Cooled RFA Delivers Long-term Pain Relief in Knee Replacement Patients
 A minimally-invasive cooled radiofrequency ablation (C-RFA) procedure delivers long-term relief for patients who experience chronic and debilitating pain after knee replacement surgery, according to a study being presented at the annual meeting of the Radiological Society of North America (RSNA). While a growing number of patients suffering from knee arthritis opt for total knee arthroplasty, 15 to 30% of people who get a knee replacement continue to experience pain and stiffness in the knee. They can go through surgery again, but there is no guarantee that the pain will not return.
A minimally-invasive cooled radiofrequency ablation (C-RFA) procedure delivers long-term relief for patients who experience chronic and debilitating pain after knee replacement surgery, according to a study being presented at the annual meeting of the Radiological Society of North America (RSNA). While a growing number of patients suffering from knee arthritis opt for total knee arthroplasty, 15 to 30% of people who get a knee replacement continue to experience pain and stiffness in the knee. They can go through surgery again, but there is no guarantee that the pain will not return.
“A lot of patients don’t achieve any resolution of pain,” said study lead author Felix Gonzalez, M.D., assistant professor in the Division of Musculoskeletal Imaging of the Department of Radiology and Imaging Sciences at Emory University School of Medicine in Atlanta, Georgia. “It’s a big problem, and up till now, there weren’t any other options.”
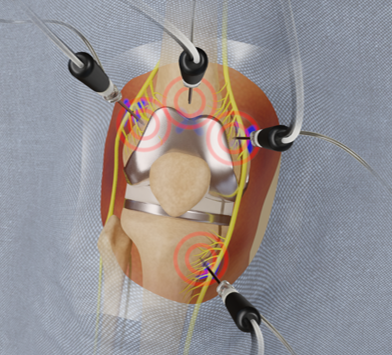
Providing hope for these patients, the C-RFA procedure involves insertion of an introducer needle around the knee under local anesthesia targeting specific nerve locations. A probe is then guided through the introducers. The tip of the probe imparts a low voltage current (radiofrequency) to the deep sensory nerves around the knee. Water circulating through the system allows for a greater dissipation of heat from the tip of the probe.
“With a larger propagating heat wave, you can account for the differences in nerve anatomy from patient to patient because of a larger treatment zone,” Dr. Gonzalez said. “Treating a larger zone increases the effectiveness of the procedure.”
In previous studies, Dr. Gonzalez’s group showed that C-RFA provides lasting pain relief for people with knee, shoulder and hip arthritis. The new study focused on 21 patients who were experiencing persistent chronic pain after total knee replacement, without underlying hardware complications. The patients had all failed conservative care. They filled out clinically validated questionnaires to assess pain severity, stiffness, functional activities of daily living and use of pain medication before and after the procedure. Follow-up outcome scores were collected up to one year after the C-RFA procedure.
Questionnaire results showed that the patients experienced, on average, a statistically significant improvement in quality of life. Both pain and stiffness scores improved dramatically. No major complications were encountered, and no patients required repeat treatment, surgical revision or other intervention.
“This procedure can have a huge impact in patients who have gone through major surgery and are still suffering pain that is very debilitating,” Dr. Gonzalez said.
The procedure’s long-term relief gives it a major advantage over cortisone injections, which offer on average only about three months of pain relief in the treatment of knee arthritis.
“It’s very encouraging that up to a year out these patients have such significant pain relief and a better quality of life,” Dr. Gonzalez said. “The hope is that in that period of time, the patient can become more mobile and increase their activity. Even if pain comes back, we predict that it won’t come back with the same intensity as before.”
Since it is minimally invasive, the procedure can easily be repeated, according to Dr. Gonzalez. It can also reduce or eliminate the use of opioid pain relievers, which carry significant risks associated with dependency.
“We hope that this procedure will become a standard of treatment for pain in this setting,” Dr. Gonzalez said.
