MRI for appendicitis in pediatric patients









Children with suspected acute appendicitis frequently undergo diagnostic imaging. Computerized tomography (CT) is a favored imaging modality in this clinical setting because of its accuracy and availability.1 CT provides both high sensitivity and specificity for the diagnosis of appendicitis.2 However, as the number of CT scan requests has increased, the medical community has raised concern about the potential risks associated with the inherent ionizing radiation exposure. Subsequently, the use of alternative modalities in children has increased.3 Ultrasound (US), for example, is favored by some physicians. In the hands of a skilled sonographer and with the appropriate patient, US is a good alternative to CT in diagnosing pediatric acute appendicitis.3 Of note, sonography’s sensitivity for appendicitis is less than CT’s4, and can be limited by operator dependence, patient body habitus, and sonographically obscure anatomic locations (retrocecal and deep pelvic regions).5 This combination of factors can result in equivocal or nondiagnostic ultrasound studies. A recent study found that ultrasound is indeterminate in 28% of cases.6
These limitations of CT and ultrasound have led to the introduction of MRI for the assessment of appendicitis in children.7-9 Many institutions have demonstrated MRI to be a reliable alternative to CT in the imaging diagnosis of appendicitis in children and adults.9-16 A pediatric-specific appendicitis MRI meta-analysis demonstrated a sensitivity of 96.5% and specificity of 96.1%, based on eleven studies in children.17 A meta-analysis of all published appendicitis MRI studies (including adults, pregnant patients, and children) also demonstrated a sensitivity and specificity of 96% and 96%, respectively, based on 30 studies.18 Additionally, favorable clinical outcomes, including time from initial clinical assessment to admission, time to antibiotic administration, time to appendectomy, and negative appendectomy rate have also been demonstrated in children at two institutions.9,19 Based on this growing body of evidence, MRI is a suitable alternative to CT in evaluating children for suspected appendicitis.
Technique
At our institution, a rapid, four-sequence, nonsedated, noncontrast MRI examination of the pediatric abdomen and pelvis has replaced CT and US in the emergent evaluation of children with suspected appendicitis. This protocol consists of axial and coronal T2 single-shot turbo spin-echo (SS-TSE) and axial and coronal T2 SS-TSE with fat saturation using spectral adiabatic inversion recovery (SPAIR) fat-suppression technique. While this protocol is more abbreviated than many other abdominal MRI examinations, the diagnostic performance and clinical outcomes validate the efficacy.9 Another recent clinical effectiveness study utilizing a similar protocol (unenhanced four-sequence T2 SS-TSE-based protocol) has also demonstrated excellent diagnostic performance in nonsedated children following equivocal ultrasound.15 At our institution we utilize 4-mm slices to cover the lung base through the pubic symphysis in the axial plane and mid liver to pubic symphysis on coronal images.
A recent systematic review of MRI in pediatric appendicitis drew the following four conclusions regarding pulse sequence selection:17
- SS-TSE is the crucial sequence for MRI appendicitis evaluation in children.
- While gadolinium-enhanced T1-weighted sequences may increase the radiologist’s degree of confidence in interpretation, the diagnostic performance is statistically similar and additional added value beyond noncontrast technique is not confirmed. Additionally, IV gadolinium increases cost and acquisition time.
- Diffusion weighted imaging (DWI) may be helpful and carries no significant added cost. However, DWI has not been included in patient outcome studies. If an institution chooses to use DWI, a b value of 500s/mm2 is suggested.
- Balanced steady-state free precession (bSSFP) sequences are often noncontributory.
Perhaps the most important aspect of a successful program is avoiding sedation. Initially, our target age range was children aged 5 to 17 years who could reasonably be expected to remain still in the MRI scanner for 15 minutes. However, we now often successfully image even younger children without sedation depending on their ability to cooperate. Nearly all patients 5 years and older, and selected younger patients may undergo evaluation with the above MRI protocol without sedation.17 Imaging without sedation has been validated by multiple institutions. 9,12,14,15,19,20
Image interpretation
Appendicitis
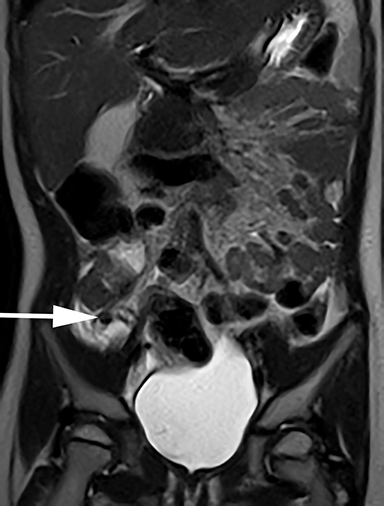
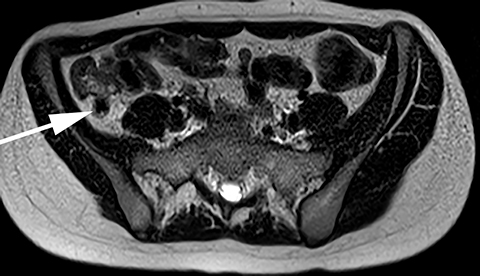
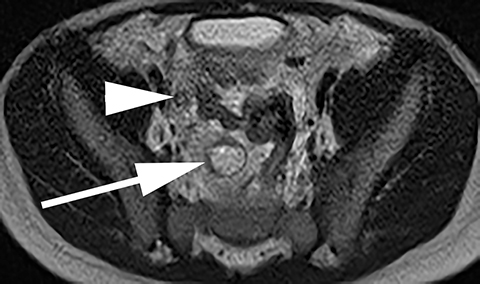
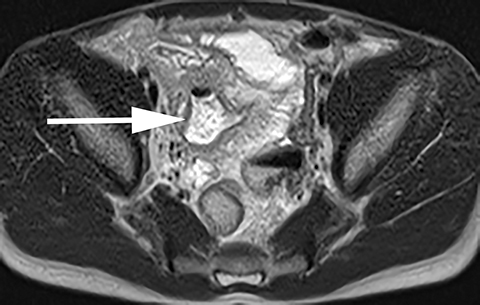
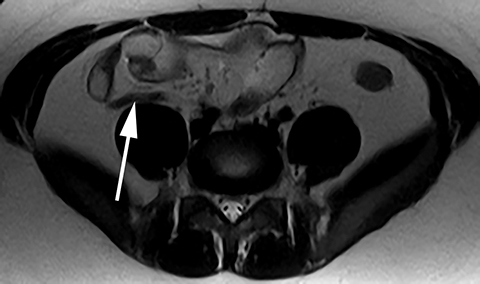
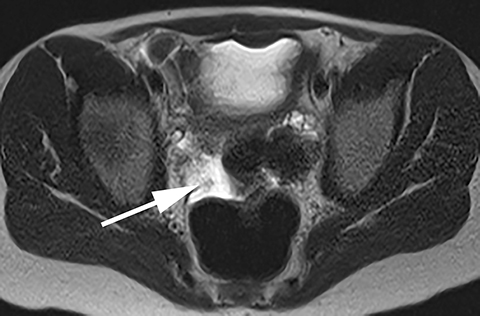
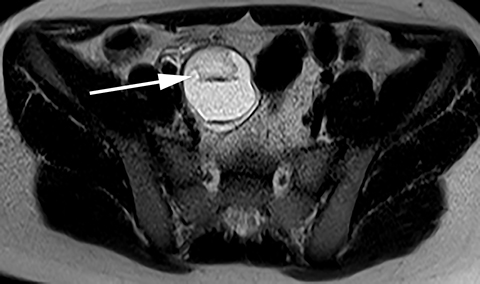
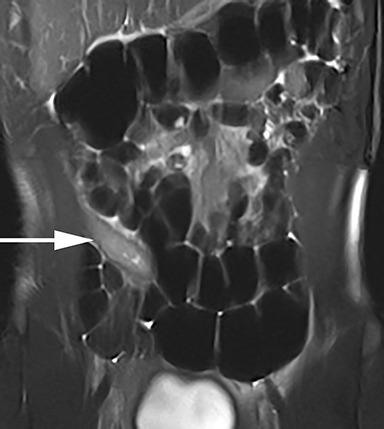
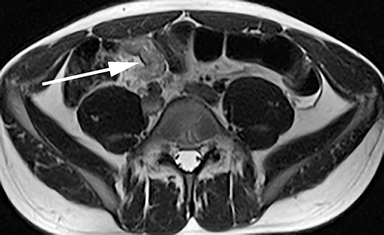
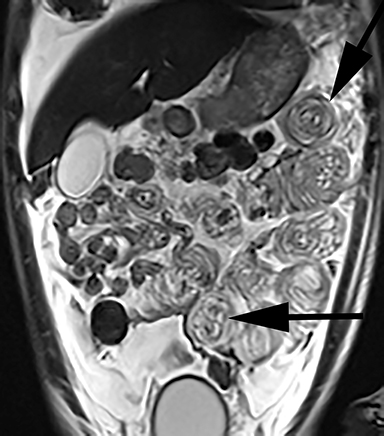
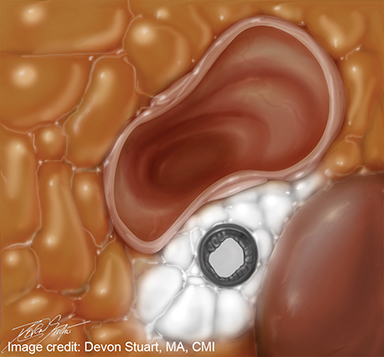
Focal periappendiceal inflammation is a hallmark of acute appendicitis and is readily detectable on the T2-weighted fluid sensitive sequences as high signal in the soft tissues adjacent to the appendix (Figure 1). In addition, fluid fills the lumen of the obstructed appendix, although it must be noted that a normal appendix may occasionally have a small amount of intraluminal fluid (in the absence of other findings). Appendicoliths are often visible (approximately 40% of cases)14 as intraluminal foci of signal dropout, and can be helpful in making the diagnosis, particularly when found obstructing the appendiceal lumen (Figures 2, 3). In tip appendicitis, the proximal appendix may appear normal; thus, it is important to assess the entire length of the appendix (Figure 4). Appendiceal enlargement is often present but is not an absolute criterion to diagnose appendicitis in the absence of surrounding inflammation.21 A ruptured appendix with abscess formation will be evident if an adjacent fluid collection is present (Figure 5). Further examples and expanded discussion are available in a previously published case interpretation pictorial essay.21
Normal appendix
The normal appendix on MRI, as on CT, is visible as a blind-ending tubular structure arising from the cecum. The normal appendix may be filled with air (low T2 signal in an nondependent position) or fluid (Figure 6). Detection of a normal appendix has increased with protocol optimization and experience. The normal appendix will be visualized in 70 to 80% of cases.17 We have also realized that inherent non-visualization of the appendix due to adjacent bowel or lack of intraperitoneal fat implies that the appendix is not inflamed or enlarged. Essentially, an inflamed appendix will almost certainly be visible on MRI. Furthermore, a small amount of pelvic peritoneal free fluid is a nonspecific finding in children with abdominal pain and is not diagnostic of appendicitis (Figure 7), although this finding does merit an additional higher level of scrutiny.21 Using this approach, our institutional negative predictive value is 98.9%.9 The negative predictive value of appendicitis MRI in children is 98.3% in the pediatric meta-analysis,17 a statistic that helps to facilitate efficient patient disposition from the emergency department.
Alternative diagnoses
MRI has the additional benefit of identifying alternative diagnoses as the cause of abdominal pain in up to 20% of patients, based on studies from three institutions. 15,20,22 While these alternative findings may be visible on CT, they would not necessarily be evident on a directed US examination of the appendix. The most common alternative diagnoses included adnexal cysts (Figure 8) and enteritis/colitis (Figure 9). Other relatively common and important alternative diagnoses include pyelonephritis, hydronephrosis, and ovarian torsion. Multiple examples of ovarian torsion are available for review within the literature.17,22 Occasionally, MRI will demonstrate unexpected or unusual etiologies for abdominal pain (Figure 10).
Current limitations
Evaluating appendicitis in children with MRI is not without limitations. Foremost is the need for ready access to an MRI scanner, a resource that is not uniformly available in all hospitals. The utilization of MRI for appendicitis assessment is particularly well suited for health systems that operate multiple magnets 24 hours per day. Second, while most patients can cooperate for the 15-minute exam time, a very young child (<5 years) or a severely neurologically impaired child may not be a good candidate. In these cases, we employ US as a first-line modality. Finally, a comparative cost effectiveness analysis that includes both direct and indirect costs is still needed to assess whether an imaging pathway utilizing MRI following equivocal ultrasound versus MRI as first-line imaging is the most effective approach.
Conclusion
The diagnostic and clinical outcomes associated with MR imaging of children with suspected appendicitis are excellent. A simplified, four-sequence protocol using T2 SS-TSE sequences is commonly utilized. Protocols longer than five sequences are not advised as they may hinder emergent magnet access. Gadolinium-enhanced T1 imaging has not been shown to provide added value beyond noncontrast technique. These studies should be performed without sedation, and may be attempted in children even younger than 5 years, depending on the child’s ability to cooperate. Multiple cases of appendicitis, the normal appendix, and alternative diagnoses are presented in this manuscript to assist the radiologist’s interpretation. The most salient interpretation feature of focal periappendiceal inflammation is emphasized in Figure 11.
References
- Callahan MF, Rodriguez CP, Taylor GA. CT of appendicitis in children. Radiology. 2002:224(2):325-332.
- Doria AS, Moineddin R, Kellenberger CJ, et al. US or CT for Diagnosis of Appendicitis in Children and Adults? A Meta-Analysis. Radiology. 2006;241(1):83-94.
- Strouse PJ. Pediatric Appendicitis: An Argument for US. Radiology. 2010;255(1):8-13.
- Trout AT, Sanches R, Ladino-Torres MF. A critical evaluation of US for the diagnosis of pediatric acute appendicitis in a real-life setting: how can we improve the diagnostic value of sonography? Pediatr Radiol. 2012;42(7):813-823.
- Hernanz-Schulman M. CT and US in the Diagnosis of Appendicitis: An Argument for CT. Radiology. 2010;255(1):3-7.
- Binkovitz LA, Unsdorfer KML, Thapa P, et al. Pediatric appendiceal ultrasound: accuracy, determinacy and clinical outcomes. Pediatr Radiol. 2015;45(13):1934-1944.
- Brenner DJ, Hall EJ. Computed tomography – an increasing source of radiation exposure. N Engl J Med. 2007;357(22):2277-2284.
- Miglioretti DL, Johnson E, Williams A, et al. The use of computed tomography in pediatric and the associated radiation exposure and estimated cancer risk. JAMA Pediatr. 2013;167(8):700-707.
- Kulaylat AN, Moore MM, Engbrecht BW, et al. An implemented MRI program to eliminate radiation from the evaluation of pediatric appendicitis. J Pediatr Surg. 2015;50(8):1359-1363.
- Cobben L, Groot I, Kingma L, et al. A simple MRI protocol in patients with clinically suspected appendicitis: results in 138 patients and effect on outcome of appendectomy. Eur Radiol. 2009;19(5):1175-1183.
- Sing AK, Desai H, Novelline RA. Emergency MRI of acute pelvic pain: MRI protocol with no contrast. Emerg Radiol. 2009;16(2):133-141.
- Johnson AK, Filippi CG, Andrews T, et al. Ultrafast 3-T MRI in the evaluation of children with acute lower abdominal pain for the detection of appendicitis. AJR Am J Roentgenol. 2012:198(6):1424-1430.
- Moore MM, Gustas CN, Choudhary AK, et al. MRI for clinically suspected appendicitis: Implemented program. Pediatr Radiol. 2012;42(9):1056-1063.
- Theime ME, Leeuwenburgh MM, Valdehueza ZD, et al. Diagnostic accuracy and patient acceptance of MR in children with suspected appendicitis. Eur Radiol. 2014;24(3):630-637.
- Dillman JR, Gadepalli S, Sroufe NS, et al. Equivocal pediatric appendicitis: enhanced MR imaging protocol for non-sedated children – a clinical effectiveness study. Radiology. 2015;279(1): 216-225.
- Petkovska I, Martin DR, Covington MF, et al. Accuracy of Unenhanced MR Imaging in the Detection of Acute Appendicitis: Single-Institution Clinical Performance Review. Radiology. 2016;279(2):451-460.
- Moore MM, Kulaylat AN, Hollenbeak SC, et al. Magnetic resonance imaging in pediatric appendicitis: a systematic review. Pediatr Radiol. 2016;46(6):928-939.
- Duke E, Kalb B, Arif-Tiwari H, et al. A Systematic Review and Meta-Analysis of Diagnostic Performance of MRI for Evaluation of Acute Appendicitis. AJR Am J Roentgenol. 2016;206(3):508-517.
- Aspelund G, Fingernet A, Gross E, et al. Ultrasonography/MRI versus CT for diagnosing appendicitis. Pediatrics. 2014;133(4):586-593.
- Koning JL, Naheedy JH, Kruk PG. Diagnostic performance of contrast-enhanced MR for acute appendicitis and alternative causes of abdominal pain in children. Pediatr Radiol. 2014;44(8):948-955.
- Moore MM, Brian JM, Methratta SM, et al. MRI for clinically suspected appendicitis: case interpretation. Pediatr Radiol. 2014;44(5):605-612.
- Moore MM, Kulaylat AN, Brian JM, et al. Alternative diagnosis at paediatric appendicitis MRI. Clinical Radiology. 2015;70(8):881-889.
Dr. Brian is an Assistant Professor of Radiology and Pediatrics, and Dr. Moore is an Associate Professor of Radiology and Pediatrics at Penn State College of Medicine, Hershey, PA.
