Metastatic Pulmonary Calcinosis
By Jindal V, Towbin AJ, Morgan D, Towbin RB

Case Summary
A teenager with a history of antineutrophil cytoplasmic autoantibody (ANCA)-associated vasculitis, pulmonary hemorrhage, and renal failure presented with a mild chronic cough and superficial thrombophlebitis. At laboratory examination their calcium level was 10.4 mg/dL (normal 8.7-10.8 mg/dL) and serum phosphate was 9.8 mg/dL (normal 3.1-5.4 mg/dL).
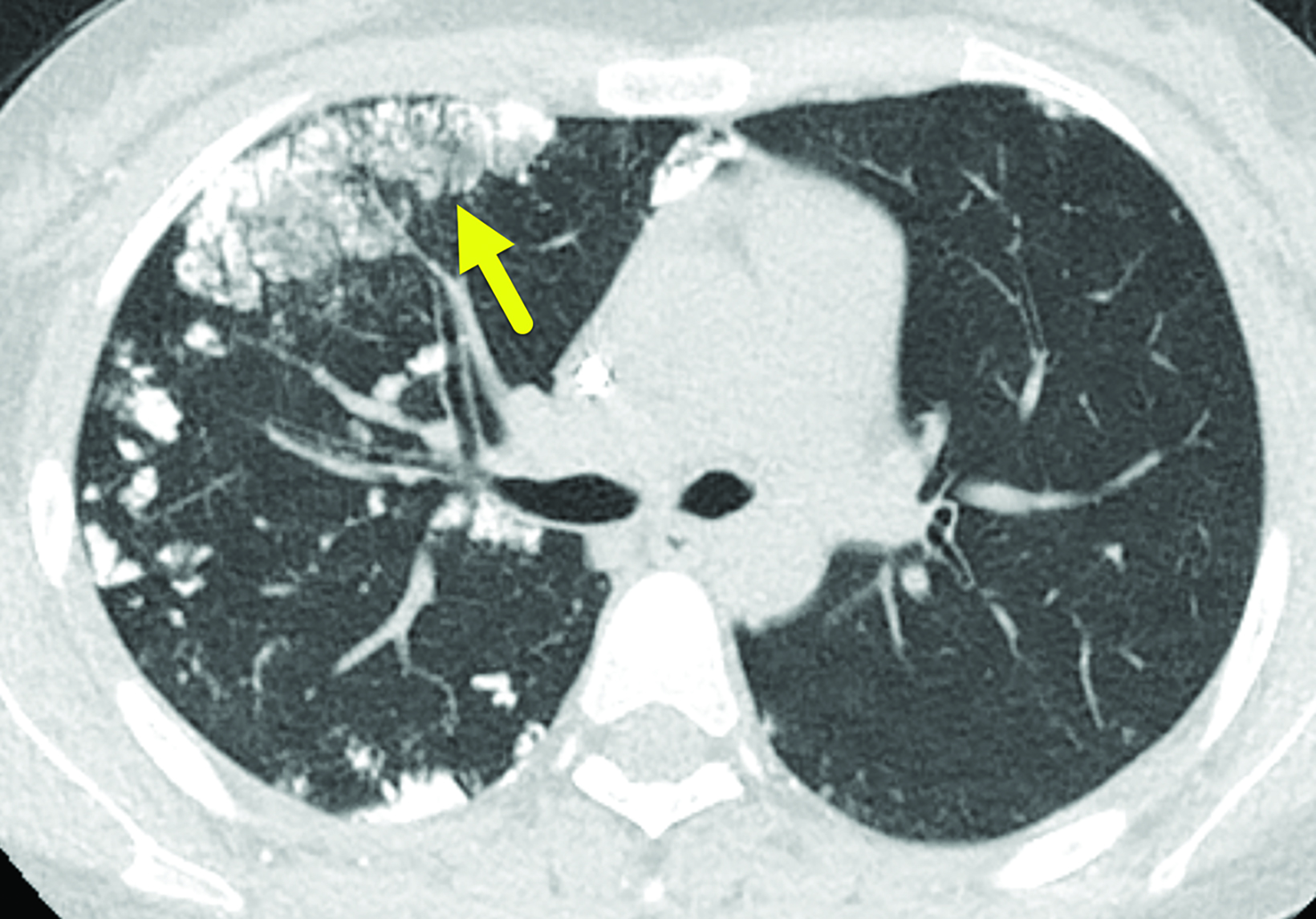
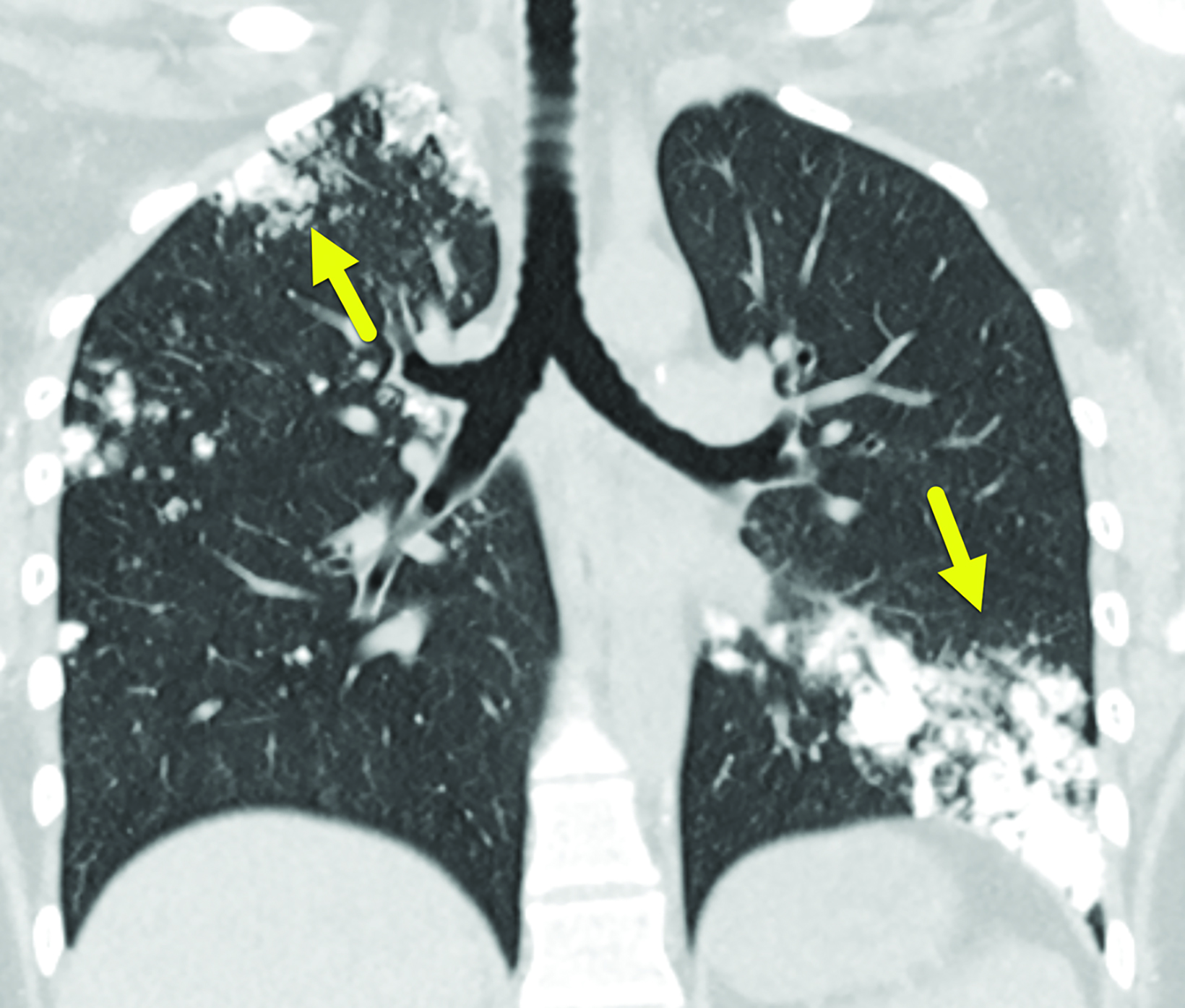
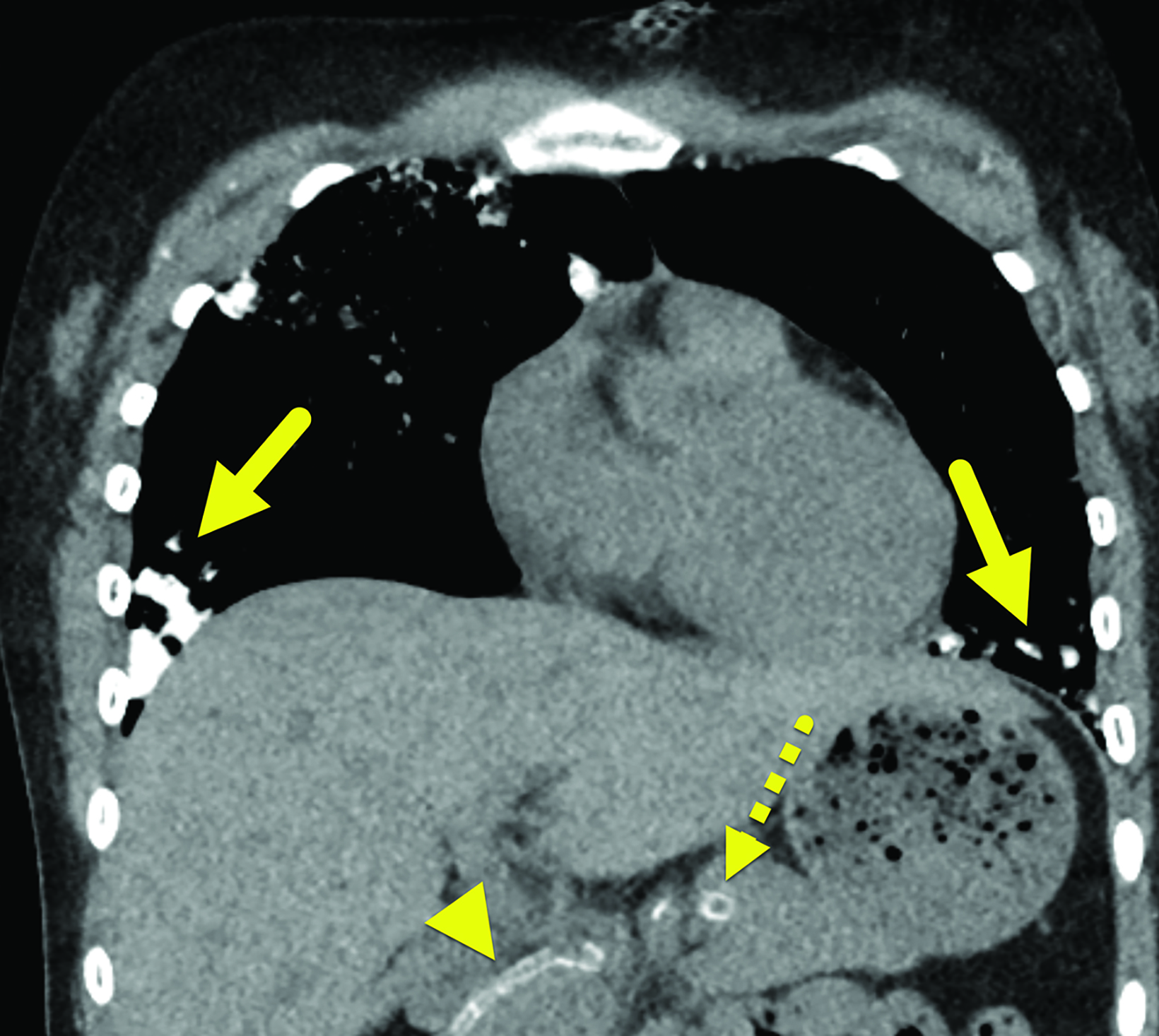
Imaging Findings
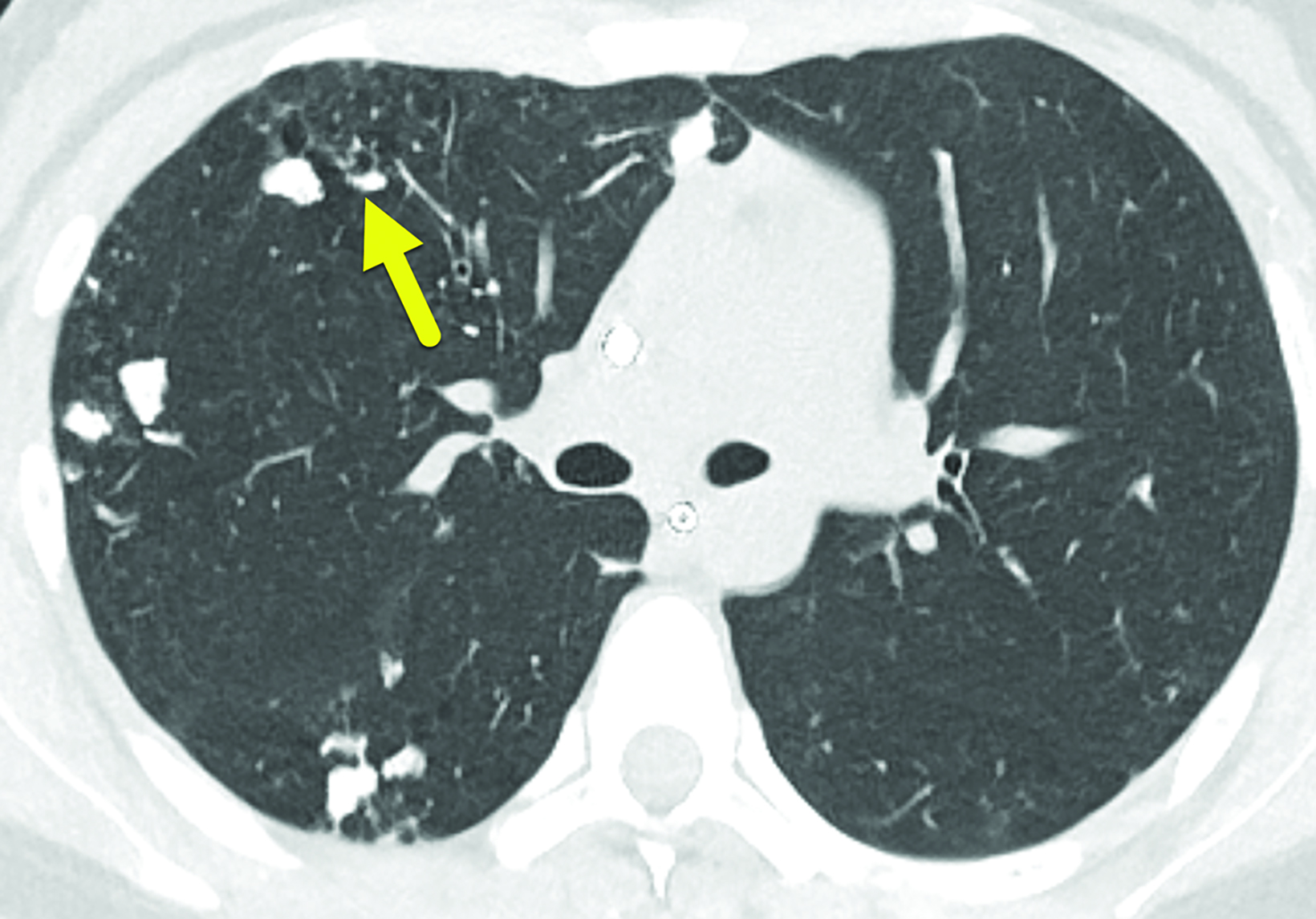
The initial CT scan (Figure 1) demonstrated extensive nodular opacities concentrated in a peripheral distribution throughout the lungs. The opacities had areas of increased density, which were that of calcification. Follow-up CT performed 18 months later (Fig- ure 2) showed improvement in the calcifications and development of cysts in areas of prior calcification.
Diagnosis
Metastatic pulmonary calcinosis secondary to renal failure. The differential diagnosis includes idiopathic pulmonary ossification, ossified pulmonary metastasis, chronic hemorrhagic conditions, infection, and inflammatory disorders.
Discussion
Metastatic pulmonary calcinosis (MPC) is a lung disease characterized by calcifications in the pulmonary parenchyma. It commonly occurs in patients with chronic renal failure. Studies have shown that 60 to 75% of patients on hemodialysis had MPC on autopsy yet were asymptomatic during life.1,2 While the diagnosis is relatively common in adults with chronic renal failure, it is rare in children and very few cases have been reported.3
Patients with MPC are usually asymptomatic but can report a chronic, nonproductive cough and respiratory distress. There is no association between the level of respiratory distress and the extent of calcifications.2,4,5
Metastatic calcification can occur in normal tissue when the calcium-phosphate product (serum Ca * serum P) is greater than 70 mg2/dL2 (normal < 40 mg2/dL2).2,5 This elevation occurs most often in patients with renal failure. While the calcium-phosphate product can be elevated in other conditions such as primary hyperparathyroidism, tumors, renal or liver transplantation, and following cardiac surgery, the level in these conditions is generally below 60 mg2/dL2 and MPC does not occur.2,6
Metastatic calcinosis can also affect the kidneys and stomach, although the lungs are the most commonly affected organs.1,2 They have an alkaline environment, as they secrete free hydrogen ion, allowing for the formation of calcium salts. The calcifications occur in the interstitium of the alveolar septa, the walls of the bronchioles, or large airways. The upper lobes are affected more often than the lower lungs, owing to the former’s higher ventilation/perfusion ratio, which leads to higher pH levels.4,6,7
Chest radiography is not sensitive to MPC. Most patients have normal radiographs owing to low levels of calcium deposition.2,4,8 In one study of seven patients with MPC, calcifications were visible on chest radiographs in only two and on CT in all seven.9 When visible on radiographs, the calcifications can appear as regions of consolidation.
High-resolution chest CT is preferred for diagnosing MPC.8 Three patterns have been described: diffuse or patchy areas of ground-glass opacity or consolidation; multiple diffuse calcified nodules; and confluent high-attenuation parenchymal consolidation. Of these, centrilobular ground-glass opacities that may contain foci of calcification are the most common.2,4,10 Other findings associated with MPC include calcification of the chest wall vessels, myocardium, bronchial wall, small pulmonary arteries, and the superior vena cava.2
Technetium 99m-methyl diphosphonate bone scintigraphy has shown to be effective for early detection of MPC. Affected lungs show regional increased radiotracer uptake.3,11 MPC can also be detected on MRI. On T1 images, MPC appears hyperintense compared to muscle and has a higher lesion/muscle signal intensity ratio compared to that of T2 images.2 Although MRI can show metastatic calcinosis, it is often not used because of its lower sensitivity for detection.
The pulmonary prognosis for most patients is good. The goal of treatment is to normalize serum levels of calcium and phosphate.2,6,8 Commonly used medications include bisphosphonates, phosphate binders, and vitamin D supplementation. In more advanced disease, parathyroidectomy, increased dialysis, or renal transplant may be considered.6,10 As calcium and phosphate levels normalize, calcium deposition in the lungs may decrease and pulmonary function may increase.2,6,10 This was the case in our patient.
Conclusion
Metastatic pulmonary calcinosis is a rare condition seen mostly in patients with renal failure. Affected patients are often asymptomatic but can develop respiratory distress. Diagnosis is typically made with chest CT, which demonstrates centrilobular ground-glass opacities that may contain foci of calcification. Treatment involves normalizing calcium and phosphate serum levels and possible surgical intervention.
