Steatosis with Steatohepatitis
By O’Halloran P, Martin N, Teoh S, Marianacci E

Case Summary
A middle-aged patient with a history of alcohol dependence presented to the emergency department with weakness, icterus/jaundice, and weight loss progressively worsening over the previous five months. The patient was tachycardic and hypotensive with laboratory findings of anemia, transaminitis, and elevated INR. An enlarged liver was noted on physical exam.
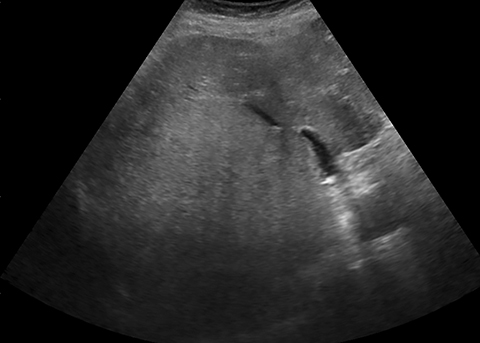
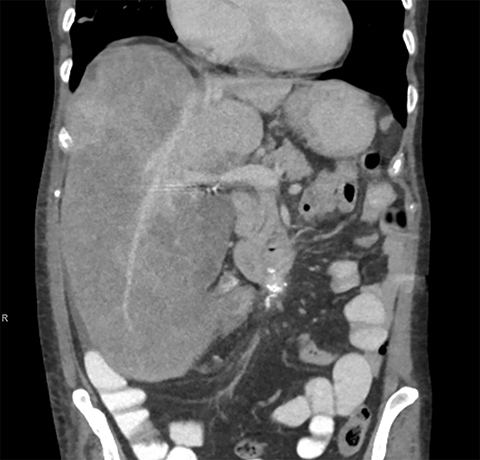
A right upper quadrant ultrasound demonstrated a heterogeneous, nodular liver and ascites. An abdominal/pelvic contrast-enhanced computed tomography (CECT) scan demonstrated a mass-like lesion of the right hepatic lobe, raising the possibility of malignancy.
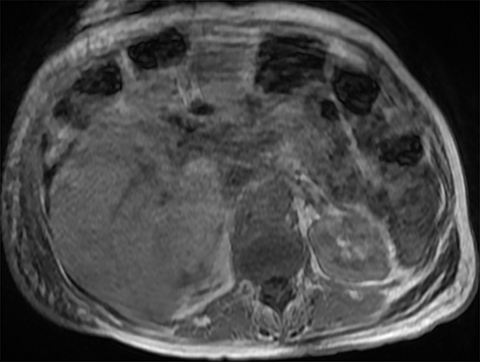
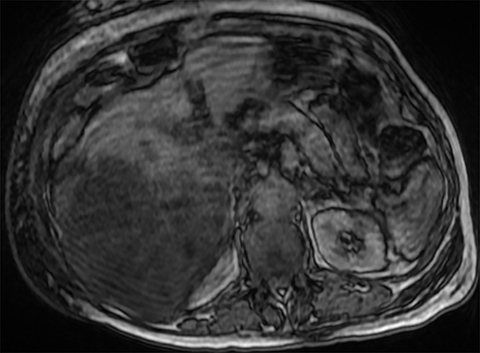
The alpha fetoprotein level was within normal limits. This lesion was therefore further characterized with an abdominal magnetic resonance imaging (MRI), at which point hepatic steatosis was the leading diagnosis, with the caveat that an underlying malignancy would be difficult to exclude in the absence of contrast in the setting of cirrhosis.
Given the patient’s history of significant weight loss, jaundice, and transaminitis, the care team felt tissue sampling was necessary to exclude malignancy, despite reassuring imaging findings.
Imaging Findings
On ultrasound, the liver was enlarged and heterogeneously echogenic with decreased through transmission, consistent with fatty infiltration (Figure 1).1 The appearance of a nodular liver contour and ascites were consistent with cirrhosis in a patient with a history of alcohol dependence.
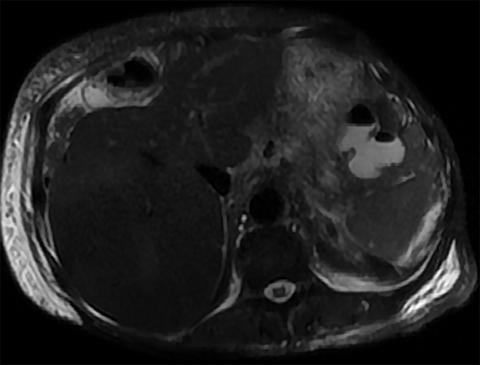
On CECT, the liver was nodular and heterogeneous, with atrophy of the left hepatic lobe, confirming cirrhosis (Figure 2). There was mass-like enlargement of the right hepatic lobe with diffusely decreased attenuation. Despite mass effect on the middle hepatic vein, portal veins were seen coursing through the right hepatic lobe lesion without focal abnormal enhancement, most consistent with hepatic steatosis.
Differential consideration was given to neoplastic masses such as hepatocellular carcinoma or cholangiocarcinoma; however, these typically demonstrate invasion, obstruction, and/or displacement of the hepatic vasculature and biliary tree.2 Other infiltrative malignancies such as lymphoma would be hyperdense on CECT.
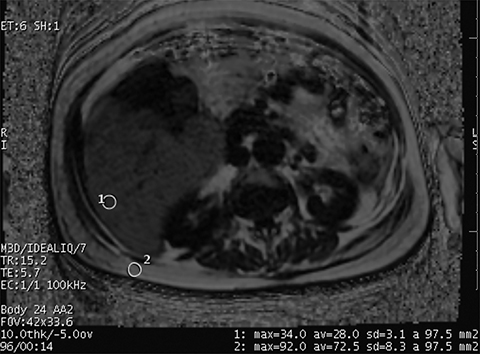
On MRI, (Figure 3), the uniform right hepatic lobe signal dropout on out-of-phase imaging was consistent with hepatic steatosis. This was supported by dropout of signal on fat saturation sequences. Finally, Iterative Decomposition of water and fat with Echo Asymmetry and Least squares estimation (IDEAL) imaging is an accepted method of quantifying fat within the liver which confirmed grade II hepatic steatosis in the right hepatic lobe.3,4
Diagnosis
Steatosis with steatohepatitis
Discussion
Hepatic steatosis affects approximately 15% of the population and is even more common in patients with alcohol dependence, hyperlipidemia, or obesity. Coincidence of both alcohol dependence and obesity correlate with an increased incidence of 95%. Hepatic steatosis can also be associated with viral hepatitis, medication reaction, nutritional abnormality, or inherited disorders.2
On a cellular level, hepatic steatosis is characterized by the accumulation of triglycerides within hepatocytes, which can cause cellular damage and inflammation (steatohepatitis). This eventually culminates in cirrhosis.
However, histologic analysis is not always needed to diagnose hepatic steatosis. Classic ultrasound findings include liver echogenicity greater than renal cortex or spleen, as well as posterior attenuation of the ultrasound beam; these findings are 60-100% sensitive and 77-95% specific. Classic noncontrast CT findings of hepatic steatosis include attenuation of at least 10 HU less than the spleen, or absolute measurement of less than 40 HU. These findings are 43-95% sensitive and 90% specific. CECT is not reliable for diagnosis of hepatic steatosis. Classic MRI findings include signal drop-out on out-of-phase sequences; this finding is 81% sensitive and 100% specific.2
Unfortunately, other lesions, including hepatic adenoma, hepatocellular carcinoma, and focal nodular hyperplasia, can also contain microscopic fat. Hepatocellular carcinoma (HCC) specifically can have an infiltrative appearance, making it difficult to exclude.
Risk factors including unintentional weight loss and cirrhosis contribute to clinical concern for HCC. In this setting, the Liver Imaging Reporting and Data System (Li-RADS) can be used to guide management. This lesion demonstrated size greater than 2 cm without any major criteria such as arterial phase hyperenhancement, washout, a capsule, or growth; therefore, it was appropriately classified as LR-3.5
Li-RADS-3 lesions are associated with an intermediate probability of HCC (approximately 38%).
Management generally includes repeat or alternative diagnostic imaging in 3-6 months; however biopsy can be used judiciously.5
Conclusion
Hepatic steatosis can present as mass-like on multiple imaging modalities. In this case, the mass-like enlargement of the right hepatic lobe, displacement of the middle hepatic vein, cirrhosis, and weight loss were suspicious for malignancy.
Despite imaging findings that are classic for hepatic steatosis on multiple modalities, an ultrasound-guided biopsy was performed to confirm the diagnosis of hepatic steatosis superimposed on background cirrhosis.
References
- Bhatnagar G, Sidhu HS, Vardhanabhuti V, et al. The varied sonographic appearances of focal fatty liver disease: review and diagnostic algorithm. Clin Radiol. 2012; 67:372–379.
- Hamer OW, Aguirre DA, Casola G, et al. Fatty liver: imaging patterns and pitfalls. RadioGraphics. 2006; 26(6):1637-1653.
- Liu CY, McKenzie CA, Yu H, Brittain JH, Reeder SB. Fat quantification with IDEAL gradient echo imaging: correction of bias from T(1) and noise. Magn Res Med. 2007;58(2):354-364.
- Cassidy FH, Yokoo T, Aganovic L, et al. Fatty liver disease: MR imaging techniques for the detection and quantification of liver steatosis. Radiographics. 2009; 29(1):231-260.
- Victoria Chernyak , Kathryn J. Fowler, Aya Kamaya, et al. Liver Imaging Reporting and Data System (LI-RADS) version 2018: imaging of hepatocellular carcinoma in at-risk patients. Radiology. 2018; 289(3):816-830.
Affiliations: Mount Auburn Hospital, Harvard Medical School, Israel Lahey Health, Cambridge, MA.
