins; 2006.
