Complete gastroesophageal obstruction by food bolus
By KO Kragha

CASE SUMMARY
A 54-year-old male with history of esophageal varices, alcoholic cirrhosis and alcohol abuse presented with inability to swallow that started on the day of presentation to the emergency room. The patient woke up at 3 a.m. and ate steak, then went back to sleep. Shortly there after, he woke up to drink water but was unable to swallow the water and had not been able to swallow since then. The patient was coughing up yellow phlegm frequently. He had his last drink of alcohol before eating the steak and about 12 hours prior to presentation to the emergency room. His serum alcohol toxicology screen was 120 mg/dl. The patient was tremulous at presentation to the emergency room. The patient reported no blood in sputum but reported bright red blood per rectum with history of hemorrhoids and blood in urine one month ago, which had turned dark ever since.
IMAGING FINDINGS
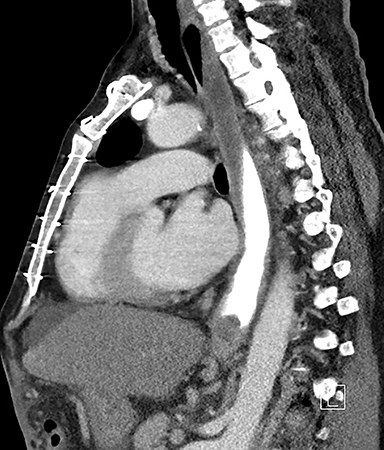
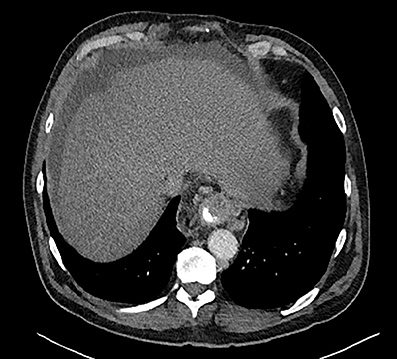
Computed tomography (CT) showed paraesophageal fluid and varices, liver cirrhosis, splenectomy and multiple splenules. There is a dilated upper and mid esophagus with air fluid level, paraesophageal fluid and varices; mid to lower esophagus was dilated with fluid contrast level to the distal esophagus, approaching the gastroesophageal junction. There was an intraluminal filling defect in the distal esophagus which progressed to terminate in complete obstruction. No contrast was seen in the gastrointestinal tract distal to the filling defect (Figures 1 and 2).
Esophagogastroduodenoscopy (EGD) showed the patient had prior food bolus impaction now presenting with food impaction. The food bolus was encountered and attempts to remove it with Roth net, tripod extension were initially unsuccessful. An over tube was placed and the bolus was removed in piecemeal fashion, using suction cup, Roth net, and tripod extension. The bolus was completely removed. The procedure was difficult and took an hour to complete. There were no complications. The food bolus was found in the lower third of the esophagus lumen. A Schiatzki’s ring was found in the gastroesophageal junction. Protruding and bleeding varices were seen in the lower third esophagus. Gastric mucosa showed diffuse erythema and friability. The duodenum was normal. The above findings were compatible with portal hypertensive gastropathy.
DIAGNOSIS
Complete gastroesophageal obstruction by food bolus
DISCUSSION
Esophageal food bolus impaction is a common gastrointestinal emergency with esophageal food impaction the third most common non-biliary endoscopic emergency after upper and lower gastrointestinal hemorrhage. Food bolus is the most common impacted foreign body, particularly in adults, but other objects include coins, toys, bones, batteries. The annual incidence is about 11 to 13 cases per 100,000 per year, with the male: female ratio of 1.7:1, and resulting in up to 1,500 deaths per year. Esophageal food impaction is more common in older adults and rare in children. Most food impaction in adults occurs as a result of underlying esophageal anatomic pathology. The use of dentures may contribute to esophageal food impaction. Presentation includes chest or throat discomfort, dysphagia or odynophagia, and difficulty managing oral secretions, such as choking and drooling, refusal to eat, vomiting, wheezing, blood-stained saliva, or respiratory distress, heartburn, cough, abdominal pain. Predisposition is prior episodes of sensation of food getting stuck in the esophagus and previous endoscopic intervention for disimpaction of esophageal food impaction, gastroesophageal reflux in infancy, and asthma. Esophageal intramural pseudodiverticulosis and nutcracker esophagus are rare causes of food impaction. Eosinophilic esophagitis, which is associated with food impaction in adults, is now the leading cause of food impaction in patients presenting to the emergency room, accounting for more than 50 percent of episodes. Eosinophilic esophagitis is an inflammatory disorder of the esophagus, which decreases the ability of the esophagus to stretch and accommodate swallowed foods, presenting with mainly dysphagia and food stuck in the esophagus and other less common symptoms including heartburn and chest pain. Eosinophilic esophagitis, which is seen in childhood and young adults with men more commonly affected than women, has the following characteristics: (1) symptoms, including but not restricted to, food impaction and dysphagia; (2) biopsy specimen showing more than 15 eosinophils/high-power field; and (3) other disorders associated with similar clinical, histological, or endoscopic features have been excluded. Eosinophilic esophagitis is a T-helper (Th) 2-type immune/antigen mediated or atopic chronic relapsing disease involving ingested and inhaled allergens with remodeling of the esophagus resulting in dense eosinophilic infiltrate, esophageal dysfunction, and bolus impaction with majority of the patients having concurrent allergic rhinitis, asthma, eczema, and/or history of atopy. Characteristic endoscopic features are linear furrows, corrugated mucosal rings, and white papules, and narrowed esophageal lumen. Food bolus impaction which has increased over the last 15 years is associated with an increased prevalence of eosinophilic esophagitis and a reduction in age of presentation and peptic-related strictures.1-8
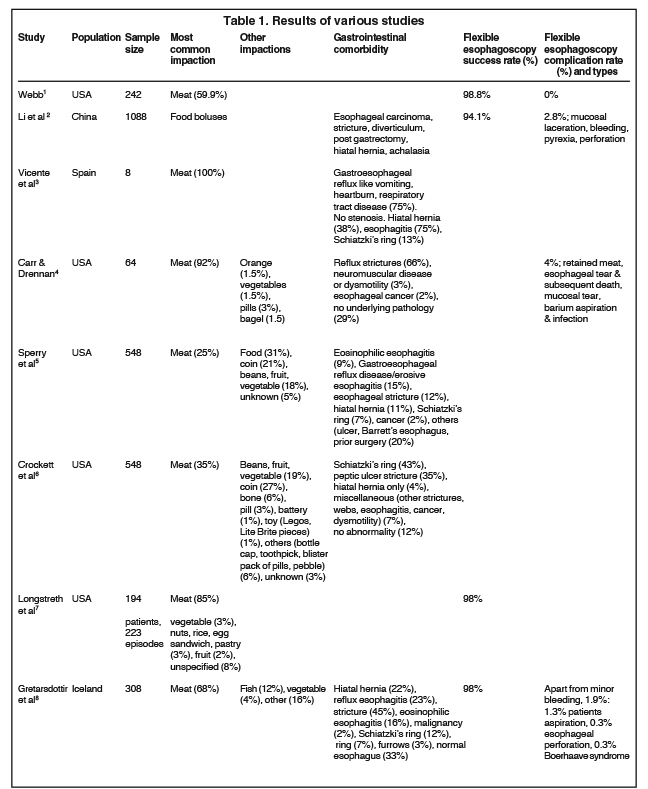
This is a case of complete esophageal obstruction by steak that may mimic cancer in the absence of known history. This case describes esophageal food bolus impaction and its CT and EGD findings. To the best of my knowledge, the CT imaging of complete esophageal obstruction by food impaction or bolus has not been previously reported. Table 1 shows the results of various studies. The patient had a classic presentation of esophageal food bolus impaction. This is a 54-year-old male who ate steak and shortly thereafter was unable to swallow water and was coughing. However, the patient had no blood in sputum, a finding sometimes seen in esophageal food impaction. Esophageal food impaction may be complete obstruction (83%) and partial obstruction (17%). Esophageal food impaction is more common in males (55-59%) than females (41-45%) with age range of 3 months to 99 years. There is bimodal age distribution, peaking in children (age 1 to 5 years) and older adults (age 40 to 80 years). The foreign bodies are located in the pharynx (1 to 16%), esophagus (53 to 75%), stomach (8 to 41%), and small bowel (1 to 5%). and surgical anastomosis (1%). Gastrointestinal comorbidities in esophageal food impaction include gastrointestinal reflux disease, esophageal strictures, Schatzki ring, achalasia, malignancy, eosinophilic esophagitis, diverticulum, post gastrectomy, hiatal hernia, neuromuscular disease or dysmotility, esophageal cancer, Barrett’s changes, dysplasia, and no underlying pathology (29%); this last group may have normal esophagus but swallowed too large a piece of meat, confounded by other factors such as alcoholism. This patient had a Schatzki ring and alcohol abuse. Esophageal food impaction can be associated with serious consequences, such as caustic injury, esophageal perforation, aortoesophageal fistula formation. Oral radiographic contrast studies should be avoided in esophageal food impaction because of the risk of aspiration and interference with endoscopy. However, this patient had no complications from the esophageal food impaction and oral contrast administration for CT scan.1,5-7 However, this patient had no complications from the esophageal food impaction and oral contrast administration for CT scan.
EGD treatment of food bolus impaction
The majority of ingested foreign bodies (80 to 90%) pass spontaneously. About 10 to 20% of ingested foreign bodies require nonsurgical intervention and less than 1% requires surgical intervention. However, in intentional ingestion, the rate of nonsurgical intervention may be as high as 63 to 76% and surgical intervention, 12 to 16%. The initial management of esophageal food impaction is assessment of the patient’s ventilation and airway. Proximal esophageal foreign body ingestion may require general anesthesia and intubation. Intervention depends on the time since ingestion, anatomic location of the ingested object, patient’s age and the size, shape, content of the ingested foreign body. Majority of esophageal food impaction can be successfully treated with flexible endoscopes under conscious sedation. Endoscopic treatment includes food extraction and push of the bolus into the stomach. Extraction may involve piecemeal removal or en bloc removal by various grasping devices. Retrieval devices include rat-tooth and alligator forceps, polypectomy snares, polyp graspers, Dormier baskets, retrieval nets, magnetic probes, and friction-fit adaptors or banding caps. An over tube facilitates passage of the endoscope and protects the airway and during removal of multiple objects or during piecemeal clearance of food impaction, and also protects the esophageal mucosa from lacerations during retrieval of sharp objects.1, 3, 5-7
Complications of EGD treatment of food bolus impaction
The complications of endoscopy are rare, occurring in 1 to 6% of cases. The most common complication is unsuccessful extraction requiring a second extraction or different treatment. Other complications include small distal esophageal lacerations with oozing of blood, esophageal mucosa tear during dilation but no contrast extravasation on follow up barium swallow and managed conservatively, esophageal tear at the gastroesophageal junction and subsequent death in an elderly patient, aspirated barium and subsequent infection, atrial fibrillation, bronchospasm.6, 7
Other treatment modalities of food bolus impaction
Other techniques include suctioning the bolus into a ligator adaptor on an endoscope tip, using retrieval net, cooking the center of the bolus with an Nd:YAG laser, performing blind bougienage with a Maloney dilator, and suctioning the bolus into a modified gastric lavage tube. Laryngoscopy and rigid endoscopy can be used for proximal impactions, pediatric cases, and those who fail intervention via flexible upper endoscopy.7 Several pharmacologic agents including hyoscine butyl bromide (buscopan), glucagon, nitrates, calcium channel blockers, and papaveretum and nonmedicinal agents such as water, effervescent crystals, papain and fresh pineapple juice have been used in the treatment of esophageal food impaction with variable success rate. Proteolytic enzymes such as papain may cause of esophageal perforation, erosion, hypernatremia, hemorrhagic pulmonary edema and aspiration pneumonitis. Glucagon may cause vomiting airway obstruction and potential risk of esophageal perforation. Effervescent crystals may cause laryngeal aspiration, vomiting and mucosal tear. The overwhelming conclusion is that there is no strong evidence suggesting any of these agents are effective in dislodging food bolus obstruction.9
Algorithm for management of esophageal food bolus impaction
If esophageal food impaction is suspected and the patient can swallow saliva, then perform barium swallow with effervescent crystals and glucagon. If there is successful disimpaction of esophageal food impaction, then arrange endoscopy as outpatient. If the patient cannot swallow saliva, then take the patient to surgery under general anesthesia and endotracheal tube and attempt extraction of esophageal food impaction with flexible esophagoscopy under fluoroscopy. If successful, may obtain biopsy and dilate esophagus as clinically indicated. If not successful, try balloon for retrograde extraction or under fluoroscopy pass guidewire around esophageal food impaction, dilate and push into stomach. If this is still unsuccessful, then open extraction.4
Recommendations for management of ingested foreign bodies and food impactions
The following are recommendations for the management of ingested for foreign bodies and food impactions9:
- Avoid contrast radiologic examinations before removal of foreign body.
- Otorhinolaryngology consultation for foreign bodies at or above the cricopharyngeus muscle level.
- Emergent removal of esophageal bolus impactions and foreign bodies in complete esophageal obstruction.
- Acceptable methods for the management of esophageal food impactions include en bloc removal, piecemeal removal, and gentle push technique.
- Endoscopic removal of all objects larger than 2.5 cm from the stomach.
- Endoscopic removal of sharp-pointed objects or objects larger than 6 cm in the proximal duodenum.
- Emergent removal of disk batteries from the esophagus.
- Removal of all magnets within endoscopic reach. For magnets beyond endoscopic reach, close observation and surgical consultation.
- Observe patients with coins in the esophagus who are asymptomatic but remove coins if there is no spontaneous passage within 24 hours of coin ingestion.
- No endoscopic removal of drug- containing packets.
CONCLUSION
Esophageal food impaction is a common problem in older men, mostly caused by meat. An anatomic abnormality such as a Schiatzki’s ring or peptic ulcer stricture is often present. The majority of ingested foreign bodies will pass spontaneously. However, the minority of the cases which require intervention can be safely treated with flexible esophagoscopy, often by pushing the impacted food bolus into the stomach or piecemeal extraction of the impacted food bolus.
REFERENCES
- Webb WA. Management of foreign bodies of the upper gastrointestinal tract: update. Gastrointestinal Endoscopy. 1995;41:39-51.
- Li ZS, Sun ZX, Zou DW, et al. Endoscopic management of foreign bodies in the upper-GI tract: experience with 1088 cases in china. Gastrointestinal Endoscopy. 2006;64:485-492.
- Vicente Y, Hernandez-Peredo G, Molina M, et al. Acute food bolus impaction without stricture in children with gastroesophageal reflux. J Pediatric Surg. 2001;36:1397-1400.
- Carr JA Drennan JA. Food bolus impaction secondary to reflux strictures: a rural surgical experience. J Amer Coll Surg. 2008;207:745-750.
- Sperry SLW, Crockett SD, Miller CB, et al. Esophageal foreign body impactions: epidemiology, time trends, and the impact of the increasing prevalence of eosinophilic esophagitis. Gastrointestinal Endoscopy. 2011;74:985-991.
- Crockett SD, Sperry SLW, Miller CB, et al. Emergency care of esophageal foreign body impactions: timing, treatment modalities, and resource utilization. Dis Esophagus. 2013;26:105-112.
- Longstreth GF, Longstreth KJ, Yao JF. Esophageal food impaction: epidemiology and therapy. A retrospective study, observational study. Gastrointestinal Endoscopy. 2001;53:193-198.
- Gretarsdottir HM, Jonasson JG, Bjornsson ES. Etiology and management of esophageal food impaction: a population based study. Scandinavian J Gastroenterol. 2015;50:513-518.
- American Society for Gastrointestinal Endoscopy. Guideline for the management of ingested foreign bodies and food impactions. Gastrointestinal Endoscopy. 2011;73:1085-1091.
