High-grade Undifferentiated Pleomorphic Sarcoma
By Parikh P, Calvert AD, Mousa M, Kedar RP


CASE SUMMARY
A 51-year-old presented to the emergency department with a non-productive cough and intermittent hemoptysis of one-month duration. He had no significant medical history or comorbidities. Additional symptoms included progressive dyspnea, night sweats, and a 25-pound unintentional weight loss over the previous six months. The patient denied fever, recent surgery, long travel, history of blood clots, or family history of cancer. Physical examination was notable for decreased breath sounds in the right lower lung. Lab results demonstrated normocytic anemia but were otherwise unremarkable.
IMAGING FINDINGS
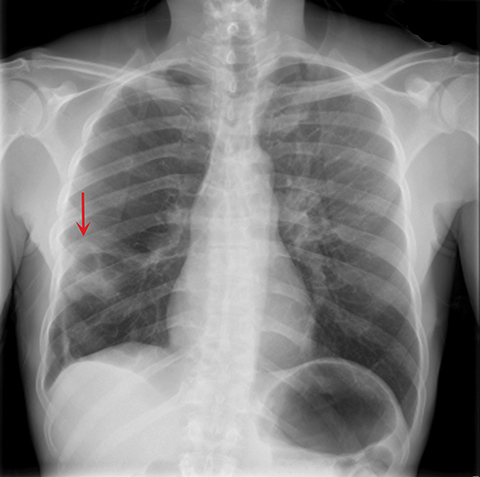
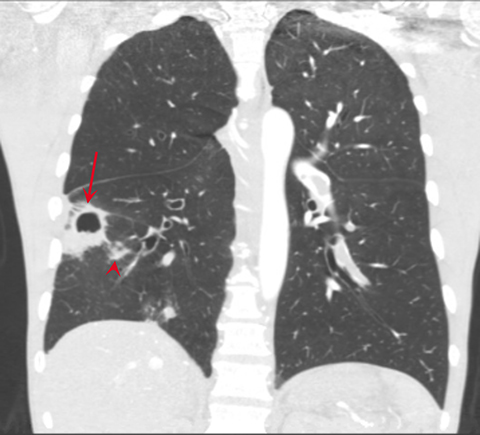
A frontal view chest x-ray showed a cavitary lesion with surrounding airspace consolidation in the right lower lobe (Figure 1). A CT angiogram of the pulmonary arteries was performed to evaluate the cavitary lesion. Axial and coronal images demonstrated a large low-attenuated intraluminal-filling defect within the pulmonary trunk and main pulmonary arteries with distal extension into the bilateral lobar and segmental arteries (Figure 2). The filling defect did not demonstrate obvious enhancement or extraluminal extension.
The right lower lobe contained a cavitary lesion with adjacent consolidative changes and a sub-centimeter noncalcified nodule medially (Figure 3). Initially diagnosed as a saddle pulmonary embolism with a pulmonary infarct, the patient was treated with anticoagulation.
Owing to a lack of improvement in the patient’s clinical status after several days of therapy, repeat imaging was performed, demonstrating unchanged low-attenuation filling defects involving the bilateral pulmonary arteries. Interventional mechanical thrombectomy was unsuccessful; however, the obtained tissue sample revealed a high-grade undifferentiated pleomorphic sarcoma.
DIAGNOSIS
High-grade undifferentiated pleomorphic sarcoma
DISCUSSION
Primary pulmonary artery sarcoma is a rare but aggressive malignancy with only a few hundred cases reported in the literature since first described by Mandelstamm in 1923.1,2 The tumor usually presents in middle-aged adults and is more prevalent in females. The vast majority of pulmonary artery sarcomas originate from the intimal layer of the pulmonary trunk and main pulmonary arteries. The predominant histologic subtypes are poorly differentiated intimal sarcoma and leiomyosarcoma.3,4
The typical presenting signs and symptoms of pulmonary artery sarcoma are nonspecific and include dyspnea, chest pain, hemoptysis, and cough. By the time patients develop symptoms, the disease is locally advanced or metastatic which, in combination with the tumor’s inherent aggressiveness, confers a poor prognosis. Owing to the rare incidence and nonspecific clinical manifestation, diagnosis of pulmonary artery sarcoma is often delayed for several weeks or months as a result of misinterpretation of imaging studies as showing pulmonary embolic disease or infection.2,3,4 Early diagnosis is critical since complete resection of the tumor is the standard of care. While overall prognosis is poor, early diagnosis and radical surgical resection provide the best means of prolonged survival.3,5
Clinical and radiological findings can overlap with thromboembolic disease; however, a pulmonary artery sarcoma is favored if a low-attenuation filling defect occupies the entire luminal diameter of a pulmonary artery with expansion of the involved artery and/or extraluminal tumor extension.6 In the absence of such findings and with failure to respond to anticoagulation therapy, particularly if patients present with constitutional signs/symptoms gadolinium-enhanced MRI is highly specific in detecting pulmonary artery sarcoma due to the heterogeneous enhancement of the tumor.7,8
In cases of subtle or equivocal tumor enhancement on MRI, 18FFDG PET/CT has demonstrated effectiveness in several limited studies and may be beneficial in the workup of suspected pulmonary artery sarcoma.4
CONCLUSION
Although pulmonary artery sarcoma is rare compared to pulmonary artery embolism, the diagnosis should be considered in atypical clinical and imaging presentations, as prompt diagnosis is essential for prolonged survival. Gadolinium-enhanced MRI has shown increased effectiveness in differentiating between bland thrombus and pulmonary artery sarcoma. In equivocal or atypical cases, 18FFDG PET/CT may provide further clarity.
REFERENCES
- Mandelstamm, M. Über primäre Neubildungen des Herzens. Virchows Arch. path Anat. 245, 43–54 (1923). https://doi.org/10.1007/BF01992097.
- Bendel EC, Maleszewski JJ, Araoz PA. Imaging sarcomas of the great vessels and heart. Semin Ultrasound CT MR. 2011; 32(5):377-404. PMID: 21963161.
- Huo L, Moran CA, Fuller GN, et al. Pulmonary artery sarcoma: a clinicopathologic and immunohistochemical study of 12 cases. Am J Clin Pathol. 2006; 125(3): 419-424. PMID: 16613346.
- von Falck C., Meyer B., Fegbeutel C., et al. Imaging features of primary sarcomas of the great vessels in CT, MRI and PET/CT: a single-center experience. BMC Med Imaging. 2013; 13:25. PMID: 23924063.
- Kruger I, Borowski A, Horst M, et al. Symptoms, diagnosis, and therapy of primary sarcomas of the pulmonary artery. Thorac Cardiovasc Surg. 1990. 38(2): p. 91-95. PMID: 2190350.
- Yi ES, Tumors of the pulmonary vasculature. Cardiol Clin. 2004; 22(3): p. 431-440, vi-vii. PMID: 15302362.
- Blackmon SH, Rice DC, Correa AM, et al. Management of primary pulmonary artery sarcomas. Ann Thorac Surg. 2009. 87(3): 977-984. PMID: 19231448.
- Rafal RB, Nichols JN.,Markisz JA. Pulmonary artery sarcoma: diagnosis and postoperative follow-up with gadolinium-diethylenetriamine pentaacetic acid-enhanced magnetic resonance imaging. Mayo Clin Proc. 1995; 70(2): 173-176. PMID: 7845042.
Affiliation: Department of Radiology, University of South Florida College of Medicine, Tampa, FL.
