Imaging Torus Lesions of Jaw Bones
Images


Torus is a common, benign exostosis of the jaw bones that develops in 5%-30% of the world population, with considerable variation in prevalence among different genders and racial or ethnic groups.1-5 This pathologic process usually manifests around puberty and continues to grow during adulthood. These lesions will then appear as lobulated protuberances on the lingual side of the jaw bones or hard palate.
Small torus lesions are usually asymptomatic and first noticed by the patient or detected incidentally during dental examination. Patients with larger tori, however, may experience longstanding symptoms including interference with proper mastication and oral hygiene, impaired speech, recurrent traumatic ulceration and inflammation of the gingival mucosa over the prominent tori, and ill-fitting dental appliances.
Larger tori can also cause a wide spectrum of other complications.
There have been reports of patients seeking advice from primary care physicians because of concern that an enlarging or ulcerated torus may represent a malignancy. Such cases can pose a diagnostic challenge to physicians who may not be well informed about the appearance and potential implications of this abnormality. Radiologists should be aware of the numerous potential manifestations and complications related to tori.
There are three major types of tori: torus mandibularis (TM), torus palatinus (TP), and torus maxillaris (TMAX).
Torus Mandibularis
On visual inspection, torus mandibularis (TM) appears as a multi-lobulated mass on the inner aspect of bicuspid and premolar regions, commonly with almost symmetrical extent on both sides. They typically measure 3-4 cm long, up to 1.5 cm thick, and are covered by intact gingival mucosa.
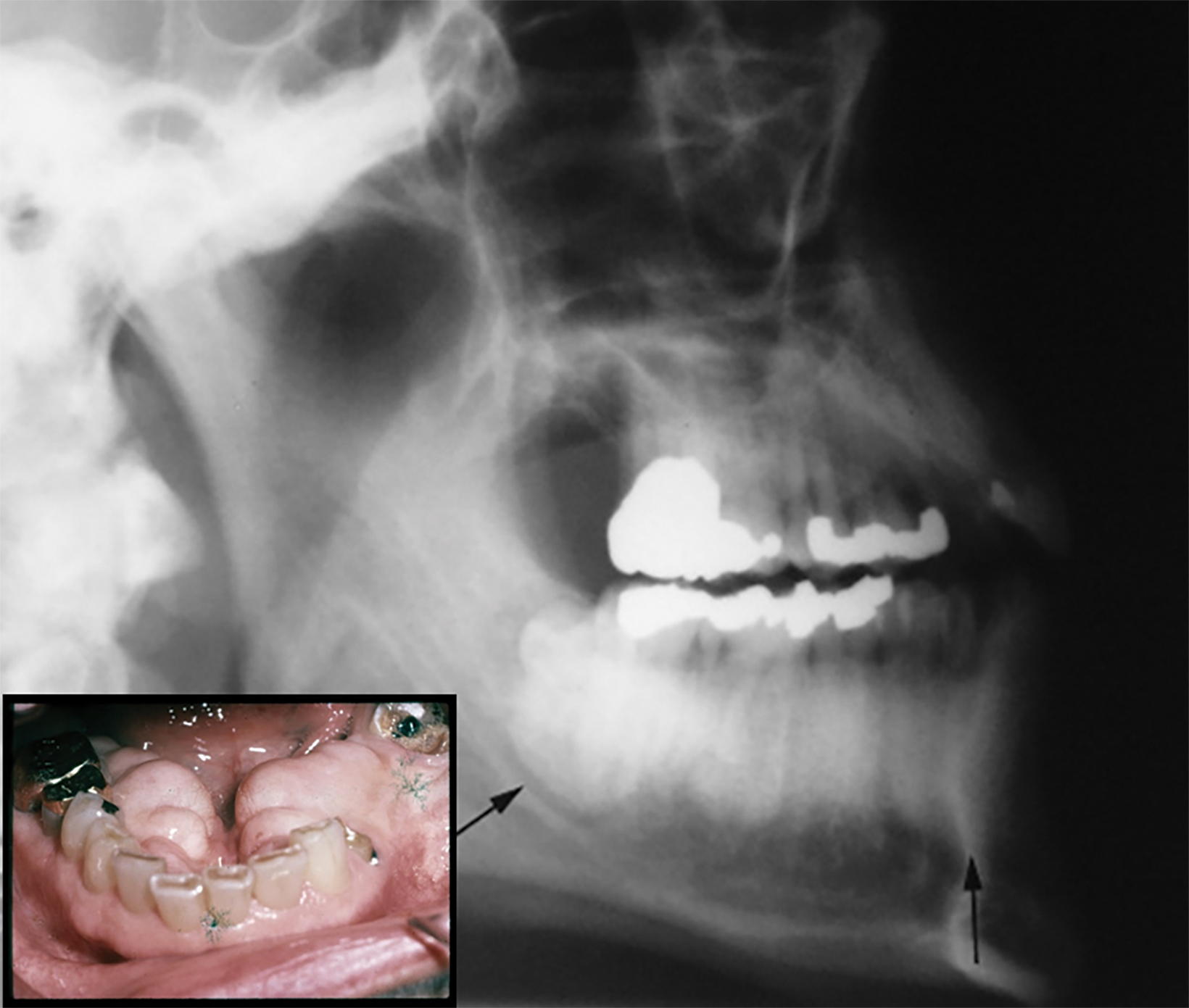
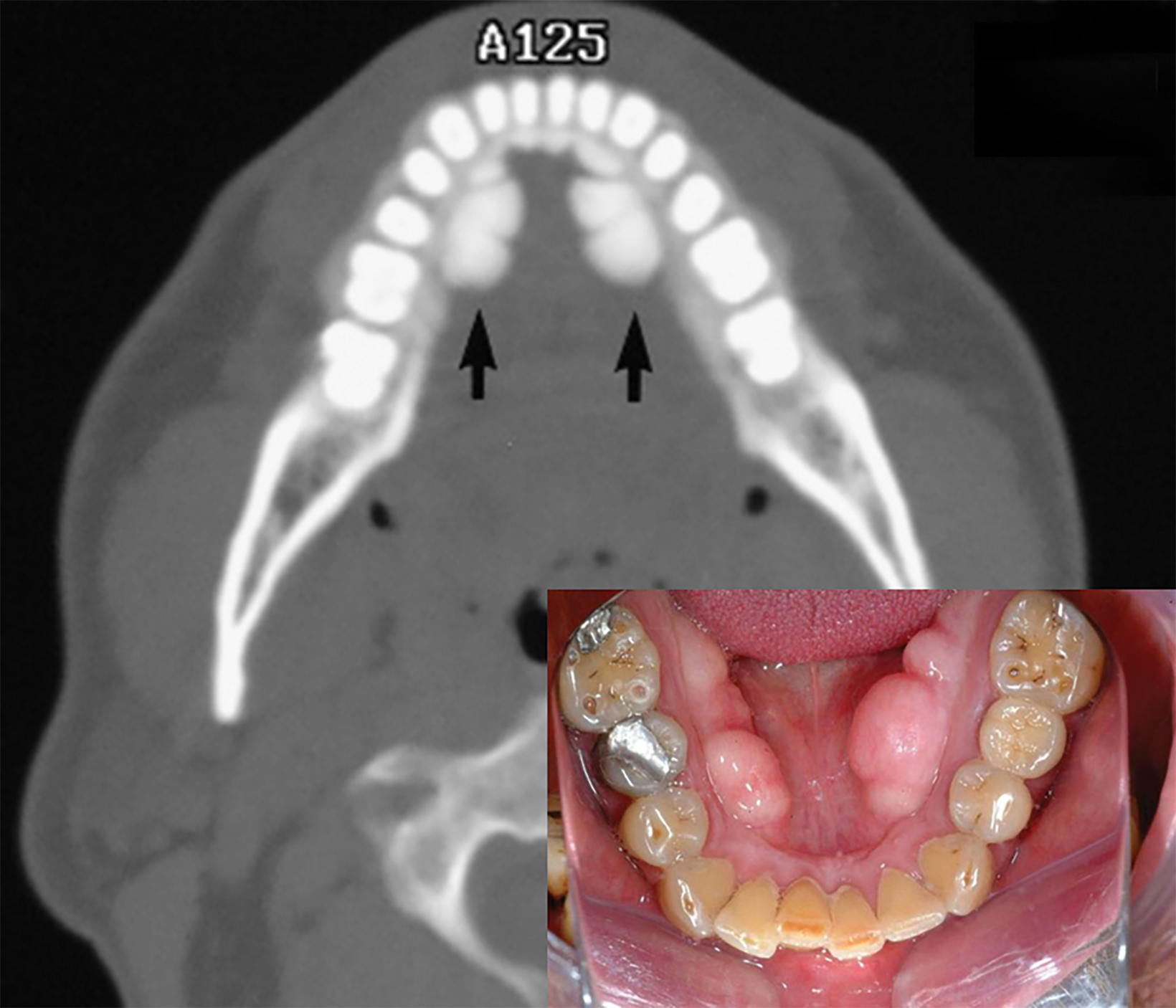
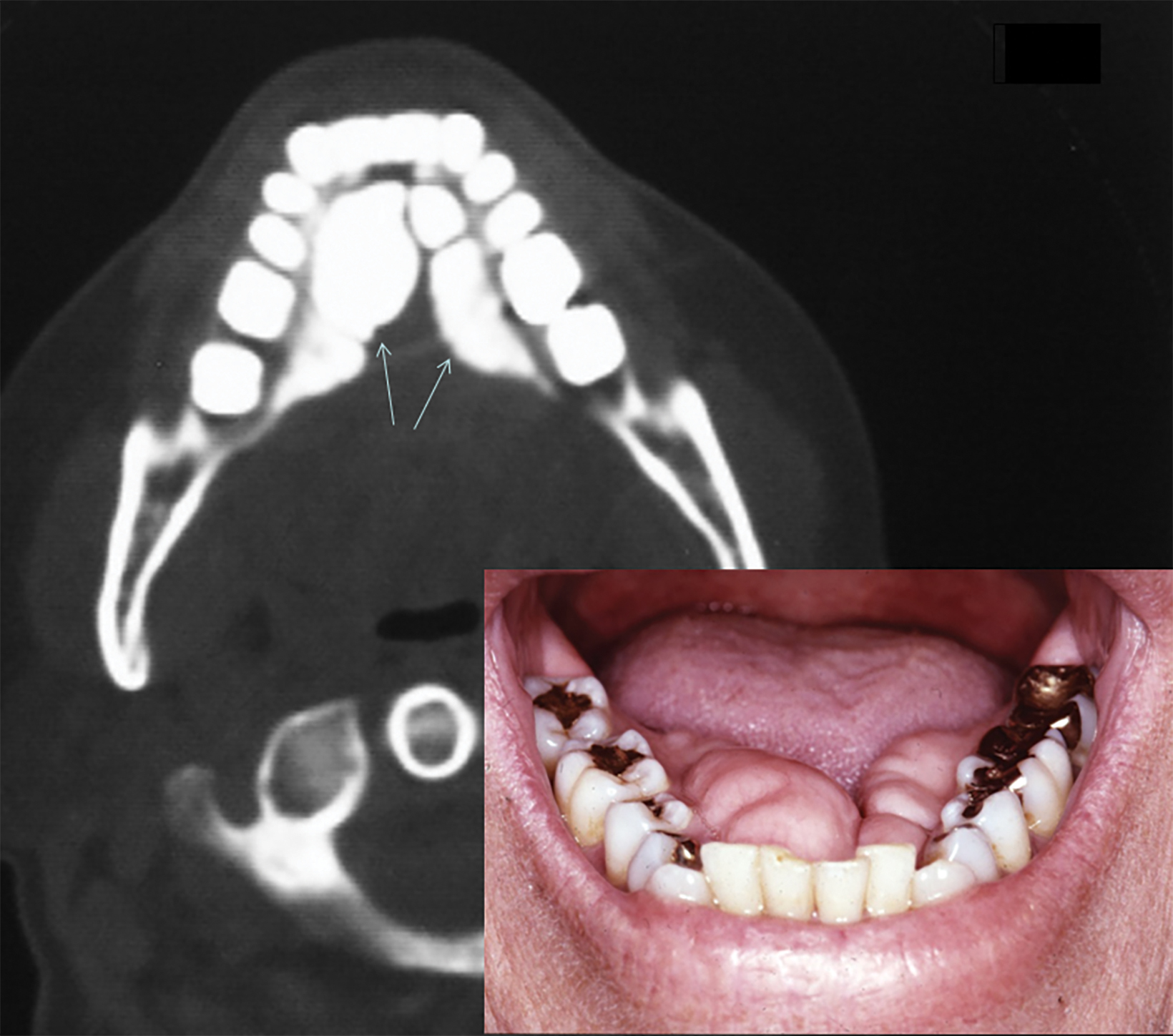
On lateral radiographs of the mandible, TM appears as a very dense sclerotic lesion or area of increased bone density superimposed on the roots of the lower teeth (Figure 1). Computed tomography (CT) demonstrates the TM as lobulated exophytic masses of cortical hyperostosis, located bilaterally above the mylohyoid line (Figures 2,3). The size and location of TM can cause posterior displacement of the tongue and interfere with speech.
Torus Palatinus
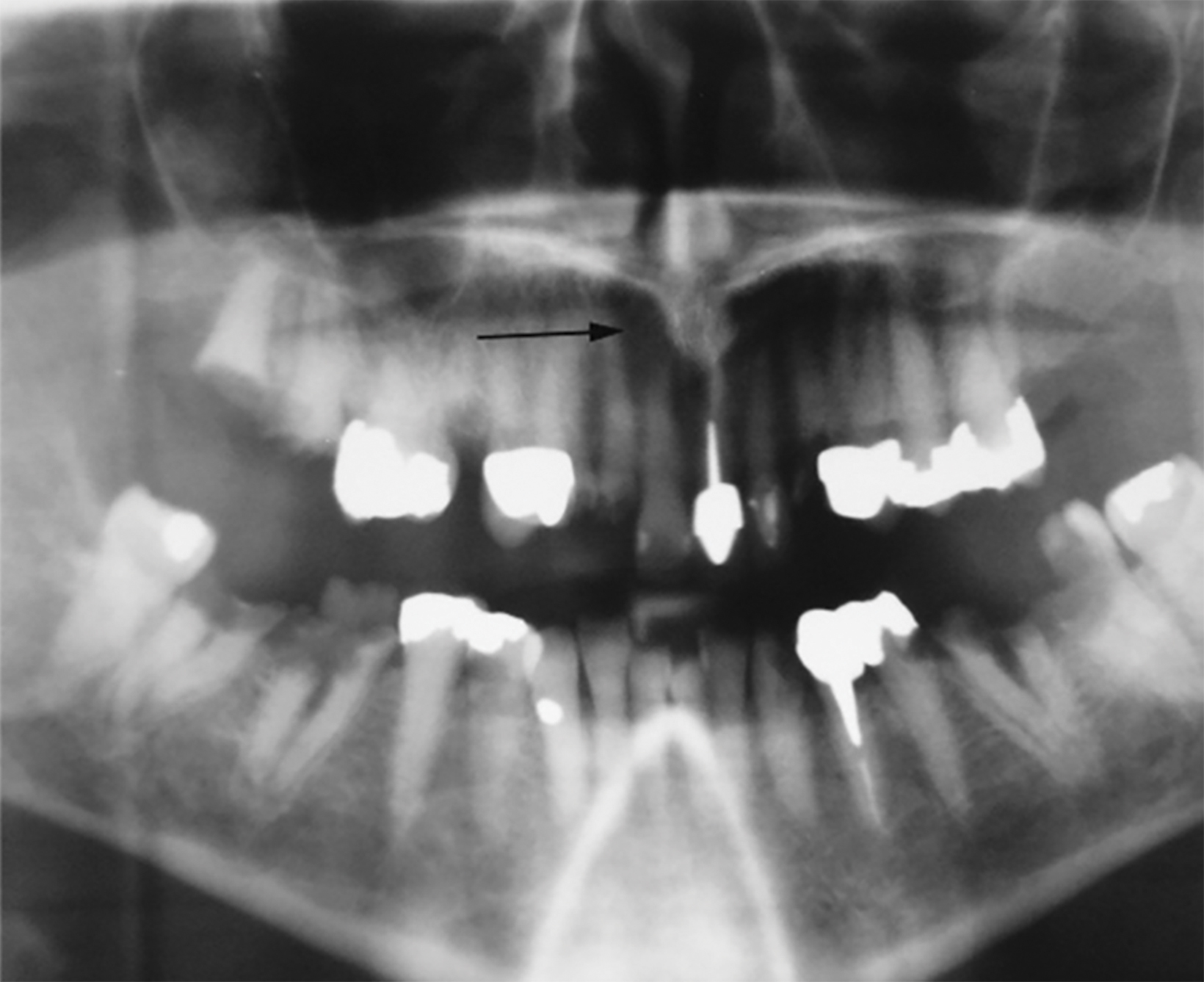
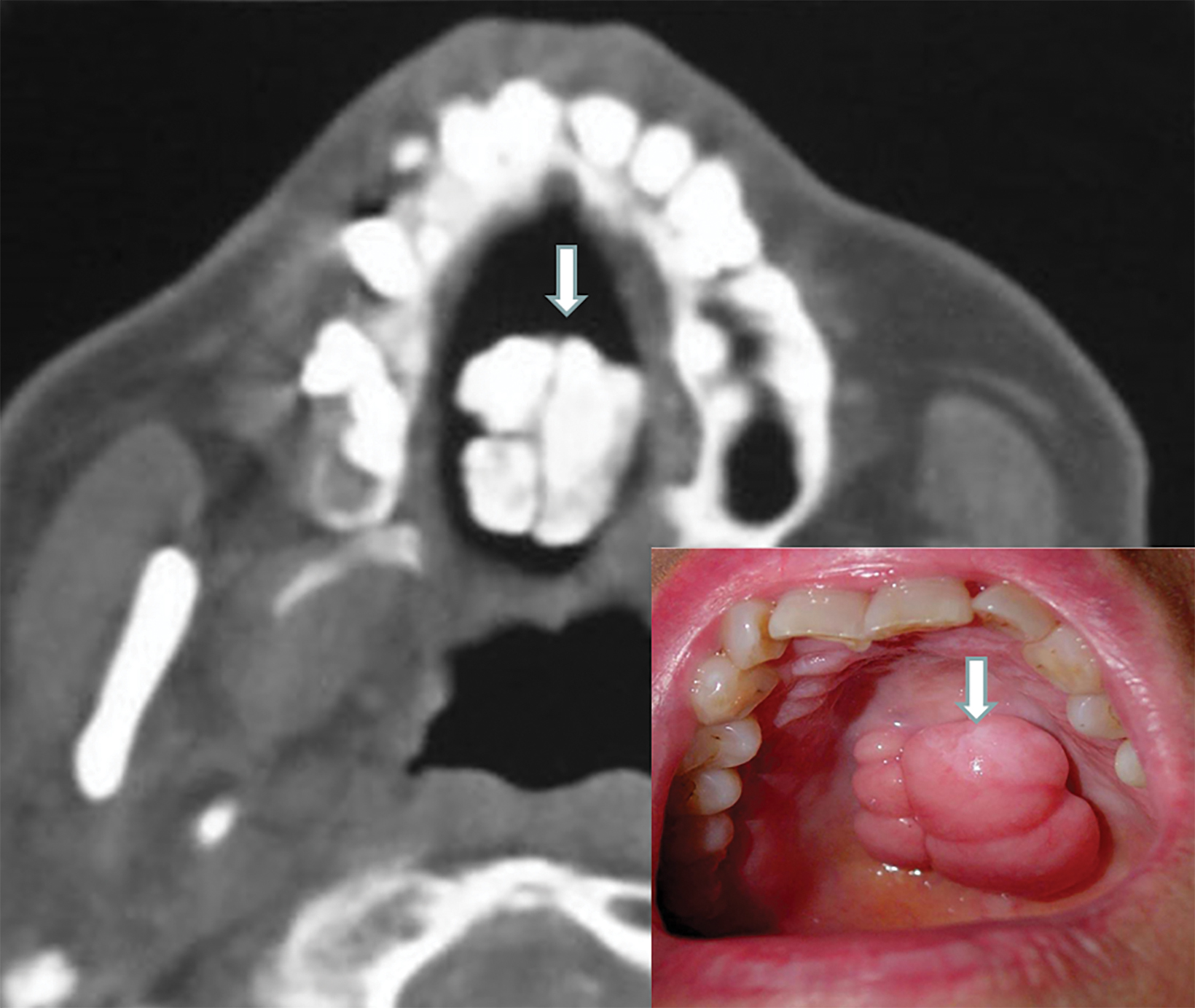
Torus palatinus (TP) manifests as a fungating mass of variable size and configuration that protrudes into the oral cavity from the center of the hard palate. The core of TP will appear as a dense and lobulated exostosis on radiographs and CT images (Figures 4,5). Intraoral inspection and photographs of larger lesions may reveal inflamed and ulcerated mucosa (Figure 6). Most patients will have experienced the same problem following repeated traumatic erosion by hard foods, such as candy. Therefore, surgical removal of a large TP by local osteotomy may be necessary to alleviate symptoms.
Torus Maxillaris
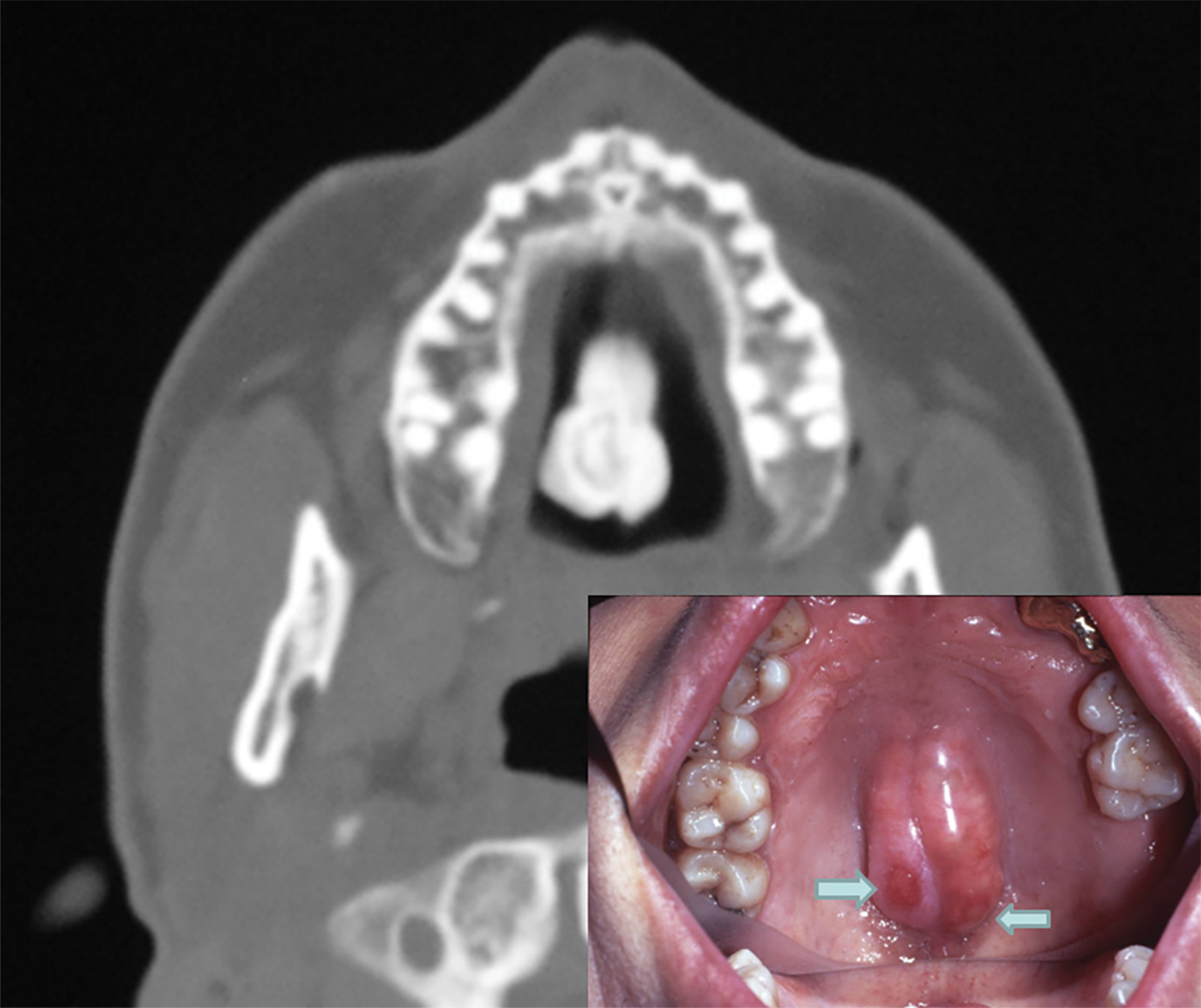
Torus maxillaris (TMAX) often appears bilaterally as prominent and lobulated masses arising from the medial aspects of the upper jaw. In contrast to TM, TMAX lesions are located more posteriorly along the molar regions. These tori are very firm and consist of marked cortical hyperostosis on CT sections (Figure 7).
On rare occasions a TMAX may be associated with a coexisting TP or other osseous abnormalities of the maxilla. We have anecdotally noticed that several patients with torus lesions had evidence of frontal hyperostosis on lateral radiographs of the skull. There are some similarities in the radiographic features of both conditions.
Etiological Considerations
Torus is a common benign exostosis that represents a developmental lesion, usually first appearing in puberty or early adulthood and becoming larger with advancing age. It has a hereditary etiology in about a third of cases. Curran, et al,6 found TM and TP in three generations of women in one family. In the study by Eggen,7 the genetic origin of TM was documented in 29.5% of patients. The remaining 70% were attributed to either environmental factors or mechanical issues caused by occlusal stress.4,5 Torus mandibularis and TMAX both have a predilection for developing adjacent to the teeth receiving local stress because of excessive teeth grinding and jaw clenching, also known as bruxism.4,5,8
Torus Prevalence and Manifestation
The most common age range at onset of torus is 10-30 years, but its growth may continue until the seventh decade of life.9,10 Tori prevalence varies with ethnicity and gender. One study of 448 female residents of Washington, DC, found tori present in 35% of African Americans, 38% of Asians, 32% of Caucasians, 30% of Hispanics, and 20% of Native Americans.2
Another investigation involving patients from the southern US revealed that 25% of Caucasian men and 24% of women had TM, whereas TMAX was present in 22% of men and 40% of women. In comparison, TM was present in 18% of African American men and 13% of African American women, while TMAX was present in 14% of African American men and 45% of African American women.1
A high incidence of tori has been reported among Asian populations. Morita and associates found TM in 58% of healthy students at Hiroshima University in Japan.11 Another study involving 1,520 dental patients in Thailand showed prevalence rates of 60.5% for TP, 32.2% for TM, and concurrent tori in 23.2%.12 Most published large series show female predominance for TP and a slight male predilection for TM.10,13
Clinical Presentation and Management
Most tori are asymptomatic and present as incidental findings during oral or dental examination. As they enlarge and become more prominent, however, tori may cause a wide spectrum of problems. These include interference with mastication and speech, compression and posterior displacement of the tongue, causing snoring or sleep apnea, and difficulty with placement and function of dental appliances, including dentures.14 Additionally, tori can promote plaque formation and periodontal disease because of food retention.3,8
Patients with large tori often experience recurrent ulceration and inflammation of the covering gingival mucosa from trauma induced during chewing and ingestion of hard food items (Figure 5). Prominent TP lesions may also interfere with endotracheal intubation during general anesthesia.15 There have been several reports concerning painful ulceration and osteonecrosis of torus in patients receiving bisphosphonate for treatment of osteoporosis.16
In some instances, larger, symptomatic tori may necessitate surgical removal.3,17 This procedure was performed in two of the illustrated cases (Figures 2,4). Indications for resection included interference with phonation or mastication, traumatic inflammation and ulceration, prosthetic instability, and in patients with disproportionate fear of malignancy.10 A potential use of an excised torus is as an autogenous bone graft in periodontal surgery and as an implant elsewhere.10,18
Although torus represents a common, well-recognized pathologic abnormality among dental professionals, the pathology has received scant mention in the medical literature. The lesion may be detected incidentally during routine radiological or physical examinations. Some patients may first seek medical advice because of concern for malignancy.
Although several causal factors have been postulated for the development of tori, their exact etiology in any individual patient may need further assessment. Radiologists familiarity with tori and their potential clinical complications can help assuage patient fears, improve diagnostic accuracy, and guide patient management.
References
- King DR, King AC. Incidence of tori in three population groups. J Oral Med. 1981; 36(1): 21-23.
- Chohayeb AA, Volpe AR. Occurrence of torus palatinus and mandibularis among women of different ethnic groups. Am J Dent. 2001; 14(5): 278-280.
- Gonsalves WC, Chi AC, Neville BW. Common oral lesions: Part II. Masses and neoplasia. Am Fam Physician 2007; 75: 509-512.
- Choi Y, Park H, Lee JS, et al. Prevalence and anatomic topography of mandibular tori: computed tomographic analysis. J Oral Maxillofac Surg. 2012; 70(6): 1286-1291.
- Sonnier KE, Horning GM, Cohen ME. Palatal tubercles, palatal tori, and mandibular tori: prevalence and anatomical features in a U.S. population. J Periodontol. 1999; 70(3); 329-336.
- Curran AE, Pfeffle RC, Miller E. Autosomal dominant osteosclerosis: report of a kindred. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999; 87: 600-604.
- Eggen S. Torus mandibularis: an estimation of the degree of genetic determination. Acta Odontol Scand. 1989; 47: 409-415.
- Morrison MD, Tamimi F. Oral tori associated with local mechanical and systemic factors: a case-control study. J Oral Maxillofac Surg. 2013; 71(1): 14-22.
- Bruce I, Ndanu TA, Addo ME. Epidemiological aspects of oral tori in a Ghanaian community. Int Dent J. 2004; 54: 78-82.
- Garcia-Garcia AS, Martinez-Gonzales JM, Gomez-Font R, etal. Current status of the torus palatinus and torus mandibularis. Med Oral Patol Oral Cir Bucal. 2010; 15(2): 353-360.
- Morita K, Tsuka H, Shintani T, et al. Prevalence of torus mandibularis in young healthy dentate adults. J Oral Maxillofac Surg. 2017; 75(12): 2593-2598.
- Jainkittivong A, Apinhasmit W, Swasdison S. Prevalence and clinical characteristics of oral tori in 1,520 chulalongkorn university dental school patients. Surg Radiol Anat.2007; 29(2): 125-131.
- Eggen S, Natvig B. Concurrence of torus mandibularis and torus palatinus. Scand J Dent Res. 1994; 102(1): 60-63.
- Ahn SH, Ha JG, Kim JW, et al. Torus mandibularis affects the severity and position-dependent sleep apnoea in non-obese patients. Clin Otolaryngol. 2019; 44(3): 279-285.
- Durrani MA, Barwise JA. Difficult endotracheal intubation associated with torus mandibularis. Anesth Analg. 2000; 90(3): 757-759.
- Godinho M, Barbosa F, Andrade F, et al. Torus palatinus osteonecrosis related to bisphosphonate: a case report. Case Rep Dermatol. 2013; 5(1): 120-125.
- Lee KH, Lee JH,Lee HJ. Concurrence of torus mandibularis with multiple buccal exostoses. Arch Plast Surg. 2013; 40(4):466-468.
- Ganz SD. Mandibular tori as a source for onlay bone graft augmentation: a surgical procedure. Pract Periodontics Aesthet Dent. 1997; 9: 973-982.
References
Citation
GG G, DR N, ZK G. Imaging Torus Lesions of Jaw Bones. Appl Radiol. 2022;(1):12-15.
January 6, 2022