Dialysis-related Amyloidosis
By Li T, Patel S, Marin H, Griffith B





Case Summary
A elderly patient with a history of end-stage renal disease requiring hemodialysis, hepatocellular carcinoma, and bilateral carpal tunnel syndrome presented with generalized neck pain, new extremity weakness, and numbness. The history of malignancy and new symptoms prompted imaging of the spine to assess for metastatic disease. Relevant laboratory values included negative serum workup for multiple myeloma and normal parathyroid hormone (PTH) levels.
Imaging Findings
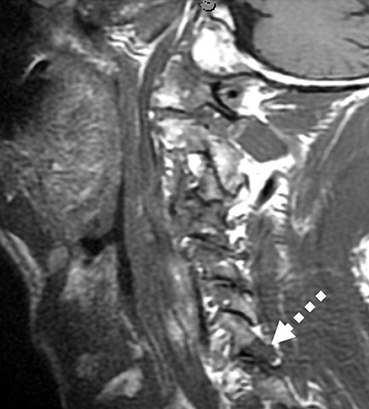
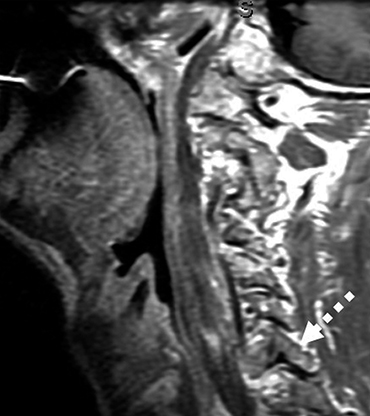
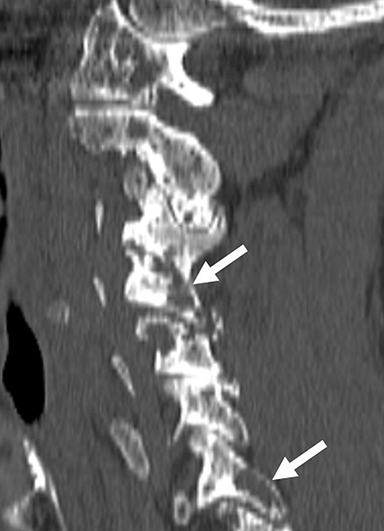
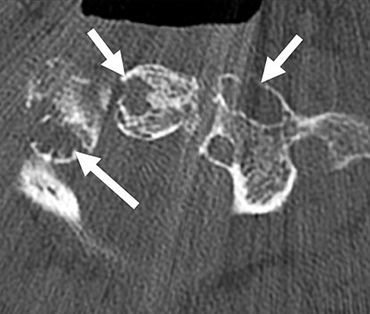
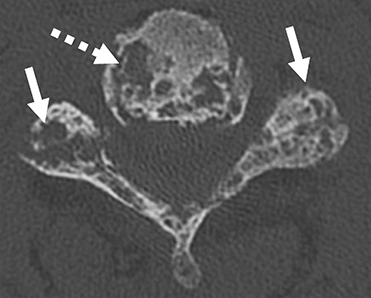
Magnetic resonance imaging (MRI) of the cervical spine demonstrated multiple T1 hypointense, contrast-enhancing lesions, including within the dens, C1 lateral mass, and C7 facet, along with periodontoid T1 hypointense soft tissue (Figure 1). Concern for metastatic disease in the setting of hepatocellular carcinoma prompted computed tomography (CT) of the cervical spine. The images demonstrated numerous lucent lesions throughout the cervical spine, including within the anterior arch of C1, the C2 vertebral body, and odontoid process. Lucent lesions also involved the endplates, facet joints, and posterior elements at multiple levels (Figure 2).
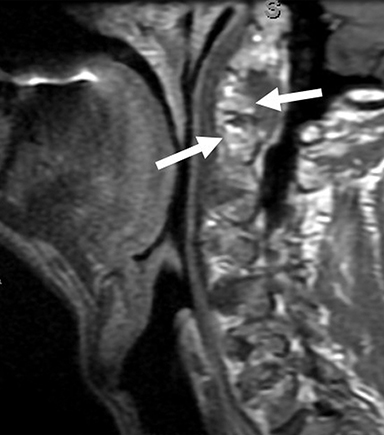
These findings were not previously present and raised suspicion for osseous metastatic disease. Further review of imaging revealed a large, well-circumscribed lytic lesion within the right humeral head with an associated pathologic fracture (Figure 3).
Subsequent bone marrow aspirate found no evidence for multiple myeloma or other plasma cell dyscrasia. The patient underwent biopsy of the lytic lesion involving the humerus, which revealed positive Congo red staining with polarization.
Diagnosis
Dialysis-related amyloidosis.
Differential diagnosis includes osseous metastatic disease, multiple myeloma, osteoarthritic degenerative changes, infectious spondylodiscitis, hyperparathyroidism, rheumatoid arthritis or calcium pyrophosphate deposition disease.
Discussion
Dialysis-related amyloidosis (DRA) is a unique subtype of amyloidosis occurring in patients undergoing long-term hemodialysis. The pathogenesis is not completely understood, but it is thought to be related to progressive deposition and accumulation of β 2-microglobulin as amyloid fibrils, within the periarticular tissues, synovium and bone.1-3
DRA invariably affects the musculoskeletal system, with the most common sites of osseous involvement being the wrists, hips, knees, and spine.1,4 Deposition in the wrists commonly causes carpal tunnel syndrome, as seen in this case.4,5 The most common manifestation in the spine is that of destructive spondyloarthropathy, which is characterized by erosive and cystic endplate changes, severe intervertebral disc space narrowing, and minimal osteophyte formation.6
Vertebral collapse, subluxation, or spondylolisthesis may occur with disease progression.1,6 The lower cervical spine is most frequently affected, with occasional involvement of the thoracic and lumbar spine, and rarely, involvement of the occipitoatlantoaxial region.1,6
Osseous involvement appears on conventional radiographs as radiolucent lesions of variable size in the medullary and cortical bone, with cortical destruction and fine sclerotic margins.2 Radiographs can also show periarticular soft tissue masses with erosive changes, joint destruction, or subluxation.1
Computed tomography of destructive spondyloarthopathy demonstrates disc-space loss with endplate erosions, irregularity, and sclerosis.6 Compared to radiography, CT is much more sensitive for detection of smaller areas of osteolysis in cortical bone, and superior for assessment of disease distribution.1 CT is also helpful for demonstrating erosive and cystic changes in the occipitoatlantoaxial region, as well as abnormal periodontoid soft-tissue masses, as seen in this case.6
Amyloid deposits on MRI are T1 hypointense with variable T2 signal; approximately 50% of deposits demonstrate increased T2 signal intensity, depending on the volume of amyloid deposit versus fluid.7 These lesions typically enhance following gadolinium administration.2,8 MRI can also demonstrate amyloid deposits in the intervertebral disc, the synovium of the apophyseal joints, and the ligamentum flavum.1
DRA-associated destructive spondyloarthropathy can appear similar to advanced osteoarthritic degenerative disc disease and spondylodiscitis. A key differentiator from typical osteoarthritic degenerative change is the minimal osteophyte formation relative to the degree of disc-space loss.6,9 MRI is helpful in differentiating from infectious spondylodiscitis, with the absence of a paraspinal mass and lack of T2 high signal making infectious etiologies less likely.1,6 It is also important to note that most patients with DRA will also have concurrent osteoarthropathy of the hands and wrists, which may help solidify the diagnosis.8
The extensive poly- and periarticular involvement of the cervical spine in this case, with numerous cystic and lytic lesions involving the atlantoaxial region and odontoid process, endplates, facets, and posterior elements, is an uncommon manifestation of DRA. Nevertheless, radiologists should be aware of this pattern, as it can be easily mistaken for osseous metastatic disease, multiple myeloma or, in the setting of end-stage renal disease, brown tumors resulting from secondary hyperparathyroidism.1 However, these processes will not have the periarticular predilection seen in DRA.1
Ultimately, correlating laboratory values such as PTH levels and serum and urine monoclonal proteins may be necessary to exclude other diagnoses. Increased serum B2-microglobulin levels are not helpful in establishing a diagnosis of DRA, as levels are comparable between dialysis patients with and without DRA.10 Definitive diagnosis o is achieved with biopsy and immunohistologic analysis demonstrating positive Congo red staining and green birefringence under polarized light.1
Treatment with high-flux dialysis membranes, hemofiltration, immunoadsorption, as well as renal transplantation, is targeted at reducing B2-microglobulin deposition. Transplantation, however, will not cause regression of the osseous lesions.3,7
Conclusion
Amyloidosis remains an important consideration in the differential diagnosis of lytic lesions of the spine of patients undergoing hemodialysis. While typical DRA-related destructive spondyloarthropathy manifests at the intervertebral discs and endplates, more extensive patterns of involvement can mimic other disease processes such as multiple myeloma and metastatic disease.
References
- Kiss E, Keusch G, Zanetti M, et al. Dialysis-related amyloidosis revisited. AJR Am J Roentgenol. 2005;185(6):1460-1467.
- Lee KS, van Holsbeeck MT, Abbud A. Atypical rapid progression of osteoarticular amyloidosis involving the hip in a patient on hemodialysis using polyacrylonitrile mem
- branes. Skeletal radiol. 2010;39(1):79-83.
- Jadoul M. Dialysis-related amyloidosis: importance of biocompatibility and age. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association - European Renal Association. 1998;13 Suppl 7:61-64.
- Danesh F, Ho LT. Dialysis-related amyloidosis: history and clinical manifestations. SemDdialysis. 2001;14(2):80-85.
- Daly KE, Kavannagh TG. Bone cyst in the cervical spine due to secondary amyloidosis. A case report. Acta Orthop. Scand. 1992;63(2):221-222.
- Theodorou DJ, Theodorou SJ, Resnick D. Imaging in dialysis spondyloarthropathy. SemDialysis. 2002;15(4):290-296.
- Nangaku M, Miyata T, Kurokawa K. Pathogenesis and management of dialysis-related amyloid bone disease. Am J Med Sci. 1999;317(6):410-415.
- Otake S, Tsuruta Y, Yamana D, Mizutani H, Ohba S. Amyloid arthropathy of the hip joint: MR demonstration of presumed amyloid lesions in 152 patients with long-term hemodialysis. EuroRadiol. 1998;8(8):1352-1356.
- Weinfeld A, Stern MH, Marx LH. Amyloid lesions of bone. Am J Roentgenol Rad Ther. , Nuc Med. 1970;108(4):799-805.
- Kazama JJ, Yamamoto S, Takahashi N, et al. Abeta-2M-amyloidosis and related bone diseases. J Bone Min Metab. 2006;24(2):182-184
Affiliations: Henry Ford Hospital, Detroit, MN.
