Posterior Nutcracker Syndrome with Left Renal Vein Duplication
By Urquiza SC, Viterbo GG, Galsim RJG


Case Summary
An adult presented with a hypertensive emergency and complaints of occasional left flank and lower abdominal pain. The physical examination was unremarkable. The patient was clinically diagnosed with hypertension, and work-up to determine the etiology was undertaken.
Imaging Findings
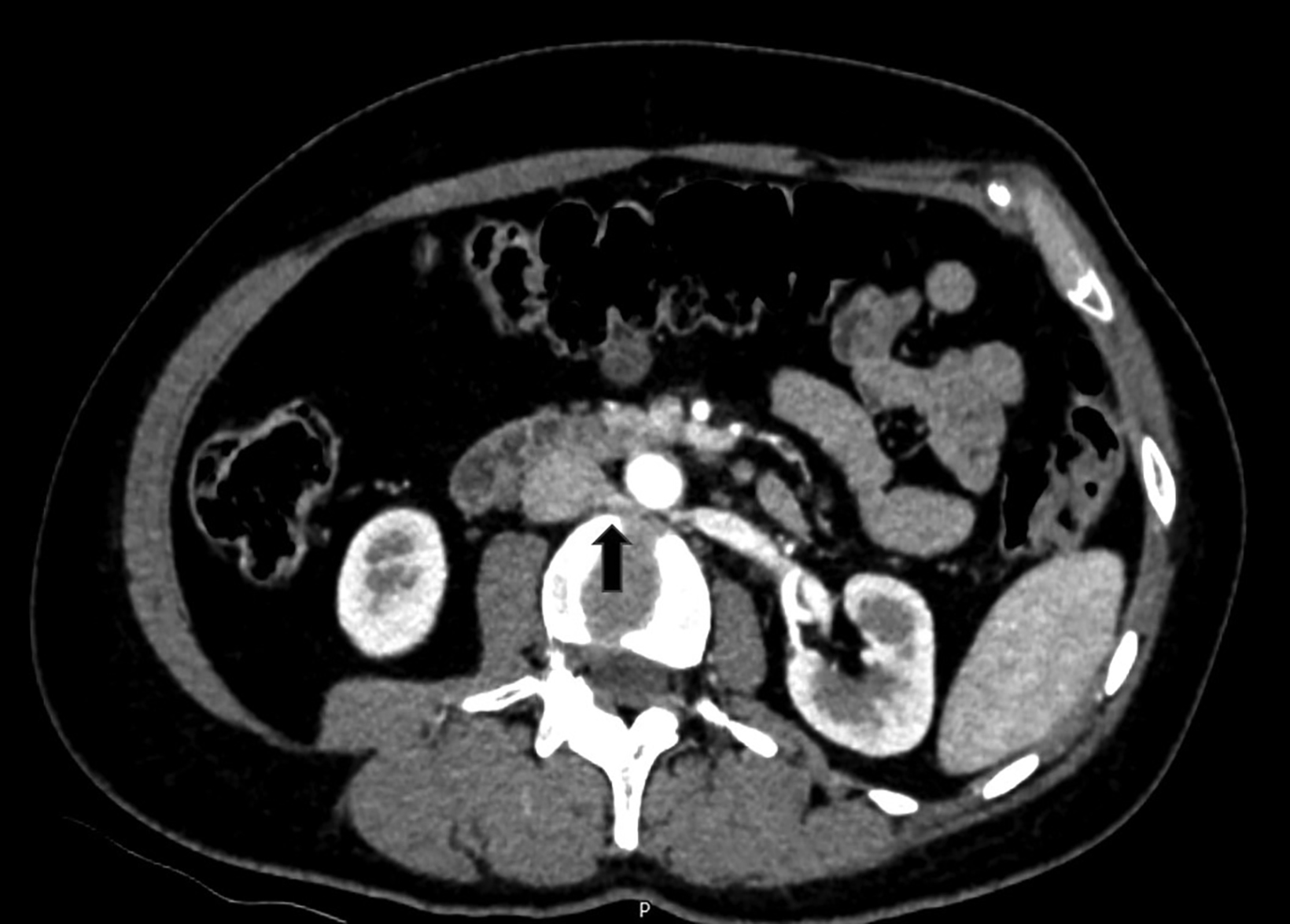
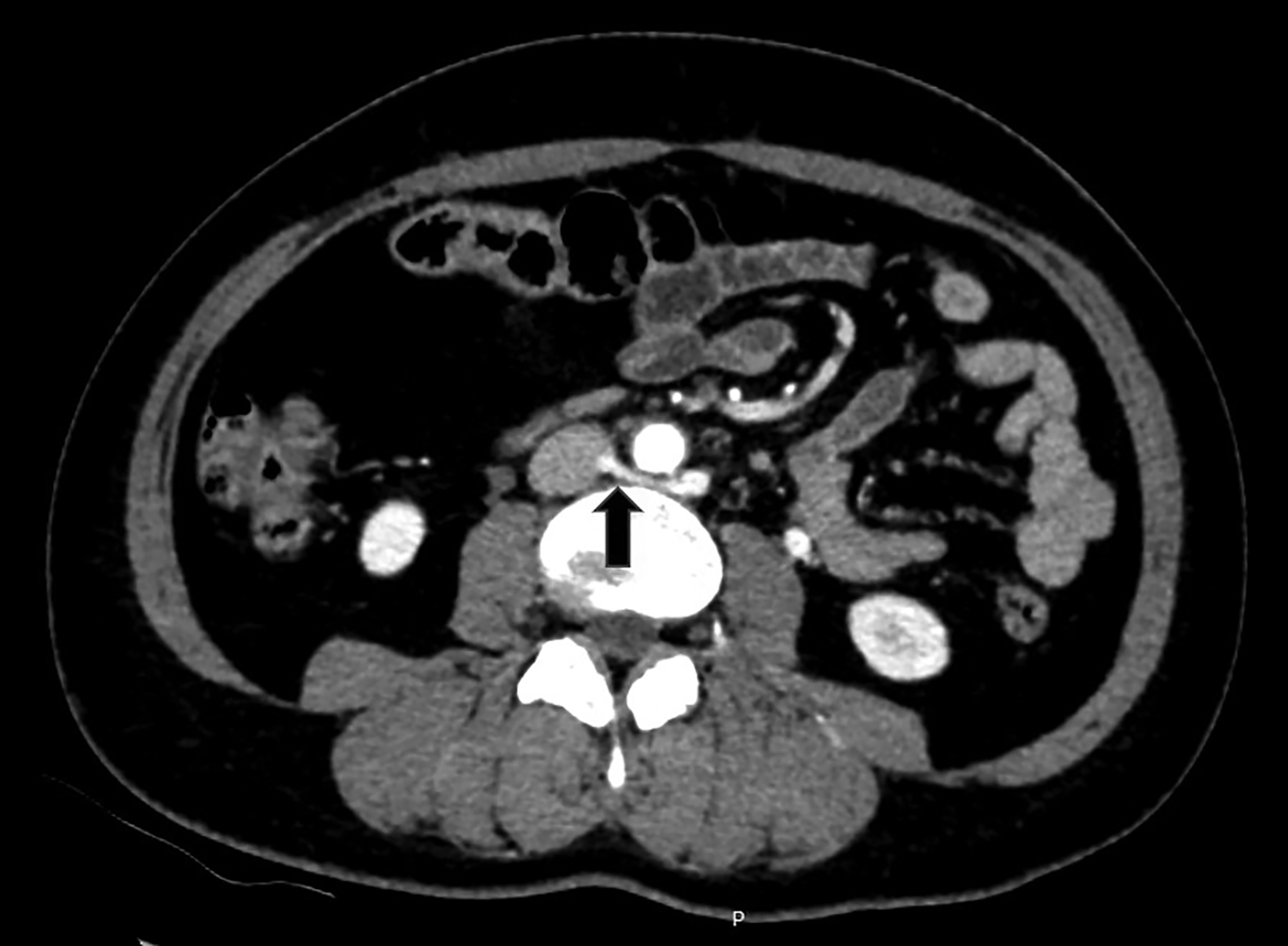
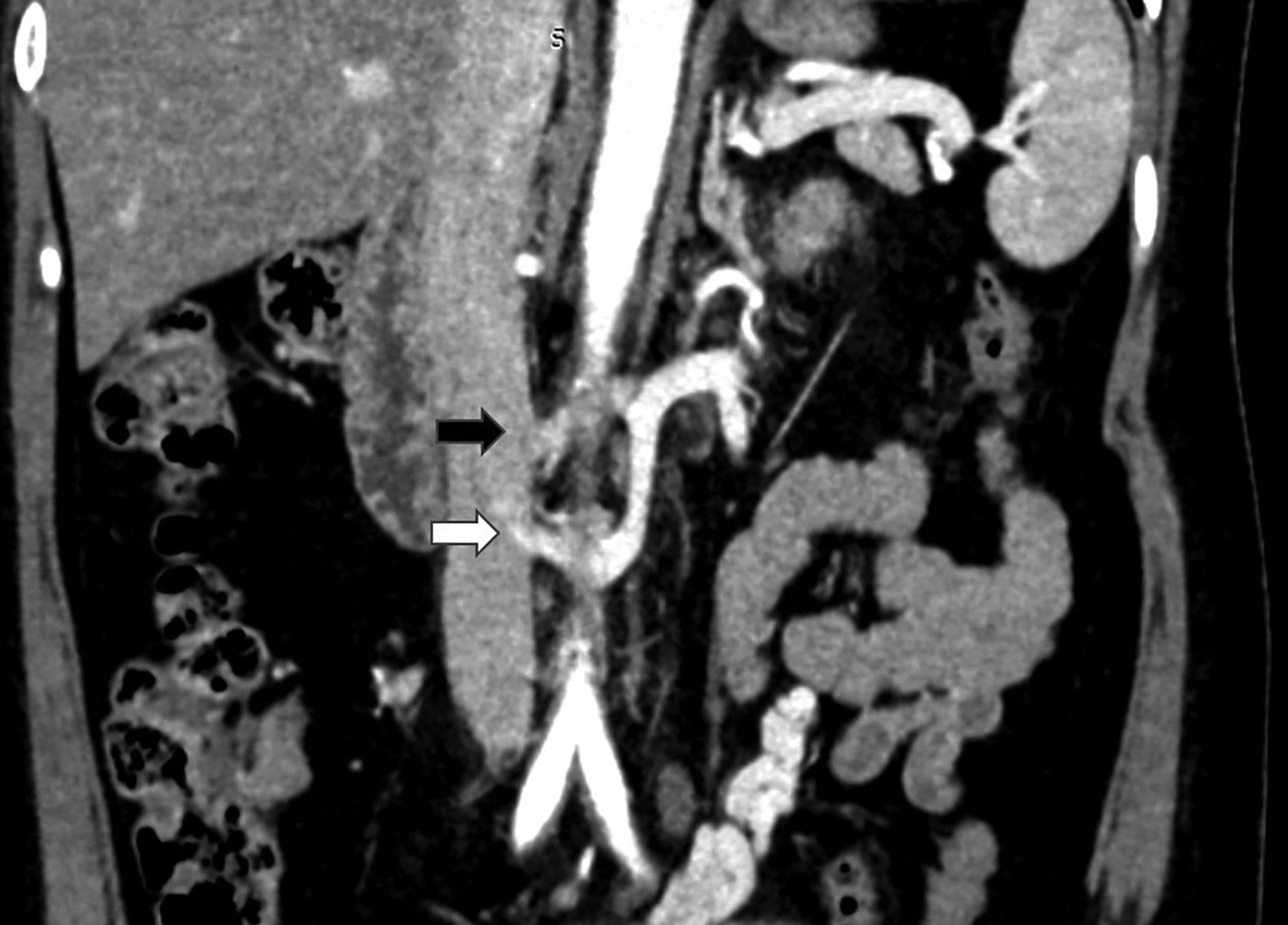
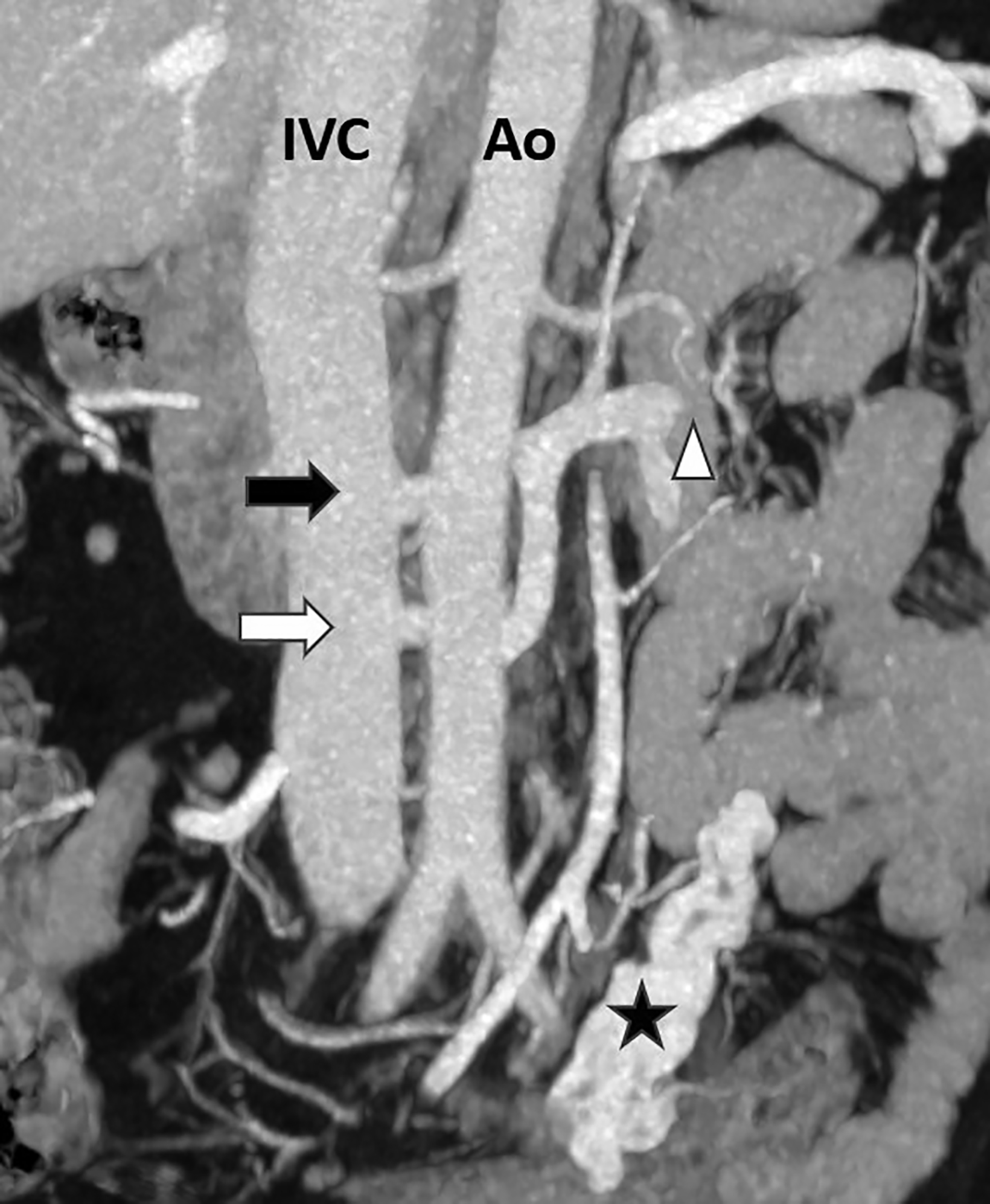
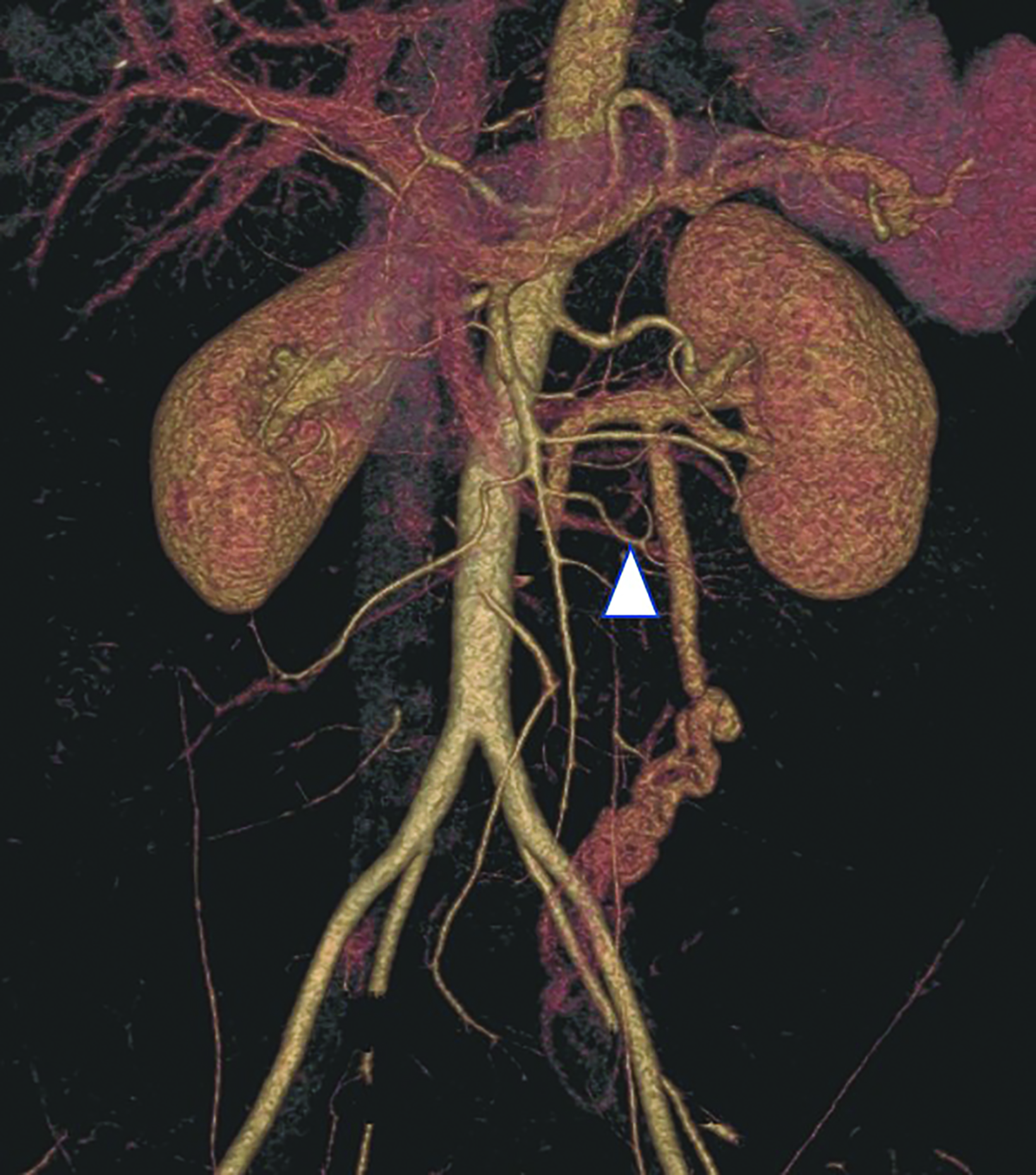
Computed tomography angiography (CTA) of the abdomen showed left renal vein duplication, with one renal vein draining at the level of the L2-L3 intervertebral disc space and the other at the level of the L3 vertebra (Figure 1). Both vessels were retroaortic and were partially compressed between the aorta and vertebrae (Figure 2). Minimal fat stranding was noted in the para-ortic and aortocaval regions. The main left renal vein was dilated. The gonadal veins, particularly the left, and tributaries were prominent and seen as tortuous vessels in the pelvic region (Figures 2,3). The inferior vena cava was dilated (2.6 cm).
Incidental findings of passive congestive changes of the liver and gallbladder lithiasis were noted. The renal arteries and remainder of the visualized arterial and venous system were unremarkable.
Diagnosis
Posterior nutcracker syndrome with left renal vein duplication
Discussion
Nutcracker syndrome, also known as entrapment of the left renal vein, is classified into two types, anterior and posterior. The latter, which is the type presented here, is the less frequent of the two, with few studies appearing in the literature.1 The posterior subtype exhibits male predominance, occurs primarily in adults, and is not known to be hereditary.1,2
In the normal embryological development of the inferior vena cava, portions of the subcardinal and supracardinal veins form an aortic collar, wherein its anterior portion gives rise to the left renal vein while the posterior portion regresses. In posterior nutcracker syndrome, the opposite happens. The left renal vein originates from the posterior portion, while the anterior aspect regresses, resulting in a retroaortic left renal vein that consequently is compressed between the abdominal aorta and vertebral column.3,4
Clinically, the most commonly observed symptom is hematuria. Owing to elevated venous pressure, thin-walled varices tend to rupture into the collecting system.5 The next most common symptom is gonadal pain syndrome or pelvic congestion syndrome. In females, persistently elevated venous pressure in the gonadal vein may eventually lead to reflux and collateral vessel formation, manifesting as lower abdominal or pelvic pain that radiates to the posteromedial thigh and buttock.3,5,6
Hypertension alone is not a typical clinical manifestation.7 Usually, hypertension is accompanied or preceded by abdominal pain, hematuria, and other signs, including orthostatic proteinuria, chronic fatigue, pelvic congestion and, in males, formation of a left- sided varicocele. Passage of blood clots along the left ureter may result in ureteral colic and manifest as left flank pain.5
Doppler ultrasonography, CTA, magnetic resonance angiography, and renal venography are established modalities for evaluation of these cases. Among these modalities, CTA is considered the gold standard owing to its noninvasive nature and superior evaluation of the retroperitoneal and vascular anatomy.
Imaging reveals retroaortic left renal vein and its abrupt narrowing point between the abdominal aorta and vertebral column, as well as secondary effects such as collateral vessel formation (eg, gonadal vein).1,3,4Associated radiologic abnormalities, including cross-fused renal ectopia and other vascular anomalies such as renal arteriovenous malformation, aneurysm, or left renal vein duplication may also be seen on CT, as in our case.1,3
Symptomatic treatment is based on clinical presentation and severity of left renal vein hypertension. Conservative treatment is suggested for mild cases, while left renal vein transposition, left renal autotransplantation, and endovascular stenting are proven effective in restoring an effective luminal diameter in symptomatic patients. Nephrectomy may be considered in severe cases.1,6,8
Conclusion
Posterior nutcracker syndrome with duplicated renal vein is a rare anomaly, presenting with varying signs and symptoms, the most common of which is hematuria. Hypertension is less frequent; therefore, multimodality diagnostic evaluation with imaging studies is important.
References
- Park JH, Lee GH, Lee SM, et al. Posterior nutcracker syndrome – a systematic review. Vasa. 2018. 47(1):23-29. https://doi.org/10.1024/0301-1526/a000670.
- Pournasiri Z. The nutcracker syndrome as a rare cause of chronic abdominal pain: a case report. J Compr Ped. 2016. 7(3):e39741 doi: 10.17795/compreped-39741.
- Orczyk K, Wysiadecki G, Majos A, et al. What each clinical anatomist has to know about left renal vein entrapment syndrome (Nutcracker syndrome): a review of the most important findings. Biomed Res Int. 2017: 1746570. https://doi.org/10.1155/2017/1746570.
- Karaman B, Koplay M, Özturk E, et al. Retroaortic left renal vein: multidetector computed tomography angiography findings and its clinical importance. Acta Radiol. 2007. 48(3): 355-360. https://www.ncbi.nlm.nih.gov/pubmed/17453511.
- Kurklinsky, AK and Rooke, TW. Nutcracker phenomenon and nutcracker syndrome. Mayo Clinic proceedings. 2010. 85(6), 552–559. https://doi.org/10.4065/ mcp.2009.0586.
- McPhee JT, Menard MT. Current management approach for left renal vein entrapment syndrome: the so-called Nutcracker syndrome. Interv. Cardiol. 2011;3(5): 557-565. https://www.openaccessjournals.com/articles/current-management-approach-for-left-renal-vein-entrapment-syndrome-the-socalled-nutcracker-syndrome.pdf.
- Narkhede NA, Deokar AB, Mehta KP, et al. Nutcracker syndrome with hypertension as an unusual initial presentation. Indian J Nephrol 2017;27:472-474. http:// www.indianjnephrol.org/text.asp?2017/27/6/472/208628.
- Gulleroglu K, Gulleroglu B, Baskin E. Nutcracker syndrome. World J Nephrol. 2014. 3(4): 277-281. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4220361/.
