Computed Tomography: An Optimal Modality for the Detection of Nontraumatic Intraperitoneal and Retroperitoneal Hemorrhage
By Okpara R, Shiralkar KG, Matta EJ, Chua SS











Acute nontraumatic abdominopelvic hemorrhage is a medical emergency that requires prompt diagnosis; imaging is often crucial to localize the source and extent of bleeding. Ultrasound may be useful as an initial screening tool but is not sensitive enough to detect subtle injuries or small bleeds.1 Computed tomography (CT) is most commonly used and typically the best option in emergency settings, owing to its reliability, speed, and typical proximity to the emergency department.2 Indeed, the modality has been shown to be superior to other imaging modalities in detecting intra-abdominal bleeding, particularly when the bleeding rate is low.1
Signs of acute hemorrhage on CT scans include the triangle sign of mesenteric bleeding, sentinel clot, mesenteric/hyperdense fluid, and active arterial extravasation. These findings may allow radiologists to localize the source and site of intraperitoneal hemorrhage, which can aid management.1,2 This review article focuses on common sources of nontraumatic hemoperitoneum while highlighting salient CT findings.
Appearance of Hemorrhage
The CT appearance of hemorrhage depends on the location, age, and extent of the bleeding. On unenhanced images, bleeding attenuates at 35-45 Hounsfield units (HU) in the hyperacute stage due to high protein concentration.3 In the next few hours, the attenuation will increase to over 60 HU as hemoglobin concentration increases in the acute stage. This will subsequently decrease over time. Typically, blood will tend to clot near the bleeding site (the “sentinel clot sign”) further pinpointing the hemorrhage location.2 Over time, the clot will shrink with progressive lysis of hemoglobin and liquefaction. On contrast-enhanced CT, a site of active bleeding may demonstrate higher attenuation ranging from 85 to 300 HU.2 Such high attenuation suggests contrast extravasation and may indicate the need for emergency embolization or surgery.
Tumor-related Causes of Hemorrhage
Absent a history of anticoagulant use or trauma, spontaneous hemoperitoneum is rare. In these cases, excluding rupture by neoplasm or vasculopathy is essential.4 While uncommon, a primary or metastatic tumor can rupture and bleed into the peritoneal or retroperitoneal cavity with devastating effects.
Renal Cell Carcinoma
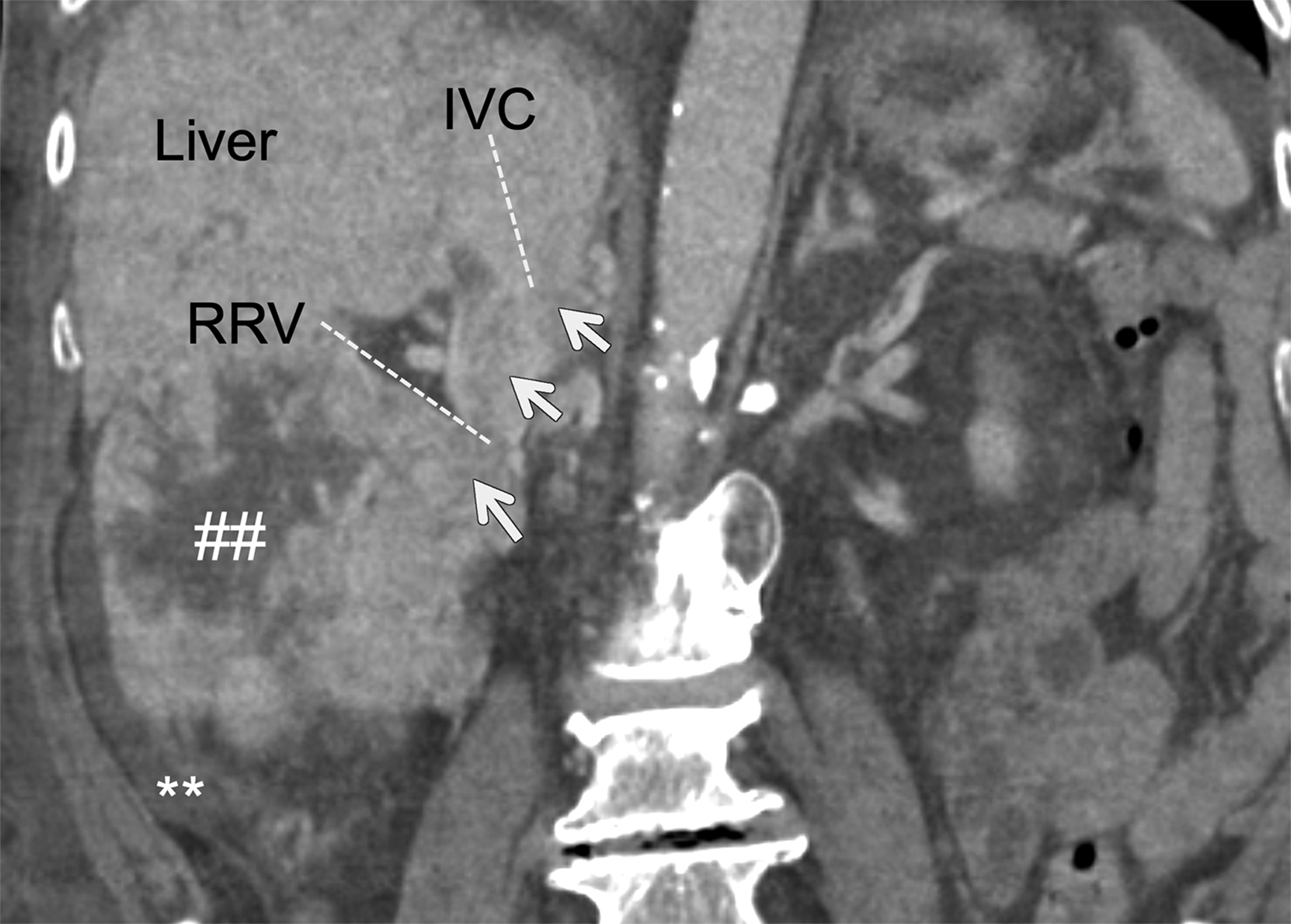
Accounting for 3% of overall adult malignancies and 90% of neoplasms derived from the kidneys, renal cell carcinoma (RCC) is the
most common renal cancer in adults.5,6 Spontaneous hemorrhaging of these tumors more commonly accompanies the clear cell and collecting duct subtypes and typically presents with hematuria, pain, and a palpable abdominal mass.7 On contrast-enhanced CT images, RCC is suggested by a solid, enhancing, and often necrotic mass (Figure 1).3 Spontaneous rupture of RCC is rare; however, the condition is life-threatening and prompt imaging and intervention may be necessary.8
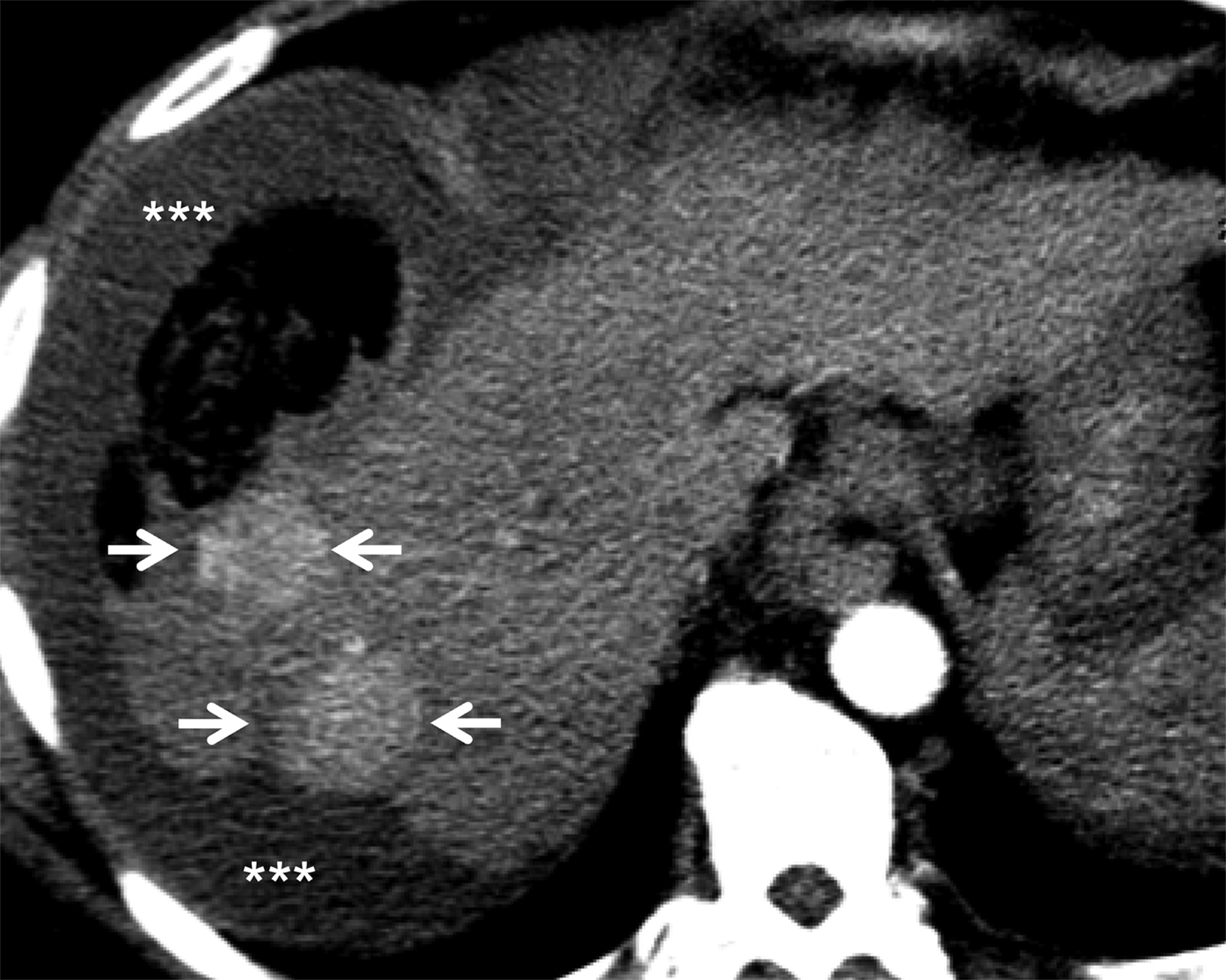
Angiomyolipoma
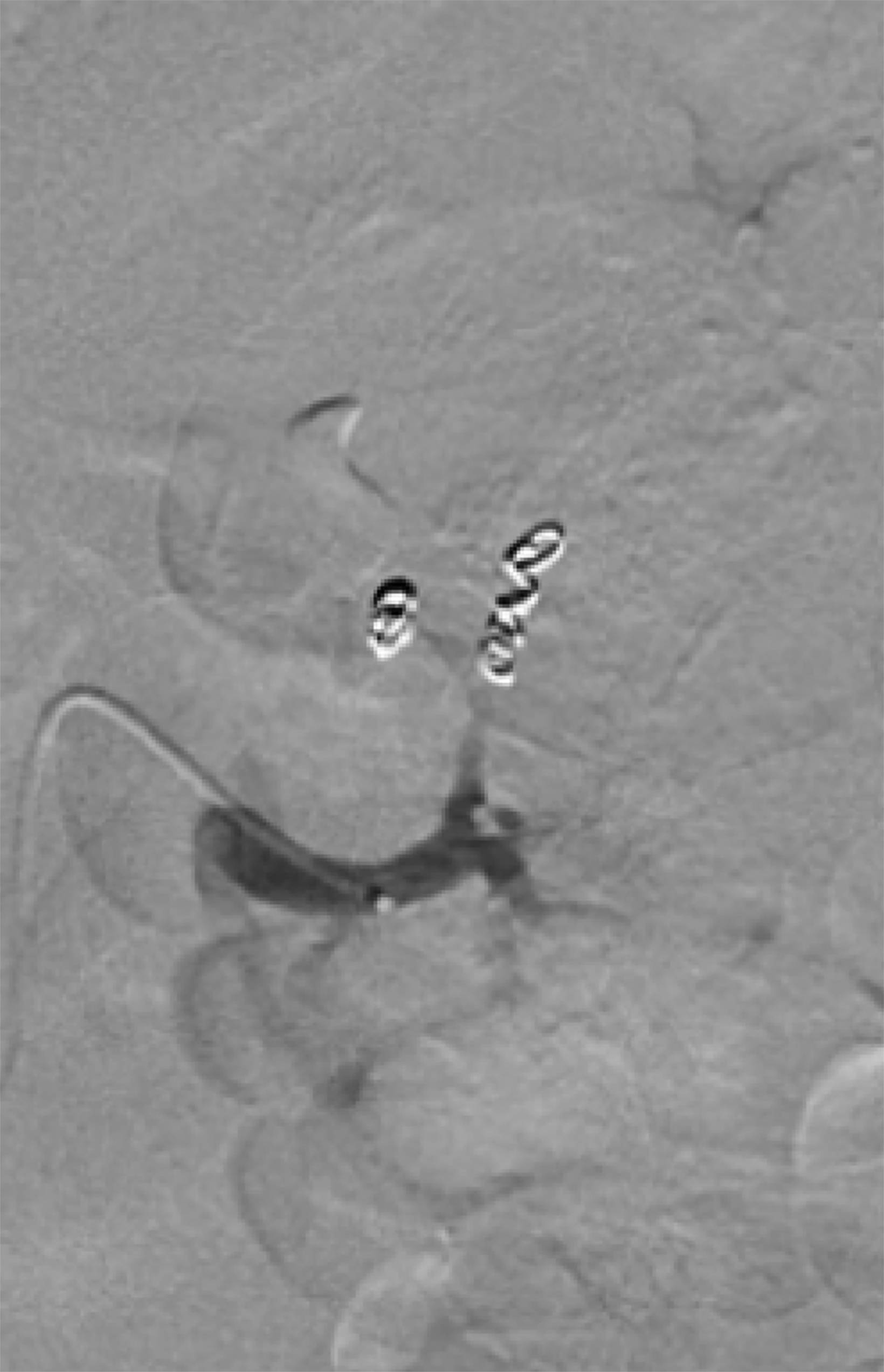
Angiomyolipoma (AML) is the most common benign renal neoplasm. It consists of fat, smooth muscle, and abnormally thick-walled vessels.9 This entity commonly affects women, usually between the ages of 40 and 70 years,9 and can present with a wide range of signs and symptoms, including hematuria, flank mass, hypertension, urinary tract infection, and renal failure in severe cases.10,11 While the tumor is benign, there is a risk of rupture (Figure 2). This is especially true for tumors larger than 4 cm and for those with pseudoaneurysms greater than 0.5 cm, which frequently call for embolization.10 A lipid-rich AML will often demonstrate internal enhancement on contrast-enhanced CT with low-attenuation areas of macroscopic fat density.3 Surveillance may be indicated in certain situations, as the risk of rupture increases with tumor size.10 There are no established guidelines for AML surveillance; however, the International Tuberous Sclerosis Complex Consensus Conference recommends that abdominal MRI or CT should be performed every 1-3 years to assess AML progression over the life of the patient.10
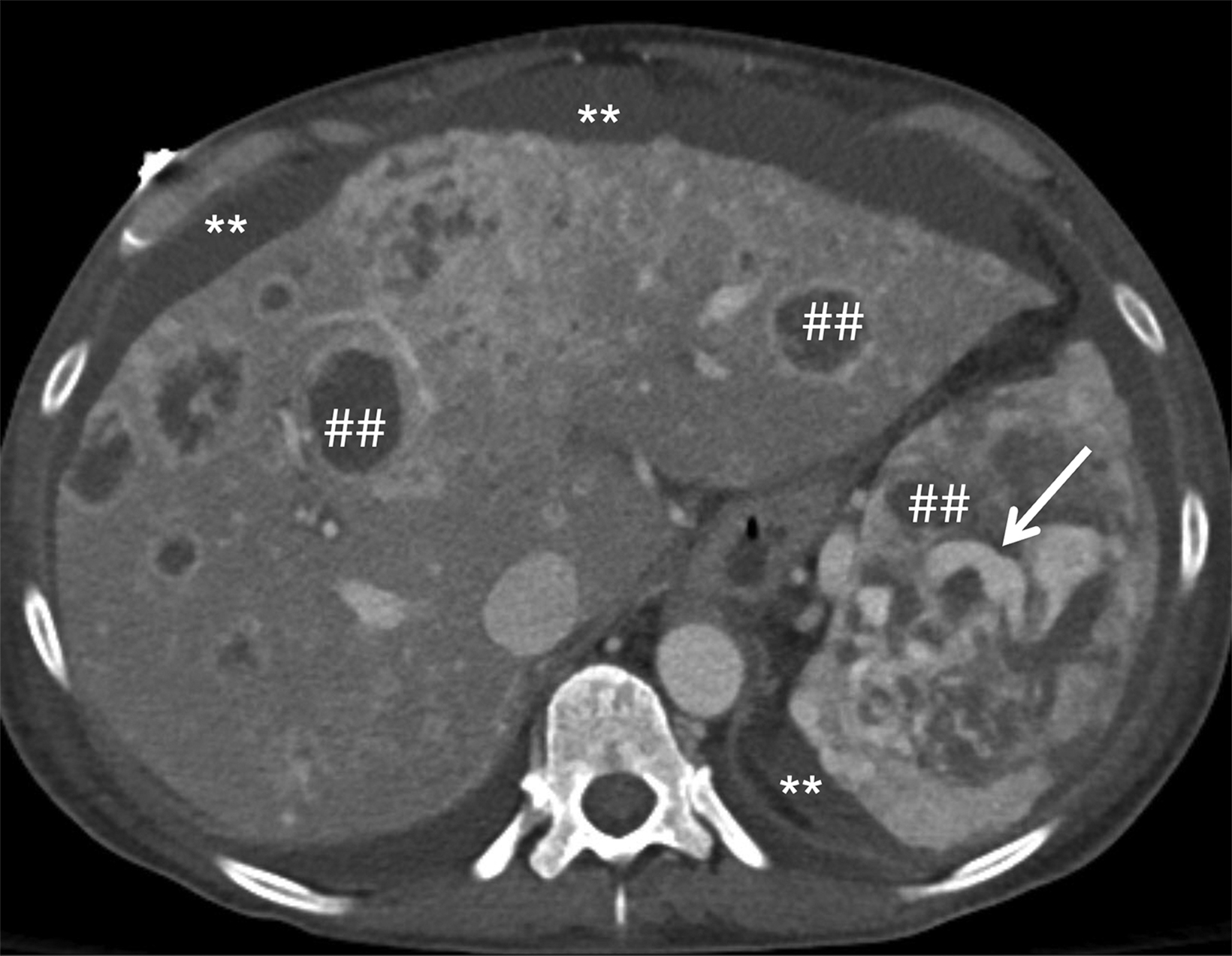
Splenic Angiosarcoma
A rare and aggressive type of hypervascular cancer, splenic angiosarcoma is typically composed of splenic endothelial cells.12
Like AMLs, splenic angiosarcomas more often affect women over age 40. Signs and symptoms may include left upper quadrant pain, weakness, unintentional weight loss, dyspnea, and back pain.13 Splenic rupture is a severe complication that is commonly fatal (Figure 3).14 As the lesion is refractory to radiation and chemotherapy, swift diagnosis can facilitate urgent splenectomy.15
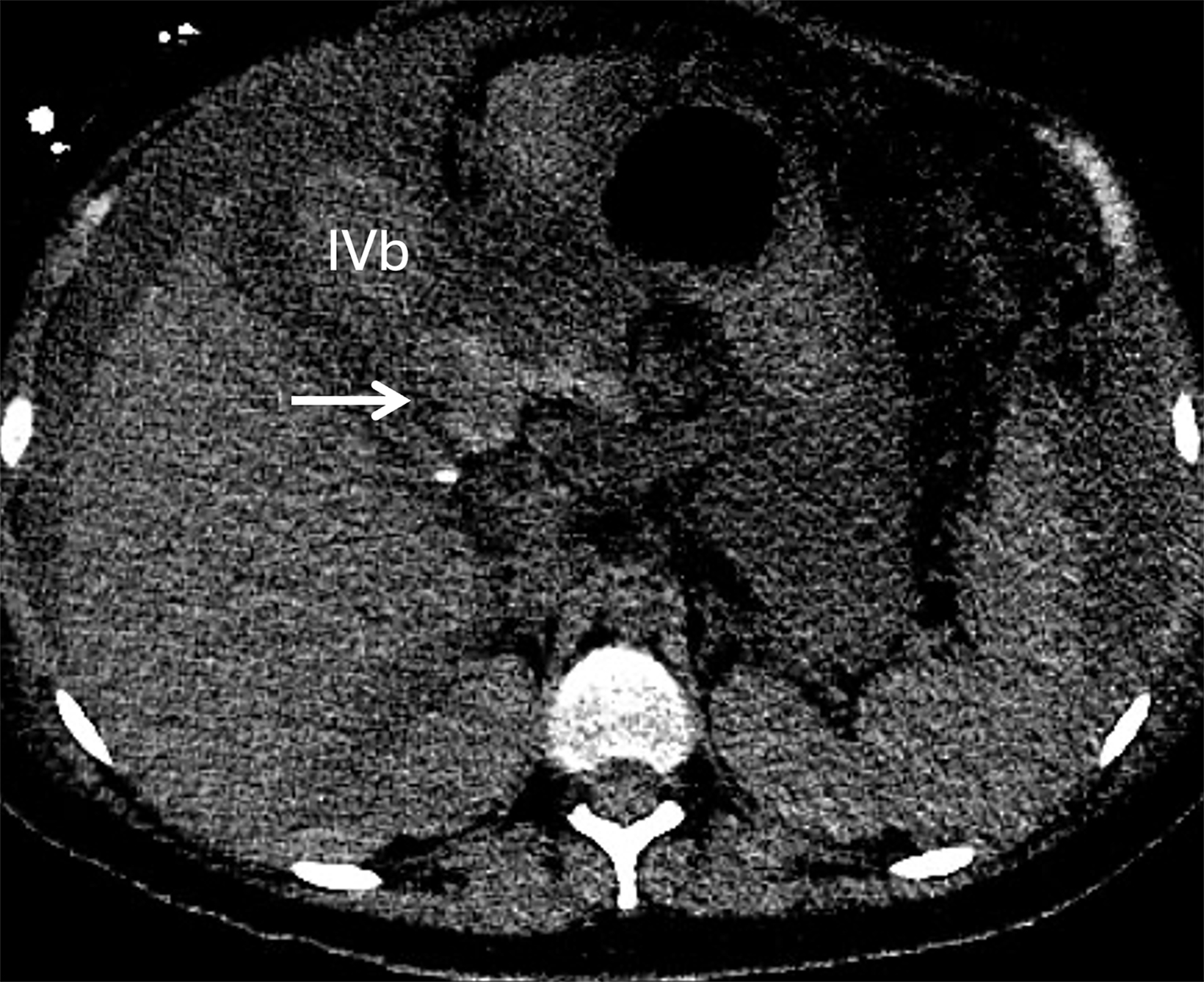
Liver Tumors
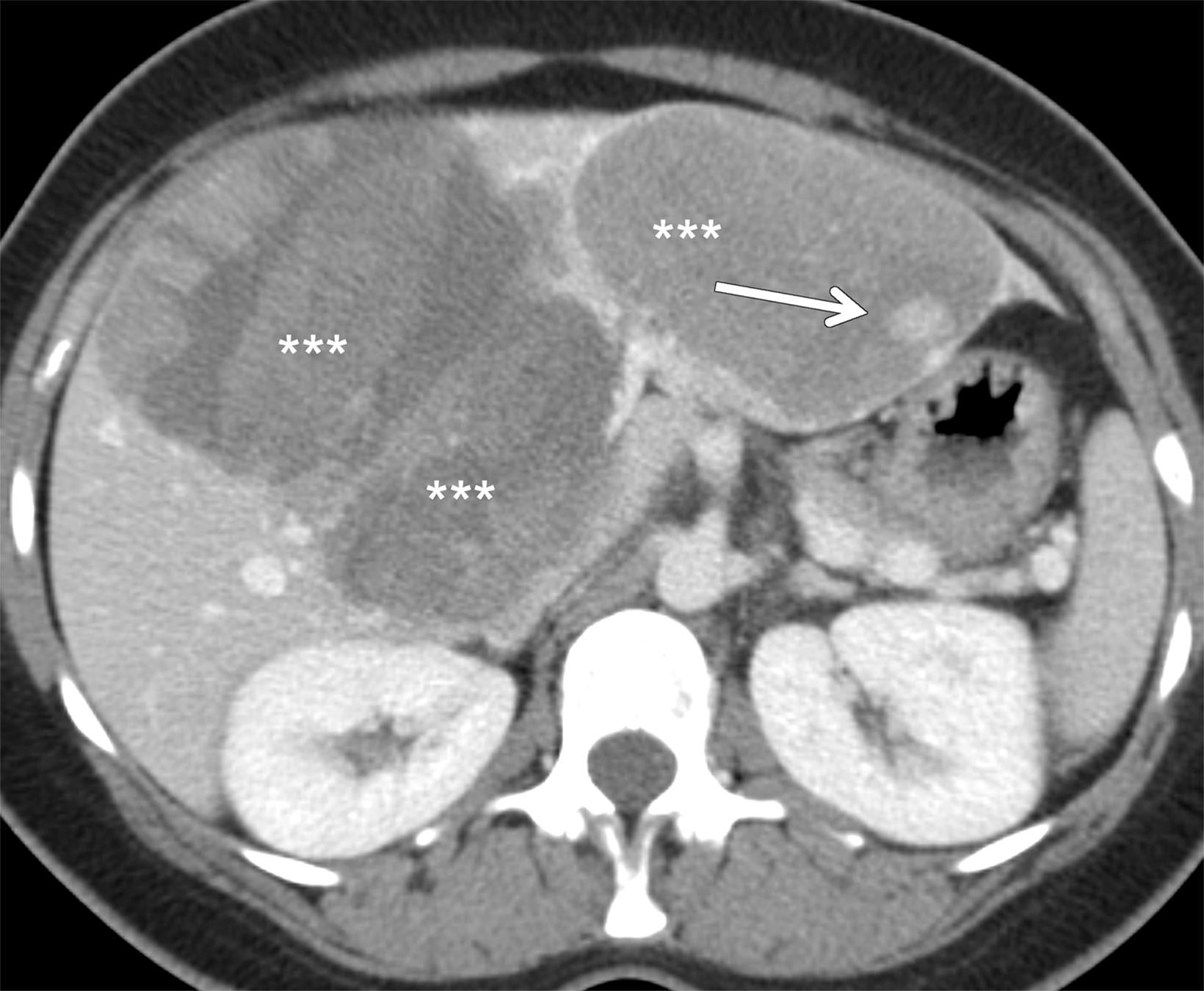
Hepatocellular adenoma (HCA) and hepatocellular carcinoma (HCC) and are the two most common liver tumors that may result in spontaneous hemorrhage.2 An uncommon benign neoplasm, HCA is most often found in women, usually during their reproductive years. It may be associated with hyperestrogenic states associated with obesity and the use of estrogen-based oral contraceptives.16 Accurately diagnosing an HCA as soon as possible is vital,16 as hemorrhage — often associated with large HCAs ( > 5 cm) — can cause right upper quadrant pain and hemodynamic instability (Figure 4),17 as well as spread into the liver or intraperitoneal cavity, requiring tumor resection.2 In many cases, rupture can lead to hemorrhagic shock, which requires emergent treatment.
Further highlighting the importance of prompt identification of these tumors, some subtypes can undergo malignant transformation into HCC.18
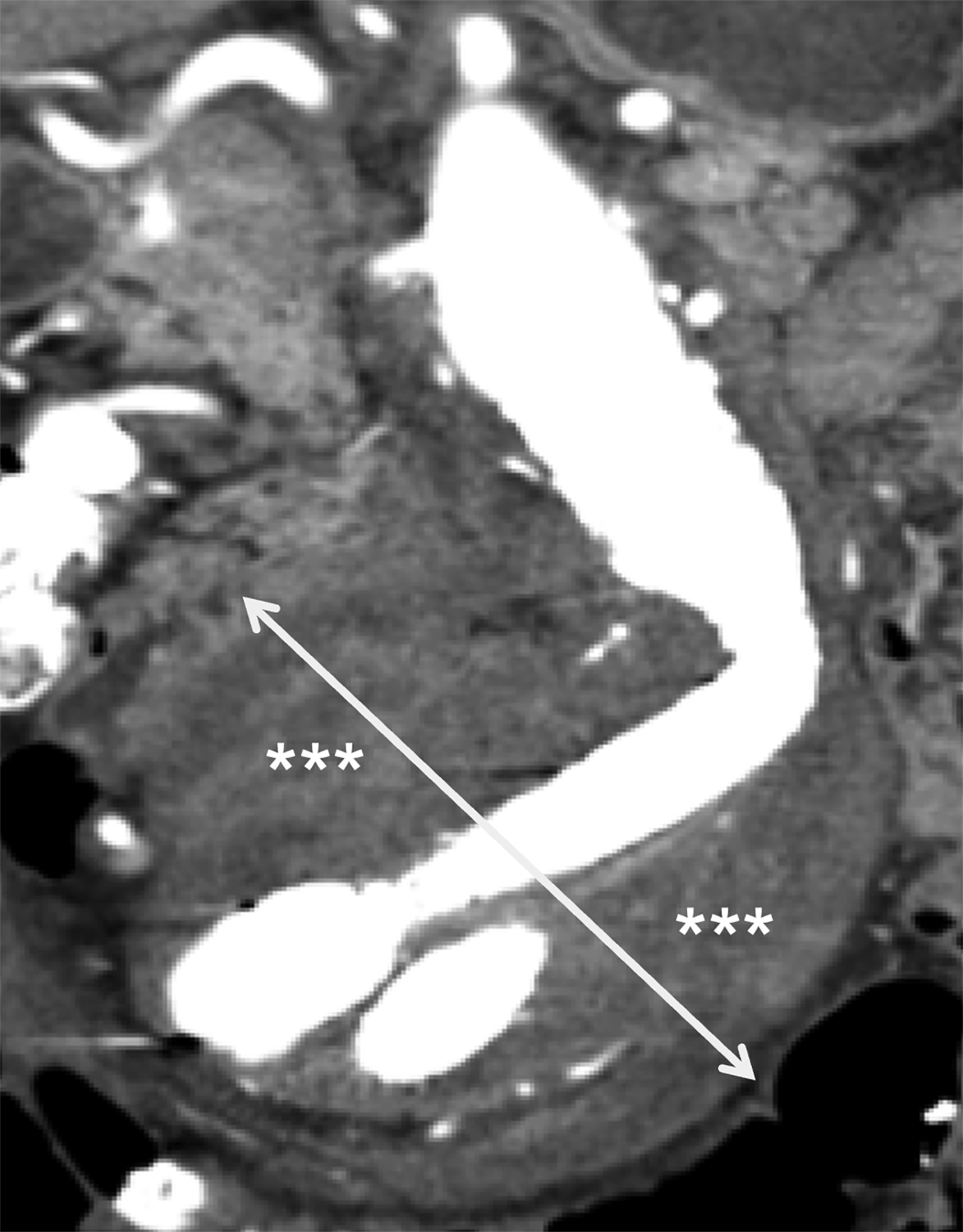
Hepatocellular carcinoma is the second-most common cause of cancer-related mortality in the world.18 This cancer is typically found in patients with cirrhosis and chronic hepatic inflammation, usually as a consequence of hepatitis B or hepatitis C.2,18 Rupture with hemorrhage into the peritoneal or subscapular space is a complication of HCC, occurring in 3-15% of cases (Figure 5).18 Larger and/or peripherally located tumors are at a higher risk of rupture; CT or contrast-enhanced MRI using a liver-mass protocol are the best modalities for diagnosis.19 Images of HCC rupture typically demonstrate discontinuity of the liver capsule, subcapsular/peritoneal hematoma, and active contrast extravasation.19
Gynecologic and Obstetric Causes
Ectopic Pregnancy Rupture
The most common causes of gynecological nontraumatic hemoperitoneum are ectopic pregnancy and hemorrhagic cyst ruptures.3
Ectopic pregnancy ruptures can be life threatening; thus, they should be considered for every person of childbearing capability who presents with abdominal pain or vaginal bleeding (Figure 6). Affecting about 1-3% of all pregnancies, ectopic pregnancy most often occurs in the ampulla of the fallopian tube.20 The diagnostic workup typically begins with serum β-HCG measurement and pelvic sonography. Patients with a β-HCG level over 2000 mIU/mL and an empty uterine cavity are at increased risk of ectopic pregnancy.2 On imaging, an adnexal mass with hemorrhage is concerning for the condition;3 if confirmed, these patients may require emergent surgery.
Ovarian Cyst Rupture
Ovarian cyst (typically a corpus luteal or follicular cyst) rupture is common in premenopausal people. Clinical findings are nonspecific but may include pelvic pain. The patient may not be pregnant, in which case the β-HCG levels are normal.3 However, it should be noted that a positive β-HCG does not exclude cyst rupture which, though rarely life threatening, should be promptly diagnosed and treated. In addition, while rarely causing severe hemorrhage (Figure 7), a ruptured cyst can mimic conditions such as appendicitis that require emergent surgery.2 Imaging will demonstrate a thick-walled cystic structure in the adnexa with internal echoes and focal wall discontinuity or irregularity, along with surrounding free fluid/blood products.21
HELLP Syndrome
Hemolysis, elevated liver enzymes, and low platelet count constitute a condition known as HELLP syndrome, another potential cause of hemorrhage. As a severe variation of preeclampsia,2 the syndrome should always be considered in the setting of acute or severe abdominal pain during pregnancy with abnormalities in the laboratory values.3 A rare complication of HELLP is hepatic hemorrhage (Figure 8), which can lead to hepatic rupture, placental abruption, hematoma, and other complications, increasing parental and neonatal mortality.22 In these patients, CT is the preferred imaging modality for characterizing intraperitoneal (Figure 8) and hepatic/perihepatic hemorrhage and infarctions.3,22 Hepatic infarction can appear on CT as low-attenuation, wedge-shaped areas around the liver periphery.23 Owing to the life-threatening nature of HELLP complicated by hepatic rupture, prompt evaluation and diagnosis are imperative.
Vascular Causes of Hemorrhage
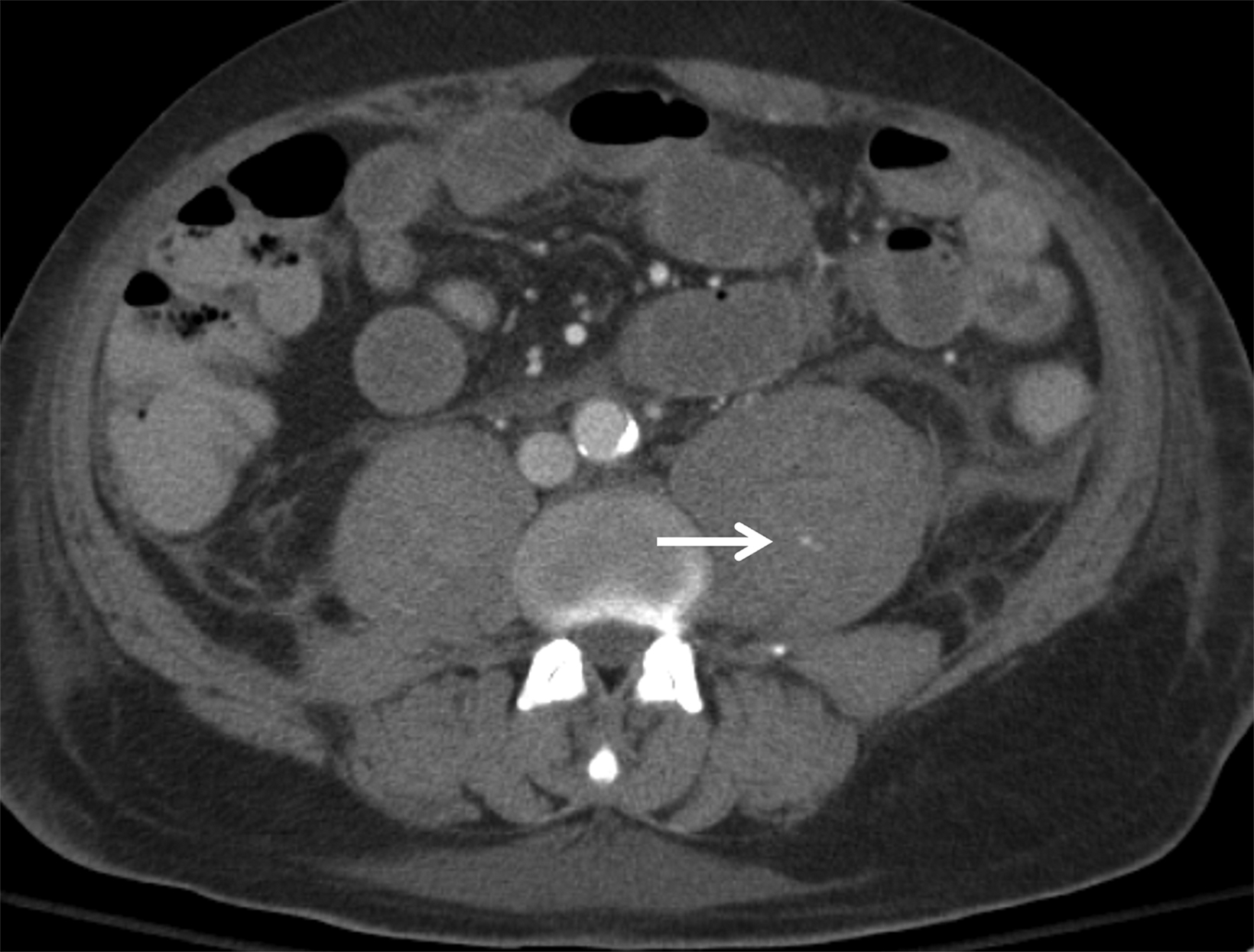
Abdominal Aortic Artery Rupture
Arterial bleeding can be caused by the rupture of an underlying vascular pathology. The most common cause of intra-abdominal vascular bleeding is a ruptured abdominal aortic aneurysm (AAA).24 Risk factors include male gender, advanced age, a history of cigarette smoking, a family history of AAA, hypertension, and hypercholesteremia.25 A ruptured AAA should be suspected in patients over 50 who present with severe abdominal or back pain and a pulsating abdominal mass.26 Computed tomography will show signs of active bleeding, loss of aortic wall continuity, the high-attenuation crescent sign, and retroperitoneal hemorrhage (Figure 9).24,27 Although many physicians prefer to proceed with immediate treatment without imaging, CT angiography is the preferred imaging modality for diagnosis.25
Iatrogenic Causes of Hemorrhage
Anticoagulation Therapy
Hemoperitoneum following anticoagulation therapy is not uncommon.28 Anticoagulants such as heparin and coumadin increase bleeding time, which in some cases can lead to life-threatening hemorrhage.28 The risk of bleeding, however, is typically related to medication dosage.2 Spontaneous hemorrhage commonly occurs in the rectus abdominis or the psoas muscles. Occasionally, anti-coagulation therapy can cause spontaneous hemoperitoneum or retroperitoneal hemorrhage. Computed tomography is beneficial in coagulopathic patients with suspected intra-abdominal bleeding.29
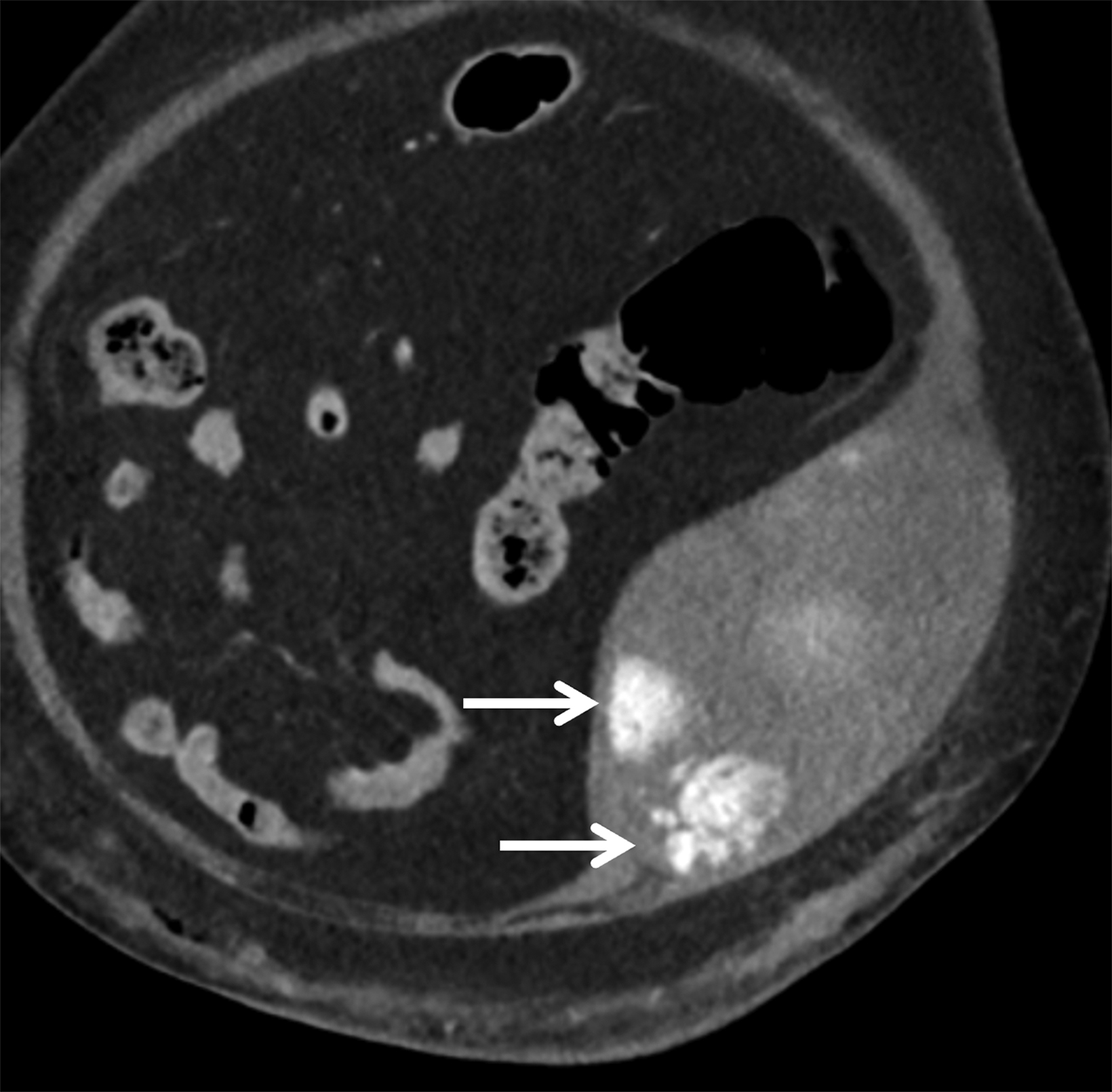
Hematomas of the Abdomen and Psoas Muscle
Rectus sheath hematoma (RSH) is often a clinically misdiagnosed cause of acute abdominal pain. This is due to an accumulation of blood in the sheath of the rectus abdominis (Figure 10), typically secondary to rupture of the inferior or superior epigastric vessel, or from a direct muscle tear.30 A common presenting feature is lower abdominal pain that never crosses the midline; the Carnett test can distinguish between tenderness occurring intra-abdominally and that occurring directly in the abdominal wall.30,31 During a straight-leg raise, abdominal pain that remains the same or gets worse (a positive test) suggests a somatic source, while pain that improves (a negative test) suggests an intra- abdominal/visceral source. Additional signs and symptoms include nausea, vomiting, chills, fever, and abdominal guarding.31 Because RSH is uncommon and frequently misdiagnosed, emergency physicians and radiologists should be familiar with this condition, which can mimic many other acute abdominal conditions. In these instances, failure to make a prompt and correct diagnosis could lead to a futile laparotomy.30
Psoas muscle hematomas occur when blood accumulates either under or within the psoas muscle (Figure 10).32 They can present as unilateral or bilateral, the latter being most common. They affect only about 0.1-0.6% of the population, mainly elderly patients on anticoagulants or receiving dialysis.32 The Cullen sign, which is ecchymosis in the periumbilical area, and the Grey- Turner sign, which is ecchymosis in the flanks, are common.33
Additional abnormalities may include muscle dysfunction and nerve palsy.34 Most psoas muscle hematomas, however, will resolve spontaneously without complication if they are not too large and/or compressing important surrounding structures.33
Conclusion
There are numerous sources of spontaneous, nontraumatic hemoperitoneum. Radiologist familiarity with their imaging features is crucial for accurate diagnosis and workup. While several imaging options are available, multidetector CT is generally the most efficient for diagnosis. Hemorrhage can be ascertained by the presence of a sentinel clot, active vascular blush, or hyperdense fluid near the organ of interest. Narrowing the site of hemorrhage can have important implications for treatment.
References
- Gomez E, Horton KM, Fishman EK, Johnson PT. CT of acute abdominopelvic hemorrhage: protocols, pearls, and pitfalls. Abdominal Radiology. 2021;47(1):475-484. doi:10.1007/s00261-021-03336-w.
- Lubner MG, Menias CC, Rucker CM, et al. Blood in the belly: CT findings of hemoperitoneum. RadioGraphics. 2007;27(1):109-125. doi:10.1148/rg.271065042.
- Furlan A, Fakhran S, Federle MP. Spontaneous abdominal hemorrhage: Causes, CT findings, and clinical implications. American Journal of Roentgenology. 2009;193(4):1077-1087. doi:10.2214/ajr.08.2231.
- Mortelé KJ, Cantisani V, Brown DL, Ros PR. Spontaneous intraperitoneal hemorrhage. Radiologic Clinics of North America. 2003;41(6):1183-1201. doi:10.1016/ s0033-8389(03)00118-0.
- Linehan MW, Berton Z, Bates S. Cancer of kidney and ureter. In: Devita VT Jr, Hellman S, Rosenberg SA, eds. Principles and Practice of Oncology, 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2001:1362–1396.
- Simon JW, Marshall FF. Kidney and ureter. In: Abeloff MD, Armitage J, Niederhuber J, Kastan M, McKenna W, eds. Clinical Oncology, 2nd ed. New York, NY: Churchill Livingstone; 2000:1784–1799.
- Ray RP, Mahapatra RS, Khullar S, Pal D, Kundu AK. Clinical characteristics of renal cell carcinoma: Five years review from a tertiary hospital in Eastern India. Indian Journal of Cancer. 2016;53(1):114. doi:10.4103/0019-509x.180851.
- Pummer K, Lämmer J, Wandschneider G, Primus G. Renal cell carcinoma presenting as spontaneous retroperitoneal haemorrhage. International Urology and Nephrology. 1990;22(4):307-311. doi:10.1007/bf02549788.
- Muttarak M, Pattamapaspong N, Lojanapiwat B, Chaiwun B. Renal angiomyolipoma with bleeding. Biomedical Imaging and Intervention Journal. 2007;3(4). doi:10.2349/biij.3.4.e8.
- Hatano T, Egawa S. Renal angiomyolipoma with tuberous sclerosis complex: How it differs from sporadic angiomyolipoma in both management and care. 2020;43(10):967-972. doi:10.1016/j.asjsur.2019.12.008.
- Altuwayr RM, Almutairi FS, Alkhaibari SH, et al. Spontaneous rupture of large angiomyolipoma of the kidney: a rare case. Cureus. November 2021. doi:10.7759/cureus.19908.
- Kania B, Vasani S. A case report of splenic rupture secondary to underlying angiosarcoma. Cureus. July 2020. doi:10.7759/cureus.9439.
- Autry JR, Weitzner S. Hemangiosarcoma of spleen with spontaneous rupture. Cancer. 1975;35(2):534-539. doi:10.1002/1097-0142(197502)35:2.
- Xu B, Xie X, Zhou X, Zhai M, Yang W. Spontaneous rupture of primary splenic angiosarcoma: A case report. Oncology Letters. 2015;10(5):3271-3273. doi:10.3892/ol.2015.3714.
- Hamid KS, Rodríguez J, Lairmore TC. Primary splenic angiosarcoma. JSLS. 2010;14(3):431-435. doi:10.4293/108680810x12924466006521.
- Dokmak S, Aussilhou B, Rasoaherinomenjanahary F, et al. Hemorrhage of hepatocellular adenoma: a complication that can be treated by conservative management without surgery. HPB. 2018;20(12):1198-1205. doi:10.1016/j.hpb.2018.06.1796.
- Papanikolaou, Giakoustidis D, Patsiaura K, et al. Management of a giant ruptured hepatocellular adenoma. Report of a case. PubMed. 2007. https://pubmed. ncbi.nlm.nih.gov/19582184. Accessed June 12, 2022.
- Thomas AJ, Menias CO, Pickhardt PJ, et al. Bleeding liver masses: imaging features with pathologic correlation and impact on management. American Journal of Roentgenology. 2019;213(1):8-16. doi:10.2214/ajr.19.21240.
- Sahu S, Chawla Y, Dhiman RK, et al. Rupture of hepatocellular Carcinoma: A review of literature. Journal of Clinical and Experimental Hepatology. 2019;9(2):245-256. doi:10.1016/j.jceh.2018.04.002.
- Della-Giustina D, Denny MW. Ectopic pregnancy. Emergency Medicine Clinics of North America. 2003;21(3):565-584. doi:10.1016/s0733-8627(03)00036-1.
- Pulappadi VP, Manchanda S, Sk P, Hari S. Identifying corpus luteum rupture as the culprit for haemoperitoneum. British Journal of Radiology. 2021;94(1117):20200383. doi:10.1259/bjr.20200383.
- Nunes JO, Turner MA, Fulcher AS. Abdominal Imaging Features of HELLP Syndrome: A 10-Year Retrospective Review. American Journal of Roentgenology. 2005;185(5):1205-1210. doi:10.2214/ajr.04.0817.
- Mortelé KJ, Cantisani V, Brown DL, Ros PR. Spontaneous intraperitoneal hemorrhage. Radiologic Clinics of North America. 2003;41(6):1183-1201. doi:10.1016/ s0033-8389(03)00118-0.
- Larrañaga N, Kozima S, Villarroel N, et al. Spontaneous abdominal hemorrhage: imaging evaluation. Revista interamericana de radiología. 2015. https://web-cir.org/revistavirtual/articulos/2015/noviembre/argentina/rar/spontaneous.pdf. Accessed June 12, 2022.
- Gawenda M, Brunkwall J. Ruptured abdominal aortic aneurysm: the state of play. Dtsch Arztebl Int. 2012;109(43):727-732. doi:10.3238/arztebl.2012.0727.
- Wilmink A, Quick CRG. Epidemiology and potential for prevention of abdominal aortic aneurysm. British Journal of Surgery. 1998;85(2):155-162. doi:10.1046/ j.1365-2168.1998.00714.x.
- Siegel C, Cohan RH, Korobkin M, Alpern M, Courneya DL, Leder RA. Abdominal aortic aneurysm morphology: CT features in patients with ruptured and nonruptured aneurysms. American Journal of Roentgenology. 1994;163(5):1123-1129. doi:10.2214/ajr.163.5.7976888.
- Lucey BC, Varghese JC, Anderson SW, Soto JA. Spontaneous hemoperitoneum: a bloody mess. Emergency Radiology. 2007;14(2):65-75. doi:10.1007/ s10140-007-0594-0.
- Nazarian LN, Lev-Toaff AS, Spettell CM, Wechsler RJ. CT assessment of abdominal hemorrhage in coagulopathic patients: impact on clinical management. Abdominal Radiology. 1999;24(3):246-249. doi:10.1007/s002619900489.
- Siu WT, Tang CN, Law BKB, Chau CH, Li MKW. Spontaneous rectus sheath hematoma. PubMed. 2003;46(5):390. https://pubmed.ncbi.nlm.nih.gov/14577716. Accessed June 15, 2022.
- Hatjipetrou A, Anyfantakis D, Kastanakis M. Rectus sheath hematoma: A review of the literature. International Journal of Surgery. 2015;13:267-271. doi:10.1016/j.ijsu.2014.12.015.
- Abedini L, Mehrabi S, Hosseinpour R, Jahantab MB, Salehi V, Barhaghtalab MJY. Non-penetrating traumatic psoas muscle hematoma presenting with gross hematuria: a case report. International Journal of Emergency Medicine. 2021;14(1). doi:10.1186/s12245-021-00345-w.
- Seo JG, Yang JC, Kim TW, Park KH. Intramuscular hematoma on the psoas muscle. Korean Journal of Neurotrauma. 2019;15(2):234. doi:10.13004/ kjnt.2019.15.e29.
- Zidouh S, Belkouch A, Mostafa R, Hicham B, Belyamani L. Conservative treatment of a psoas hematoma revealed by a lower limb palsy. Pan Afr Med J. 2017;28. doi:10.11604/pamj.2017.28.138.9930.
