Fenestral otosclerosis
Images

CASE SUMMARY
A 57-year-old female presented with a longstanding history of left-sided hearing loss that progressively worsened over the previous year with intermittent otalgia and superimposed subjective non-pulsatile tinnitus. Audiologic evaluation was notable for mixed conductive and sensorineural hearing loss on the left. Temporal bone CT imaging demonstrated resorptive changes along the margins of the oval window and cochlear promontory on the left with capsular sparing on the right compatible with clinically suspected fenestral otosclerosis. Due to the low-level gap in air/bone conduction at diagnosis, the patient was not deemed a surgical candidate for stapes replacement and referral was made for fitting of external audiological aid.
IMAGING FINDINGS
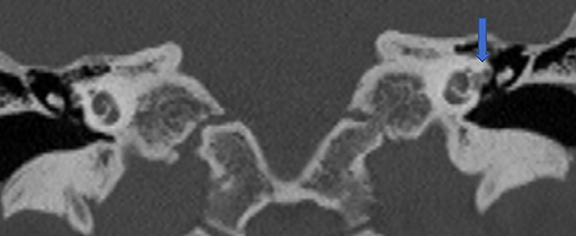
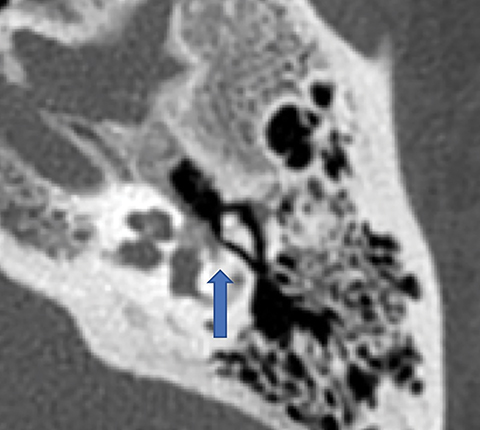
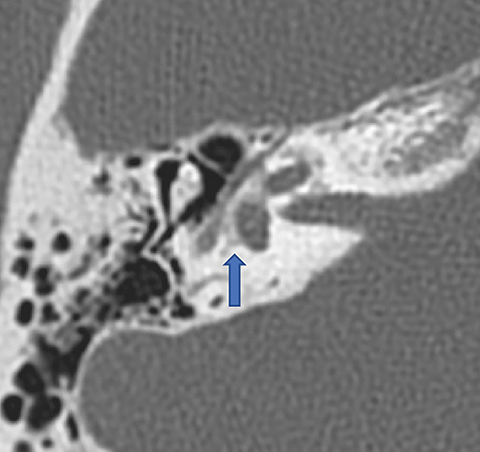
Temporal bone noncontrast CT imaging demonstrated resorptive changes along the cochlear promontory of the left otic capsule (Figures 1-3). This pathology lies in the area of the left fissula ante fenestram, which is consistent with fenestral otosclerosis. The contralateral otic capsule demonstrates the normal dense appearance of endochondral bone.
DIAGNOSIS
Fenestral otosclerosis
DISCUSSION
Affecting fewer than 1% of the U.S. adult population, otosclerosis is a primary degenerative idiopathic osteodystrophy of the osseous otic capsule that most commonly affects Caucasians in young to middle adulthood. Though the etiology remains obscure, a familial genetic predisposition has been observed with an autosomal dominant transmission displaying incomplete penetrance.1 Clinically, early otosclerosis causes conductive hearing loss. This is later admixed with sensorineural hearing loss due to disease progression.2 Histopathologically, the normally dense endochondral bone of the otic capsule is initially replaced by islands of vascular, demineralized Haversian bone that gradually becomes osteosclerotic over time. This osseous resorption has also given rise to the alternative term “otospongiosis” for the early disease phase. Initial, or fenestral, otosclerosis occurs in the area of the fissula ante fenestram, a vestigial embryonic cleft anterior to the oval window and stapes, and typically progress to involve the cochlear promontory, vestibule and otic capsule. 3,4 Involvement of the stapes footplate at the oval window leads to early conductive hearing loss via annular ligament ankylosis. With disease progression, otodystrophic damage of the cochlea results in generalized retrofenestral or cochleariform otosclerosis. The end sequelae are mixed sensorineural and conductive hearing loss with possible superimposed pulsatile tinnitus.3
Diagnosis of otosclerosis is based on a composite of clinical, audiological, and imaging findings, with radiology playing an ever-increasing role, not only in initial disease detection, but also for surgical planning and complication assessment. Typical clinical findings include the otoscopic Schwartz sign, constituted by a visible pink tinge at the cochlear promontory due to neovascular osseous changes.3,4 High-resolution, noncontrast CT imaging (HRCT) utilizing sub-millimeter slice acquisition with isotropic multiplanar reconstruction is the imaging modality of choice. Fenestral otosclerosis findings on HRCT include ill-defined osseous lucency typically centered at the oval window and cochlear promontory (Figures 1-3). Generalized otic demineralization is seen in more advanced cochleariform disease (Figure 4). Differential diagnostic considerations are limited, and they include otosyphilis, Paget’s disease and osteogenesis imperfecta.4
Meta-analyses have shown wide variability in the metrics of HRCT diagnosis of otosclerosis with more recent reports supporting collective sensitivities of over 90% for early fenestral involvement.4,5 Several studies have shown added utility in the use of semi-automated histogram analysis of CT bone density datasets as well as specialized multiplanar reconstructions paralleling the stapes crus for the detection of very early histopathological changes.6,7
Various imaging-based grading systems for otosclerosis have been proposed without universal acceptance. A three-tier grading system corresponding respectively to isolated fenestral involvement, progressive localized cochlear extension, and generalized otic disease is commonly used; both inter- and intraobserver interpretative agreement have been shown to be consistently high for this grading system.8 Otosclerosis is managed both medically and surgically, with oral fluorides having shown proven efficacy at slowing sensorineural hearing loss.3,9 Fenestral otosclerosis is most commonly treated with stapedectomy and prosthesis insertion, while more advanced cochleariform disease is often managed with direct cochlear implantation. 10 Higher grades of disease extent and lower Hounsfield densities correspond to increased audiologic air and bone conduction thresholds for hearing stimulation, as well as an increased incidence of stapes footplate complications at time of surgery. Furthermore, resorption of the osseous covering of the superior semicircular canal has been shown to be an independent contraindication to stapes prosthesis placement.2 Increasingly, HRCT temporal imaging assists in cochlear versus stapes implant stratification plans and serves an invaluable role in planning the surgical approach to otosclerosis.4
CONCLUSION
In summary, HRCT imaging of the temporal bone plays an ever-broadening role not only in the initial diagnosis of otosclerosis, but also in treatment planning. Manifesting initially in the so-called fenestral phase with resorptive changes at the level of the oval window, otosclerosis progresses over time to involve the cochlear promontory and otic capsule. Sclerotic overgrowth may be seen with more advanced cases, commonly resulting in narrowing of the oval window and fixation of the stapes footplate. Clinically, patients initially present with conductive hearing loss. This progresses to mixed sensorineural hearing loss as the otic capsule is increasingly affected. Advanced disease findings on HRCT have been shown to correlate independently with both surgical treatment failure and increased rates of postoperative complications.
REFERENCES
- Rudic M, Keogh I, Wagner R, et al. The pathophysiology of otosclerosis: Review of current research. Hear Res. 2015;330(Pt A):51-56.
- Whetstone J, Nguyen A, Nguyen-Huynh A, et al. Surgical and clinical confirmation of temporal bone CT findings in patients with otosclerosis with failed stapes surgery. AJNR. 2014; 35: 1195-1201.
- Purohit B, Hermans R, Op de beeck K. Imaging in otosclerosis: A pictorial review. Insights Imaging. 2014;5(2):245-252.
- Virk J, Singh A, Lingam R. The role of imaging in the diagnosis and management of otosclerosis. Otology and Neurotology. 2013; 34: e55-60.
- Lagleyre S, Sorrentino T, Calmels M, et al. Reliability of high-resolution CT scan in diagnosis of otosclerosis. Otology and Neurotology. 2009; 30: 1152-1159.
- Yamashita K, Yoshiura T, Hiwatashi A, et al. The radiological diagnosis of fenestral otosclerosis: the utility of histogram analysis using multidector row CT. Eur Arch Otorhinolaryngol. 2014; 271: 3277-3282.
- Mori N, Toyama Y, Kimura N, et al. Detection of small fenestral otosclerotic lesions by high-resolution computed tomography using multiplanar reconstruction. Auris Nasus Larynx. 2013; 40: 36-40.
- Lee TC, Aviv RI, Chen JM et-al. CT grading of otosclerosis. AJNR. 2009;30 (7):1435-1439.
- Cureoglu S, Baylan MY, Paparella MM. Cochlear otosclerosis. Curr Opin Otolaryngol Head Neck Surg. 2010;18(5):357-362.
- Burmeister J, Rathgeb S, Herzog J. Cochlear implantation in patients with otosclerosis of the otic capsule. Am J Otolaryngol. 2017;38(5):556-559.
Citation
T L, M R. Fenestral otosclerosis. Appl Radiol. 2018; (11):37-39.
November 8, 2018