Common and uncommon imaging manifestations of hemophilia
Images










Dr. Yeung, Dr. Lee, Dr. Lo, Dr. Ma, and Dr. Fong are from the Radiology Department, Princess Margaret Hospital, Lai Chi Kok, Hong Kong.
Hemophilia is a lifelong disease causing significant morbidity and mortality. A wide spectrum of clinical manifestations and imaging findings is associated with this disease. Hemophilias A and B are X-linked genetic disorders; hemophilia A is due to deficiency of clotting factor VIII, while hemophilia B is due to deficiency of clotting factor IX. The incidences of hemophilia A and B are 1:5000 male and 1:25000 male, respectively.1 The most common manifestation of hemophilia is hemophilic arthropathy.2,3 The authors illustrate common and rare imaging manifestations of hemophilia, focusing on hemophilic arthropathy, soft-tissue hematoma, infected soft-tissue pseudotumor eroding into the pleural cavity, intramural gastrointestinal hematoma, intracranial hemorrhage, and deep venous thrombosis.
Common manifestation
Hemophilic arthropathy
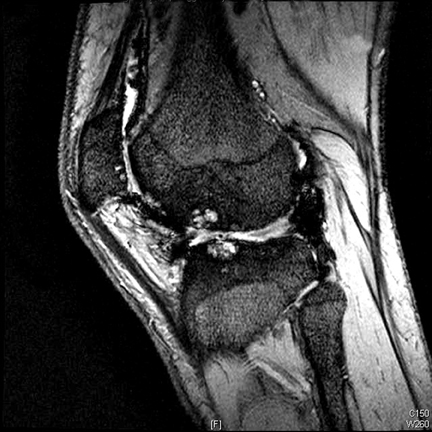
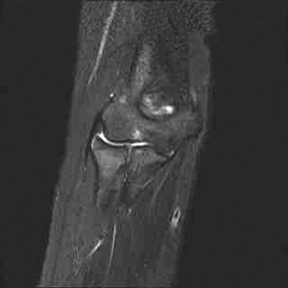
Hemophilic arthropathy is due to repeated episodes of bleeding into the synovial joints. Hemarthrosis causes a chemical reaction between blood and the synovium and cartilage, leading to pannus formation and cartilage erosion. Damage to the subchondral bone also occurs. Recurrent hyperemia of the growing joint will cause the epiphysis to enlarge and juxta-articular osteoporosis.4-6 Typical plain radiograph findings of hemophilic knee arthropathy include a widened intercondylar notch, squaring of the patella, joint space narrowing, subchondral cysts, osteoporosis, and accelerated degenerative changes.5
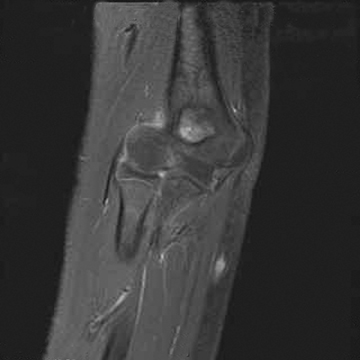
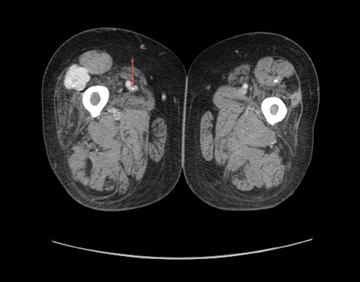
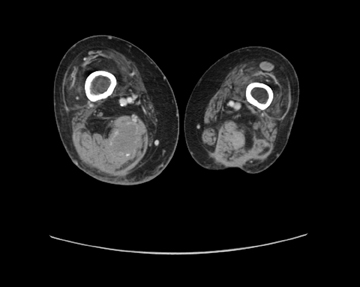
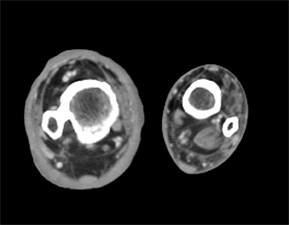
Magnetic resonance imaging (MRI) can be used to detect early erosions, subchondral cysts, bone marrow edema, joint effusion or hemorrhage, synovial hypertrophy, and concurrent ligament tears (Figures 1 and 3).
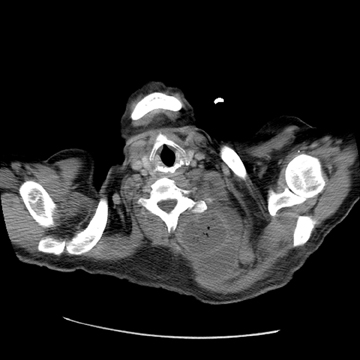
Hemophilic arthropathy most commonly affects the large joints. The frequency of joint involvement is, in descending order: the knee, elbow, ankle, hip, and shoulder.7, 8 Figures 4 through 8 provide examples of MRI and computed tomography (CT) images showing less commonly affected joints and include epiphyseal overgrowth, joint surface erosions, and osteonecrosis, another finding of hemophilic arthropathy that occurs secondarily to intra-articular bleeding.4
Less common manifestations
Soft-tissue hematoma
Intramuscular or soft-tissue hematomas account for 10% to 30% of musculoskeletal hemorrhages in hemophilia.9,10 Subcutaneous hemorrhagic nodules have also been reported by Davis et al as the presenting symptom in a 9-month-old boy with hemophilia (Figure 9).11
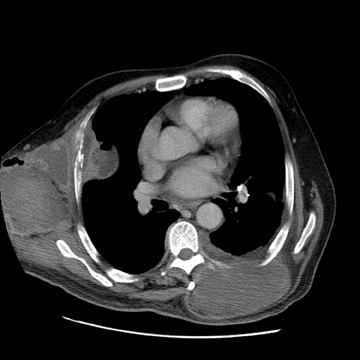
Infected soft-tissue pseudotumors
Hemophilic pseudotumors are chronic, organized, and encapsulated cystic masses that result from recurrent hemorrhage.10,12 It is estimated that 1% of severe hemophilic patients have pseudotumors.12,13 These can be osseous or soft-tissue lesions that are also able to cross anatomical boundaries.12 They are also known to cause bone erosion and pathological fractures.5 Pseudotumors may become calcified or ossified; infection is also a potential complication (Figure 10).10,14
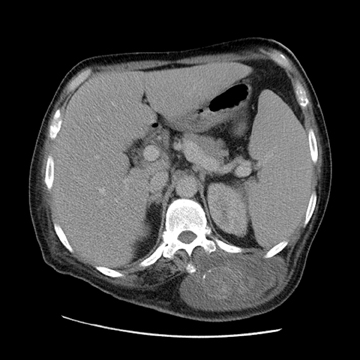
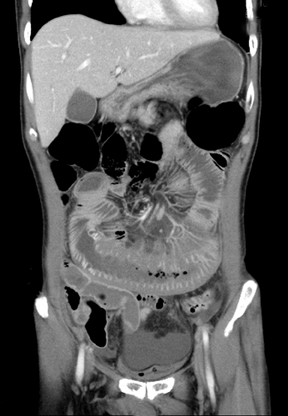
Intramural gastrointestinal hematoma
Intramural gastrointestinal hematomas have been described in patients with bleeding diastheses and those being treated with anticoagulants. They can result from serious or minor injuries, such as those caused by traffic accidents and endoscopy.15 They are most commonly found along the small bowel.15 Intramural hematomas can be the first presentation of hemophilia, as Griffin et al have presented a case of intramural gastric hematoma in a patient with undiagnosed hemophilia (Figures 11 and 12).15
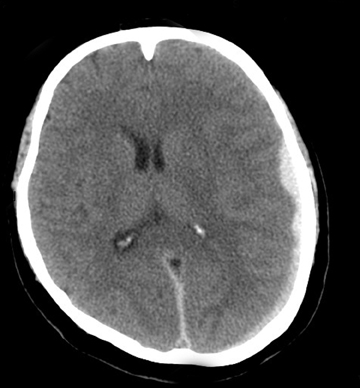
Intracranial hemorrhage
Intracranial hemorrhage is one of the most common causes of death in hemophiliacs; young patients are most often affected. It can be the initial manifestation of hemophilia. Seizures and neurological impairments are potential complications (Figures 13 and 14).16,17
Deep venous thrombosis
Venous thrombosis has been reported in hemophilia, resulting most often from indwelling catheters.18 Non-catheter-related deep vein thrombosis has also been reported by Girolami et al and Rao et al.18,19 Predisposing factors for thrombosis in hemophiliacs include the administration of coagulation factors, surgery, infection, and prothrombotic conditions, such as a Factor V Leiden mutation and Protein C or S deficiency (Figures 15 and 16).18
Conclusion
Hemophilia is a lifelong disease causing significant morbidity and mortality. A wide range of clinical manifestations and radiological findings can be seen in this disease. Bleeding diathesis and paradoxical thrombosis can occur.
References
- 1. Agaliotis DP, Zaiden RA, Ozturk S. Hemophilia in: Hematology. eMedicine. http://emedicine.medscape.com/article/210104-overview. Updated Nov. 22, 2010.
- Soreff J. Joint debridement in the treatment of advanced hemophilic knee arthropathy. Clin Orthop Relat Res. 1984;191:179-184.
- Yu W, Lin Q, Guermazi A, et al. Comparison of radiography, CT and MR imaging in detection of arthropathies in patients with hemophilia. Haemophilia. 2009;15:1090-1096.
- Kilcoyne RF. Imaging in musculoskeletal complications of hemophilia. eMedicine. http://emedicine.medscape.com/article/401842-overview. Updated Mar 21, 2008.
- Dahnert W. Radiology review manual, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2007:101-102.
- Maclachlan J, Gough-Palmer A, Hargunani R, et al. Hemophilia imaging: A review, Skeletal Radiol. 2009;38:949-957.
- Weissleder R, Wittenberg J, Harisinghani MG. Primer of diagnostic imaging. 3rd ed. St. Louis, MO: Mosby; 2003.
- Blickman JG, Vanderschueren G. Skeletal System. In: Blickman J, Parker B, Barnes P. Pediatric Radiology: The Requisites, 3rd ed. Philadelphia, PA: Mosby/ Elsevier; 2009:157-204.
- Beeton K, Alltree J, Cornwall J. Rehabilitation of muscle dysfunction in hemophilia. Haemophilia. 1990;4:532-537.
- D’Young A I. Conservative physiotherapeutic management of chronic haematomata and haemophilic pseudotumours: Case study and comparison to historical management. Haemophilia. 2009:15;253-260.
- Davis G, Butler DF, Greene J Jr. Hemorrhagic subcutaneous nodules: An initial clinical sign of hemophilia A. Pediatr Dermatol. 2007;24: 121-124.
- Park J S, Ryu K N. Hemophilic pseudotumor involving the musculoskeletal system: Spectrum of radiologic findings. AJR Am J Roentgenol. 2004;183:55-61.
- Ahlberg AK. On the natural history of hemophilic pseudotumor. J Bone Joint Surg Am. 1975; 57:1133-1136.
- Auger MJ, Critchley M, McVerry BA. Unusual presentation of a large infected hemophiliac pseudotumor in an autologous indium-111 WBC scan. Clin Nucl Med. 1986;11:568-569.
- Griffin PH, Schnure FW, Chopra S, et al. Intramural gastrointestinal hemorrhage. J Clin Gastroenterol. 1986;8:389-394.
- Rodriguez V, Schmidt KA, Slaby JA, Pruthi PK. Intracranial haemorrhage as initial presentation of severe haemophilia B: Case report and review of Mayo Clinic Comprehensive Hemophilia Center experience. Haemophilia. 2005; 11:73-77.
- Nelson MD Jr, Maeder MA, Usner D, et al. The Hemophilia Growth and Development Study-Prevalence and incidence of intracranial haemorrhage in a population of children with haemophilia. Haemophilia. 1999;5:306-312.
- Rao AN, Kumar R, Arteaga GM, et al. Non-catheter-related internal jugular vein thrombosis in a patient with severe haemophilia A. Haemophilia. 2009;15:1339-1340.
- 1Girolami A, Scandellari R, Zanon E, et al. Non-catheter-associated venous thrombosis in hemophilia A and B. A critical review of all reported cases. J Thromb Thrombolysis. 2006; 21:279-284.