CT of liver transplantation
Images









Dr. Ryan and Dr. Sidhu are Consultant Radiologists, Department of Radiology, King's College Hospital, London, England.
Transplantation is an established treatment for end-stage liver disease, whatever the precipitating cause. Imaging of both the pre- and posttransplant patient is an important facet of patient management. Advances in immunosuppressive therapy, surgical techniques, perioperative care, and imaging have combined to improve the outcome of liver transplantation; 1-year survival is now >85%, with a quoted 5-year survival rate of 65% to 78%. 1 Graft survival relies on prompt diagnosis of complications. Although there is a reliance on ultrasound (US) for assessing vascular and nonvascular complications, particularly in Europe, there is an important role for computed tomography (CT). CT imaging in the peri- and postoperative phase is used in the evaluation and diagnosis of vascular and biliary complications, focal collections (bile or infective), and hematomas, and for the assessment of the presence of pelvic fluid collections. Postoperative disease recurrence and posttransplant lymphoproliferative disease (PTLD) may be readily detected with CT.
Radiological assessment of the liver transplant
The candidate
Preoperative clinical and radiologic evaluation of the transplant candidate is essential for appropriate patient selection. 2-4 The objectives of preoperative radiologic evaluation in the recipient include assessment of vessel anatomy and patency as well as exclusion of intra- and extrahepatic malignancy. Identification of cirrhosis, sequelae of portal hypertension, and quantification of the volume of the diseased liver may be performed. Further information available on CT that is useful to the transplant surgeon includes the status of the celiac artery, the presence of splenic artery aneurysms, and the position of any spontaneous portosystemic venous shunts. 3,4
A shortage of cadaver donor livers has led to the institution of "live-related" donor transplantation. In the preoperative period, a CT of the donor assesses liver volume and vascular anatomy, excludes focal liver lesions, and identifies any unsuspected anomalies that would preclude surgery.
Hepatic parenchyma
The typical cirrhotic liver morphology shows hypertrophy of the caudate lobe (segment I according to the Couinaud classification) and the left lateral liver segments (segments II and III), with atrophy of the remaining liver (Figure 1). The presence of congestive splenomegaly, ascites, and portosystemic collaterals allows for the documentation of portal hypertension. 4,5
Hepatocellular carcinoma
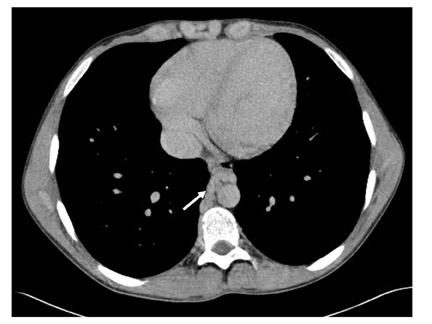
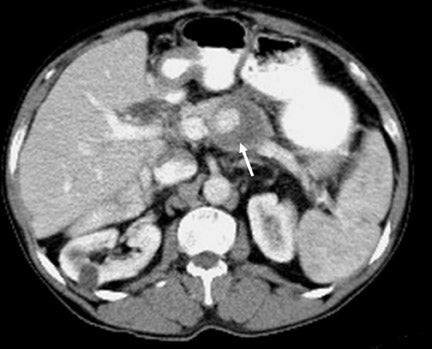
Most candidates for liver transplant will have cirrhosis and, with it, a greater risk of an associated hepatocellular carcinoma (HCC). Screening for HCC should be performed preoperatively. 2 However, the presence of HCC does not preclude transplantation, and in some instances, transplantation is curative. 6,7 The presence of lesions ≥5 cm in diameter, the presence of ≥3 lesions (the "Milan criteria"), or evidence of extra-hepatic spread are accepted contraindications to transplantation. 8 Hepatocellular carcinomas are best visualized on arterial-phase images, where they appear as avidly enhancing nodules that become hypodense on the portal-venous phase (Figure 2).
Larger lesions tend to have a typical mosaic enhancement pattern and may show a peripheral capsule. 9 Portal vein (PV) and hepatic vein involvement from tumor extension is also characteristic. The preoperative detection of a cholangiocarcinoma is an absolute contraindication to liver transplantation. The rate of recurrence is reported to be as high as 44%. 8
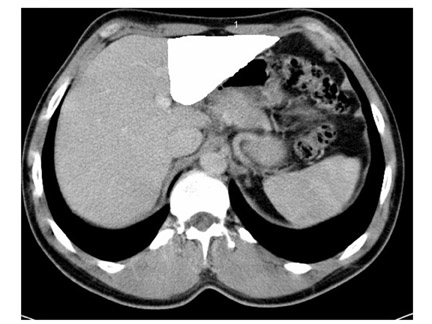
Liver volume
Assessment of the liver volume is important in live-related donors, both to ensure that adequate liver volumes remain in the donor and that an adequate volume of liver is transplanted into the recipient; liver graft size is one of the major factors that determines a successful outcome. A graft that is too large for the recipient is associated with a risk of graft compression, which leads to poor vascular perfusion. Conversely, a liver graft that is too small for the recipient may cause postoperative liver failure or primary nonfunction. 10 The volume of a cross-sectional area of liver seen on a given CT image can be determined simply from a mechanical tracing of the liver outline, which is then multiplied by the slice thickness to obtain the volume of liver represented by that image. 3,4 CT-determined volumes have been shown to be accurate and reproducible (Figure 3). 11
Vascular evaluation
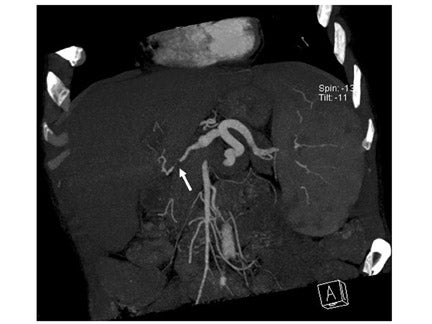
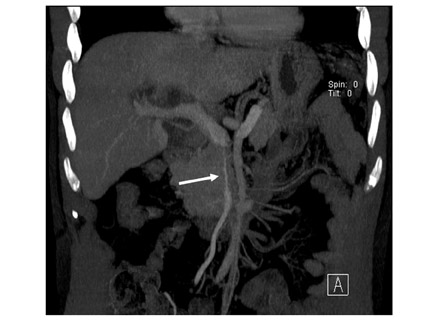
Knowledge of the exact arterial supply to the liver may be important to the surgeon when planning vascular reconstruction, as numerous variations in the normal vascular supply exist. 5 The advent of multislice CT allows rapid evaluation of large volumes of the liver with excellent spatial resolution. CT angiography (CTA), with 3-dimensional (3D) or maximum-intensity-projection (MIP) arterial reconstructions, has been shown to have a significant impact on surgical planning for liver transplantation. 12 Furthermore, 3D CT arteriography allows for accurate planning of the transsection plane in live-related donor transplantation. 13 The arterial anatomy is of particular importance in live-related transplantation selection, as up to one third of donors are ineligible for transplant following identification of unsuitable anatomy of segments II and III. 14
Portal-vein occlusion occurs in up to 10% of patients with end-stage cirrhosis. 15 The presence of PV thrombosis does not preclude surgery, but preoperative recognition on contrast-enhanced CT facilitates appropriate surgical strategies, such as a venous "jump-graft" from the superior mesenteric vein (SMV) to the donor PV. 16,17 Size discrepancy between the donor and recipient PV may necessitate a donor-iliac vein graft to connect the SMV to the PV. 2
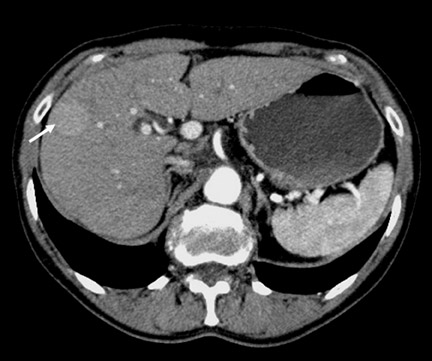
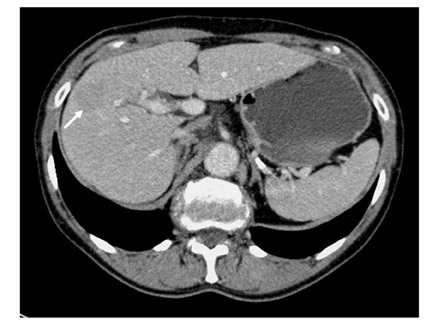
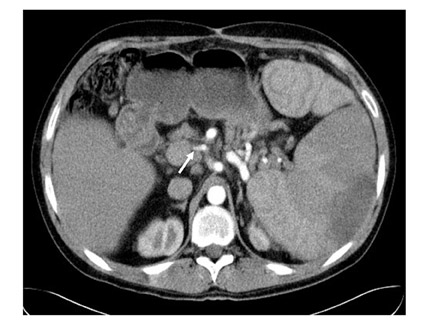
Splenic artery aneurysms occur in patients with cirrhosis and portal hypertension and are thought to be a consequence of increased flow in the splenic artery. 18 Therefore, preoperative identification on CT is important, as there is increased risk of rupture of splenic artery aneurysms following liver transplantation (Figure 4). This area is not routinely visualized at the time of surgery. Preoperative identification of porto-systemic shunts and varices is also useful, as these may be ligated at surgery to optimize blood flow toward the liver. Preoperative identification may also minimize dissection time. 2
Postoperative imaging
Most deaths occur in the first 6 months following orthotopic liver transplant, so prompt diagnosis of complications is critical for graft salvage. Noninvasive imaging-both US and CT-allows for patient assessment when clinical signs and symptoms advocate, allowing for early management. 19
Surgical techniques
Orthotopic liver transplant using the "piggy-back" technique requires at least 3 vascular anastomoses: extrahepatic portal vein, hepatic artery, and suprahepatic vena cava with the adjoining hepatic veins. The inferior vena cava (IVC) is preserved, and the caval anastomosis is performed on a common ostium formed from the 3 suprahepatic veins. In this scenario, thrombosis is expected to occur in the ligated infra-hepatic donor IVC and should not be misinterpreted as thrombosis on contrast-enhanced CT. 20 A fourth anastomoses is performed when the liver is placed in the standard orthotopic position; the infrahepatic donor vena cava is anastomosed to the recipient infrahepatic vena cava, and the superhepatic vena cava anastomoses are retained. Modifications to the standard technique may sometimes be necessary; if the celiac axis or hepatic artery flow is significantly decreased on contrast-enhanced CT, the donor iliac artery may be grafted from the recipient aorta to the donor hepatic artery. This "conduit" will minimize the possibility of postoperative graft infarction. 16,21
Vascular complications
CT angiography allows for the detection of hepatic arterial abnormalities. 12 Often, CTA is used as the second-line investigation in the diagnostic algorithm for hepatic artery thrombosis after the use of color Doppler US.
Hepatic artery thrombosis
The hepatic artery is the sole arterial supply to the biliary system after liver transplantation; all potential collaterals have been severed, and hepatic artery occlusion "de-arterializes" the liver and biliary tree (Figure 5). 22,23 Hepatic artery thrombosis is the most common vascular complication of liver transplantation, with a prevalence of 4% to 12% in adult recipients and up to 40% in children, usually occurring within 2 months of liver transplantation. 24,25 Proposed risk factors include the surgical difficulties related to the anatomic site of the anastomoses, arterial anomalies, the use of vascular conduits, small arterial size (<3 mm), and the need to surgically revise the anastomoses. 23 Clinical presentation varies from mild elevation of liver enzymes to delayed bile leak, biliary strictures or ischemia leading to relapsing bacteremia, or fulminate hepatic ne-crosis. 24 Management is surgical, either with an arterial thrombectomy or liver retransplantation. With retransplantation, mortality is up to 27%, but without retransplantation, the mortality is approximately 73%. 26
Color Doppler US is the initial imaging technique used for hepatic artery evaluation in the immediate posttransplant period. However, it may produce false-negative results because of the presence of periportal collateral arteries that bypass the occluded segment of the hepatic artery and reconstitute intrahepatic arterial flow. 27 Color Doppler US has a quoted sensitivity of 80% to 90% and is improved with the addition of microbubble US contrast media. 28,29 CT angiography with MIP is accurate in imaging the hepatic artery to confirm or refute ultrasonically suspected hepatic artery thrombosis or stenosis, with quoted sensitivities of 100%, and accuracy of 95% in the detection of all vascular complications post-liver-transplantation. 12,30-32 The role of CTA is essentially the second-line investigation in the diagnostic algorithm for hepatic artery thrombosis, following an equivocal color Doppler US.
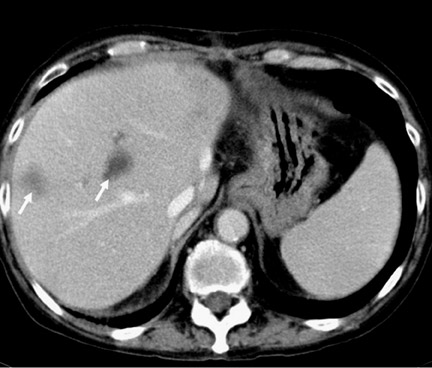
Sequela of hepatic artery thrombosis can also be visualized. Hepatic artery vascular insufficiency from either stenosis or thrombosis may lead to necrosis of bile duct epithelium, which may lead to hepatic infarction, bilomas, abscesses, and nonanastomotic bile leak. In one series, 86% of transplant patients with hepatic abscesses or infarction were found to have hepatic artery thrombosis. 26 On CT, 3 general appearances of hepatic infarction may be seen: peripheral wedge-shaped lesions, rounded lesions that may be peripheral or central, and irregularly shaped lesions that follow the course of the bile ducts (Figure 6). 19
Hepatic artery stenosis
The reported prevalence of hepatic artery stenosis varies from 5% to 11%. It is the second most common vascular complication after thrombosis, and usually occurs at the anastomotic site within 3 months of transplantation. 33,34 Early detection is important, as the stenosis is amenable either to balloon dilatation or surgical intervention. If untreated, hepatic artery stenosis may cause hepatic ischemia, hepatic artery thrombosis, and, ultimately, graft loss. 33 Revascularization procedures are usually successful, with long-term graft and patient survival assured. Comparison of 3D CTA, using MIP and shaded-surface display techniques, with conventional angiography have shown CTA to be a practical noninvasive method of diagnosing hepatic artery stenosis (Figure 7). 12,31,32
Hepatic artery pseudoaneurysm
Hepatic artery pseudoaneurysms are uncommon, with a reported incidence of 1% to 2%, often caused by a combination of infection and surgical technical malfunction. 35,36 Hepatic artery pseudoaneurysms most often occur in the second and third week after transplantation. Presentation may be nonspecific with hemobilia, unexplained fever, graft dysfunction, or a falling hemoglobin level. Hepatic artery thrombosis may occur as a consequence. The hepatic artery pseudoaneurysm may be intra- or extrahepatic; when intra-hepatic, it is often related to an iatrogenic cause (eg, biopsy) and when extrahepatic, it is often caused by infection. The diagnosis may be difficult. CT may show a low-attenuation area that enhances with intravenous contrast, either within the liver or related to the porta hepatis (Figure 8). However, if partial thrombosis is present within the pseudoaneurysm, it may be missed. Secondary signs of ischemia on CT may indicate the need for angiography. 35
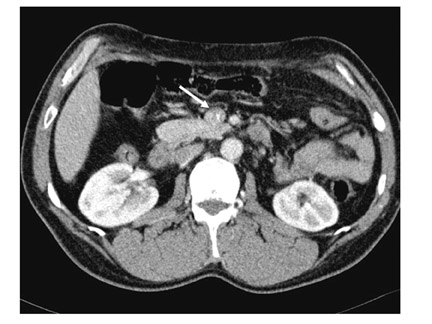
Portal vein thrombosis and stenosis
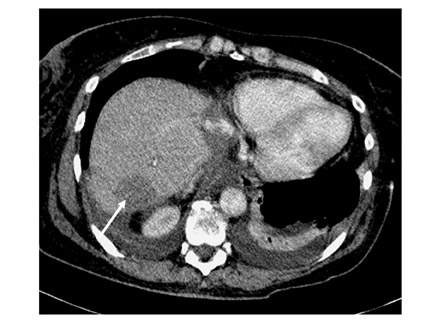
Portal-vein complications are rare, with an incidence of 1% to 2%. 37 The narrowing of the vessel that is suggestive of stenosis may be seen on CT, but the functional significance should be confirmed with pressure-gradient measurement at angiography. Similar features may be found with a donor-recipient size discrepancy. 37 In cases of functionally significant stenosis or of PV thrombosis, secondary features of portal hypertension may be evident on CT, such as varices, bowel edema, and ascites. 26 Portal-vein thrombosis is evident on contrast-enhanced CT as a low-attenuation lesion within the involved portal venous segment with or without expansion of the vessel, with possible enhancement at the margin of the thrombus. 38 Thrombosis of the PV, SMV, or IVC after liver transplantation is seen almost exclusively in pediatric recipients (Figure 9). 39
Inferior vena cava stenosis and thrombosis
Complications that involve the hepatic veins and IVC occur in <1% of patients. 40 Inferior vena cava stenosis or thrombosis is usually related to the surgical anastomoses site or to the presence of a hypercoagulable state. 24,37 As with PV stenosis, the functional significance of IVC stenosis requires confirmation with measurement of the pressure gradient across the stenosis. The possibility of stenosis is increased with the "piggy-back" technique, especially when the right hepatic vein is ligated to match the size between the donor and recipient IVC. The treatment of choice in IVC stenosis is balloon dilatation. 36
Biliary complications
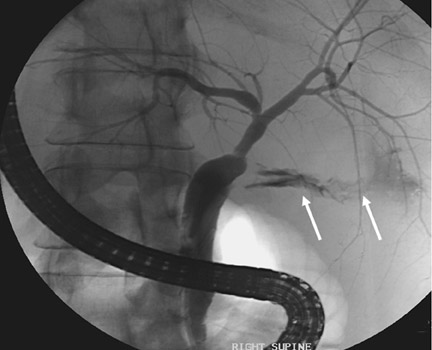
Despite improvements in surgical technique, biliary tract complications remain an important cause of morbidity and mortality in up to 15% to 30% of transplant patients. 41 Early diagnosis and prompt intervention has decreased mortality. 42 Most biliary complications occur within 3 months following transplantation, although some, such as strictures and stone formation, can develop months to years later. 19 Although biliary leakage and anastomotic obstruction (partial or complete) are the most common complications, other potential problems include dysfunction of the ampulla, mucoceles, intrahepatic biliary strictures, "bile cast" syndrome, bilomas, hepatic abscesses, biliary stones, and stent-related complications (Figure 10). 43
Bile leak resulting from bile duct necrosis secondary to hepatic ischemia or liver biopsy may also occur. 19 T-tube cholangiography, magnetic resonance cholangiopancreatography (MRCP), and US are the best noninvasive means for evaluating the biliary tree. CT is best used to reveal associated biliary complications (Figure 11). 24 Bilomas that are adjacent to the site of the bile leak may be visualized and drained by percutaneous methods using CT guidance. The coexistence of arterial pathology with biliary complications must be considered in the case of non-anastomotic bile leaks, as a biliary reconstruction or revision in the presence of an inadequate arterial supply will inevitably result in further complications. 43 Careful assessment of the hepatic artery on CT is essential in patients with nonanastomotic bile leaks. When arterial problems are encountered in the context of bilomas, drainage may offer temporary relief from symptoms, but the definitive solution is usually retransplantation. 19,43
Biliary strictures
Strictures, either anastomotic or non-anastomotic, occur in 4% to 17% of grafts. 19 Most biliary strictures occur at the anastomotic site and are probably caused by scarring and retraction after surgery, although the anastomoses may be involved by the same processes (such as ischemia) that lead to nonanastomotic strictures. 24 Nonanastomotic strictures, often ischemic in origin, are also caused by infection, chronic rejection, prolonged cold preservation time, cytomegalovirus (CMV) or Cryptosporidium infection, or recurrence of primary sclerosing cholangitis. 44 If a stricture is suspected and CT does not show any biliary dilatation, endoscopic retrograde cholangiopancreatography or percutaneous transhepatic cholangiography should be performed, as many liver transplants do not develop bile duct dilatation, even when there is high-grade narrowing. 24
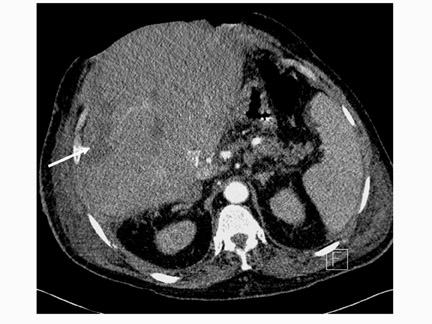
Fluid collections and hematoma
The majority of patients develop a right-sided pleural effusion that tends to be a transudate and generally resolves within a few days. 45 If the pleural effusion does not resolve and enlarges, then patients should be evaluated for subdiaphragmatic abnormalities. Up to 70% of patients with an enlarging pleural effusion 3 days after liver transplant will exhibit a sub-diaphragmatic abnormality, such as an abscess or a hematoma (Figure 12). 46 Small parahepatic hematomas are common after surgery, and these tend to occur in the gallbladder fossa and the hepatorenal space. Hematomas may be distinguished on CT imaging from other fluid collections by their higher attenuation coefficient. 24,47 Hematomas usually resolve without complication, and intervention is not indicated, unless superimposed infection is suspected.
Abscess formation complicates up to 10% of liver transplantations. 48 In the presence of symptoms of an infection, CT is the investigation of choice, particularly if an US examination is inconclusive. However, no single imaging modality can determine if a collection is infected or not, and percutaneous aspiration will be necessary in septic patients. 19 Extrahepatic abscesses tend to occur in the subphrenic or subhepatic spaces, and percutaneous drainage is normally feasible. Intrahepatic abscesses frequently occur as a result of vascular compromise or arise as an infected biloma secondary to stricture formation (Figure 13). Percutaneous drainage may be performed, but correction of the underlying cause must be addressed. Collections around the porta hepatis may be associated with hepatic artery pseudoaneurysm formation, so particular attention must be paid to the vessels in this area on CT imaging, and correlation with color Doppler US is necessary prior to needle placement for drainage.
Spontaneous hemorrhage in the postoperative period occurs in <10% of patients and may occur secondary to breakdown of vascular anastomoses, pseudoaneurysm rupture, or bleeding after liver biopsy. 49 This is usually a clinical diagnosis, although CT has a role in stable equivocal patients and may reveal the site of bleeding if there is active extravasation.
Malignancy
Posttransplantation lymphoproliferative disorder
Posttransplantation lymphoproliferative disorder (PTLD) occurs in 2% to 10% of adults, with a higher incidence in children and may present as early as 1 month posttransplant. 50 Recognition of the CT findings of PTLD is important, as early diagnosis may result in an improved response to therapy. Extranodal disease is the most common presentation. The liver and gastrointestinal tract are the most common sites of disease; the liver is involved in 50% of cases. Within the liver, PTLD can manifest as multiple discrete nodular low-attenuation lesions on contrast-enhanced CT (Figure 14), an infiltrative pattern, consisting of a geographic or an ill-defined region of low attenuation with or without hepatomegaly, and, lastly, as a periportal mass that extends into the biliary tree with associated periportal lymphadenopathy. 50,51
With PTLD, CT of involved hollow organ viscera shows localized circumferential wall thickening, dilatation of involved loops, luminal excavation or ulceration, eccentric polypoid masses, extramural extension, and intussusception. Lymph node involvement is seen in 22% of cases, with the lymph nodes at the porta hepatis and celiac axis most commonly involved. Splenic involvement is revealed on CT by the presence of splenomegaly and focal low-attenuation lesions. 50 CT-guided biopsy can be performed to confirm the diagnosis.
Hepatocellular carcinoma
Liver transplantation for HCC provides excellent outcomes, applying the Milan criteria, with 5-year survival rates of 70% and low recurrence rates. 52 The liver, lung, and bone are the most frequent sites of disease recurrence. 53,54
Other complications
Intra-abdominal
Most liver diseases for which liver transplantation is performed recur after liver transplantation. The clinical impact of recurrence varies. For autoimmune liver diseases (such as primary biliary cirrhosis, primary sclerosing cholangitis, and autoimmune hepatitis), clinically significant recurrence appears to be relatively rare. 55 Cirrhosis secondary to hepatitis C is the leading indication for liver transplantation in the United States. Hepatitis C viremia after liver transplantation has been reported in 75% to 95% of patients, with clinical as well as histologic recurrence in 40% to 60% of patients. 56 Although CT cannot diagnose disease recurrence, it will show a cirrhotic configuration to the liver in established cirrhosis. Other miscellaneous abdominal complications that can occur include splenic infarction, right adrenal infarction due to ligation of the right adrenal vein, rupture of a splenic pseudoaneurysm, and bowel obstruction secondary to adhesions. 19,57
Extra-abdominal
Infection affects up to 70% of liver transplant recipients and is the second most common complication after rejection and graft dysfunction. The majority of symptomatic infections are bacterial and relate to surgery, ventilation, and intravenous cannulae. Cytomegalovirus infection occurs in 45% to 100% of recipients but is asymptomatic in the majority of patients. Fungal infections are primarily due to Candida albicans, but infections due to Aspergillus occur in approximately 6% and carry a high mortality. CT imaging of the chest, abdomen, and brain may be helpful in establishing the diagnosis in selected cases. 24,58,59
Rejection
Rejection occurs in more than one third of transplant recipients. There are no specific CT imaging features that are diagnostic of rejection, but CT serves to exclude other causes of elevated liver enzymes. 60
Conclusion
Multidetector CT imaging is an invaluable technique for evaluating the pre- and postoperative liver transplant patient, allowing for the accurate assessment of the pretransplant candidate and the early detection of complications. A sound understanding of the clinical abnormalities that can occur following transplantation will allow the radiologist to make a sound interpretation of the CT findings, which then enables rapid implementation of the correct management strategy.