Diagnosing osteoarthritis at early stages with novel high-resolution cone-beam CT
A new generation of high resolution x-ray detectors used with new algorithms for data processing may enable in vivo evaluation of the fine details of bone microstructure in patients. This imaging technology may help physicians detect osteoarthritis in its early stages, according to preliminary research presented at the annual meeting of the American Association of Physicists in Medicine (AAPM) held in July in Washington, D.C.
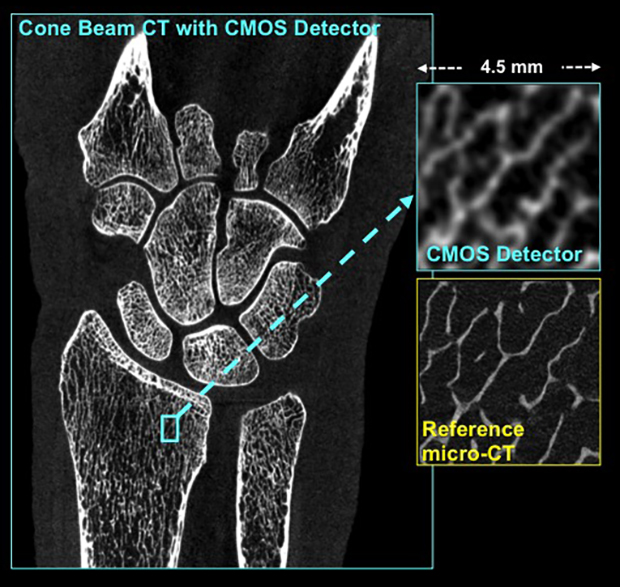
The extremity cone-beam CT (CBCT) for applications in orthopedic radiology developed in collaboration between Carestream Health and Johns Hopkins University. Our research investigates a new generation of high-resolution x-ray detectors – CMOS detectors – to enhance the spatial resolution of extremity CBCT and enable imaging of the fine microstructure of human bone in patients in vivo. The insets compare the visualization of a detail of trabecular architecture using CMOS-based CBCT and the gold standard micro-CT. The micro-CT technology is only available for imaging of small animals and laboratory samples, whereas our approach will be applicable in human patients.
Qian Cao, a PhD student in the department of biomedical engineering at Johns Hopkins University in Baltimore, and colleagues describe a novel system using complementary metal-oxide semiconductor (CMOS) detectors to enhance resolution of extremity cone beam CT (CBCT) to ∼0.1 mm, enabling morphological analysis of trabecular bone. Because the CMOS detector provides very high spatial resolution, it can detected finer details than conventional CT imaging or the current generation of extremity CBCT that utilizes flat-panel detectors (FPDs). He explained that this type of system could be used in a physician’s office as well as a radiology department due to its portability and very low dose volumetric imaging.
In his presentation, Cao explained that the research team implemented cascaded systems models of CMOS- and FPD-based extremities CBCT. They compared performance for a range of pixel sizes (0.05-0.4 mm) and x-ray techniques (0.05-0.8 mAs/projection) using detectability of high-low-, and all-frequency tasks for a non prewhitening observer. They compared metrics of bone morphology obtained using CMOS-based CBCT with the metrics of the FPD-based system in the hand of a human cadaver.
The researchers determined that CBCT/CMOS provided results that correlated with micro-CT, the gold standard for assessing trabecular bone. Compared to FPD CBCT, the CMOS detector yielded improved delineation of the trabeculae and improved correlation with micro-CT in measurements of bone volume (correlation coefficient of 0.88 vs 0.57 for FPD-CBCT) and trabecular spacing (correlation coefficient of 0.85 vs 0.63 for FPD-CBCT).
The advantage of this new system in development is that micro-CT can only be used with bone samples from biopsies, whereas this system can quantitatively perform in vivo imaging of trabecular bone.
“The technology we are developing allows us to see very fine detail in the mesh-like microstructure of bone which currently can’t be assessed in patients,” said project leader Wojceich B. Zbijewski, PhD, a medical physicist and instructor in the department of biomedical engineering. “This could help us detect bone diseases in their initial stages and help with development of new preventive therapies. For example, there is growing evidence that early stages of osteoarthritis involve changes in trabecular bone, so if we can detect such change, a patient could potentially avoid painful knee replacement surgery by getting treatment before the cartilage was irreversibly damaged.”
The research team anticipates beginning the first studies of CBCT/CMOS in patients in 2017.
