Stereotactic breast biopsies: An update in the era of digital tomosynthesis
Images


Stereotactic vacuum-assisted biopsy (S-VAB) has long been considered the preferred method to sample microcalcifications and sonographically occult masses in the breast, as well as a better alternative to traditional surgical excision.1 With increased utilization of digital breast tomosynthesis (DBT), DBT-guided vacuum-assisted biopsy (DBT-VAB) is now essential to biopsy mammographic abnormalities not well visualized on conventional full-field digital mammography (FFDM).
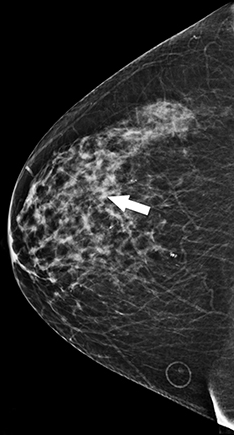
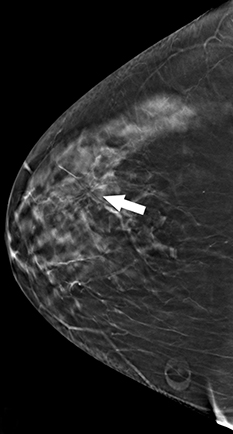
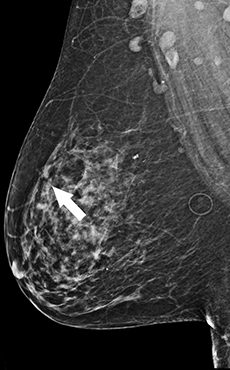
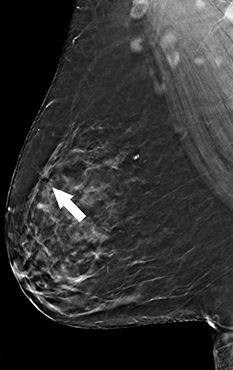
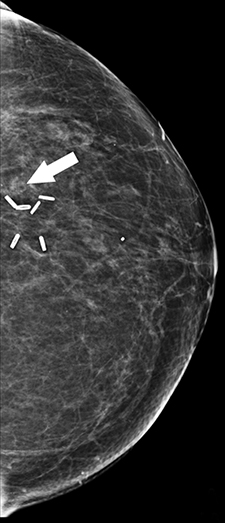
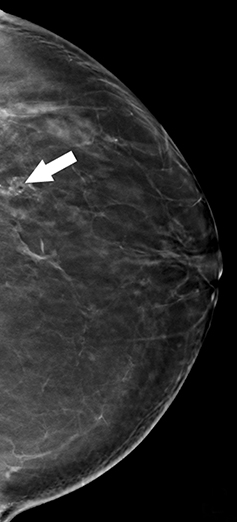
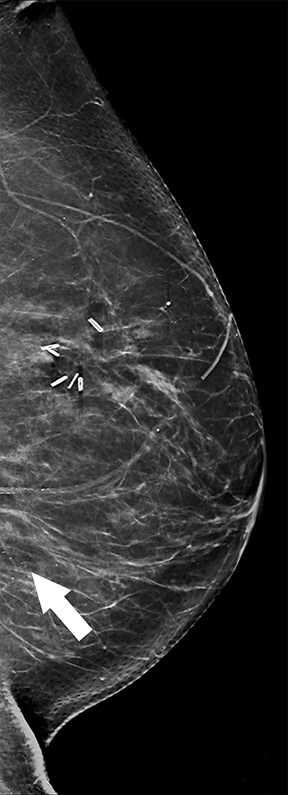
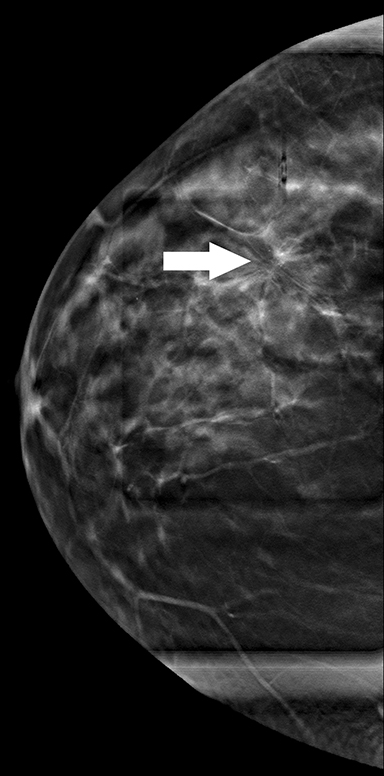
Recent studies have demonstrated that screening mammography utilizing DBT with FFDM has resulted in decreased recall rates and increased invasive cancer detection compared to conventional digital screening mammography.2,3 As patients become more aware of these studies, more of them are requesting DBT with their screening mammograms. DBT has been shown to identify certain mammographic abnormalities that may not be well evaluated or seen on FFDM, such as architectural distortions (Figures 1,2), subtle calcifications (Figures 3,4) or suspicious asymmetries and masses in patients with dense breasts.4,5 Additionally, DBT can help better characterize lesions, discriminate between benign and malignant morphologic features, and differentiate between overlying breast tissue and true mammographic abnormalities.4
Techniques
Stereotactic vacuum-assisted biopsies are often performed with the patient prone, although add-on upright units are available for stereotactic biopsy. Prone S-VABs are performed with the patient lying on the biopsy table with the breast inserted into an opening in the table and compressed between the image receptor and compression plate. The compression plate contains the biopsy window, typically 5 x 5 cm in size. Initial scout images are performed with the X-ray tube perpendicular to the image receptor (0o position). After confirmation of the target within the biopsy window, a pair of images is obtained at +15o and -15o positions (stereo pair) to determine the location of the target in a Cartesian coordinate system (X,Y,Z). Alternatively, a polar coordinate system can be used for targeting, with the needle angled slightly upwards as opposed to perpendicular in the Cartesian coordinate system. This may allow for easier access to more posterior lesions.6 A vacuum-assisted biopsy device is then advanced to the calculated coordinates. A stereo pair of images may be taken prior to deploying the needle (Pre-Fire) and/or following the needle deployment (Post-Fire) to confirm appropriate needle location. Vacuum-assisted core samples are then obtained.
Meanwhile, DBT-VABs are typically performed utilizing an add-on unit to a tomosynthesis-capable mammography machine with the patient in an upright position, although newer technologies are now available for prone DBT-biopsy. For upright DBT-VAB, the patient is usually positioned in a sitting or lateral decubitus position with the breast compressed between the image receptor and compression plate. The compression paddle is often transparent and comprises a larger biopsy window compared to those typically used with prone or upright S-VAB. The initial localizing scout image is obtained using DBT, which can then also be used to calculate the target location coordinates. Once the biopsy device is advanced to the target, DBT images may be obtained prior to and following needle deployment to confirm needle location. Vacuum-assisted core samples are then obtained.
Disadvantages of S-VAB, prone VAB
The pitfalls of S-VAB have been widely publicized. Certain mammographic abnormalities that have limited visualization on conventional FFDM, including noncalcified masses, faint microcalcifications and some architectural distortions, can make S-VAB difficult.1 Additionally, initial planning and triangulation of the mammographic abnormality, particularly in regards to accurate depth measurements, of a 3D finding on the traditional 2D FFDM may be time consuming and allows room for error.1
Vacuum-assisted biopsy with patients in the prone position has a known limitation of being unable to target lesions that are far posterior in depth or close to the axilla due to limited positioning.7 This limitation is typically circumvented by placing both the ipsilateral arm and the breast of interest through the table opening (arm through the hole technique) in order to access more posterior tissue.8 Patient factors such as mobility and weight also may limit use of the prone stereotactic table. In addition, the prone table system is an expensive, and perhaps less cost-effective, unit that only has the ability to perform stereotactic biopsies and cannot be used for routine mammographic imaging.
Advantages, disadvantages of upright VAB
>One of the largest advantages of the upright over the prone table is that there is no weight limit. Some of the chairs used during the upright biopsy are reclinable, which has the added benefit to allow for easier access of more posterior and lateral tissue while putting the patient in a supine oblique position. Additionally, the upright VAB unit is an add-on device to an existing upright mammographic machine; thus, it is an overall cheaper system to implement. It is also easier to translate the position of targeted lesions from the mammogram to the pre-biopsy images on the upright systems. Most upright VAB systems are now add-on to a mammographic machine with tomosynthesis capability, allowing the mammographic abnormality to be localized on a full field detector (18 x 24 cm) with DBT versus the typical 5 x 5 cm biopsy window used for S-VAB.1
A known disadvantage to the upright VAB is an increased possibility of patient experiencing a vasovagal reaction when compared to the prone position and increased patient anxiety due to the ability to see the needle, skin entry site, and tissue sampling during the procedure.1
Advantages, disadvantages of DBT-VAB
In addition to the advantages of upright VAB, DBT-VAB has been shown to halve the overall procedure time compared to prone or upright S-VAB.1 Additionally, there is no requirement for triangulation of the mammographic abnormality via stereo pair images as the depth is calculated by the system automatically when localizing an abnormality on scout tomosynthesis images (Figures 5-6). Pre-fire images using tomosynthesis can allow the radiologist to better make fine adjustments prior to biopsy since the location of the needle tip can be accurately determined. The literature has demonstrated a high success rate with abnormalities biopsied by DBT with a low percentage of radiologic-pathologic discordance.1 Although DBT images result in a slightly greater radiation dose per exposure compared to FFDM, DBT-biopsy requires overall a lower number of exposures compared to P-VAB, resulting in overall decreased radiation exposure to the breast.9,10
While there are not many disadvantages of DBT-biopsy in the literature, one factor considered a disadvantage by some is that the glandular tissue of the entire breast is exposed during targeting with DBT due to the transparent compression paddle versus exposure to just a small amount of glandular tissue in the often-utilized 5 x 5 cm window used with PS-VAB.1
Conclusion
As early studies are demonstrating the advantages of DBT over FFDM, including increased invasive cancer detection rates particularly with abnormalities identified only on DBT, DBT-VAB is being used more frequently. DBT-VAB has shown many advantages and few disadvantages when compared to S-VAB and may eventually replace S-VAB in terms of sampling mammographic abnormalities identified on both DBT and FFDM. Additionally, with the advent of prone DBT-VAB, some of the disadvantages of upright tables may be avoided with the use of prone tables while maintaining the advantages of DBT biopsy.
References
- Schrading S, Distelmaier M, Dirrichs T, et al. Digital breast tomosynthesis-guided vacuum-assisted breast biopsy: initial experiences and comparison with prone stereotactic vacuum-assisted biopsy. Radiology. 2015;274(3):654–662.
- Sharpe RE, Venkataraman S, Phillips J, et al. Increased cancer detection rate and variations in the recall rate resulting from implementation of 3D digital breast tomosynthesis into a population-based screening program. Radiology. 2016; 278(3):698–706.
- Carbonaro LA, Di Leo G, Clauser P, et al. Impact on the recall rate of digital breast tomosynthesis as an adjunct to digital mammography in the screening setting. A double reading experience and review of the literature. Eur J Radiol. 2016; 85(4):808-814.
- Kopans, DB. Digital breast tomosynthesis from concept to clinical care. AJR Am J Roentgenol. 2014; 202(2):299–308.
- Durand MA, Wang S, Hooley RJ, et al. Tomosynthesis-detected architectural distortion management algorithm with radiologic-pathologic correlation. RadioGraphics. 2016; 36(2):311–321.
- Kopans, DB. Breast Imaging. 3rd ed. Philadelphia: Lippincott, Williams & Wilkins; 2006.
- Jung YJ, Bae JY, Seo H, et al. Lateral decubitus positioning stereotactic vacuum assisted breast biopsy with true lateral mammography. J Breast Cancer. 2011; 14(1):64-68.
- Soo MS, Walsh R, Patton J. Prone table stereotactic breast biopsy: facilitating biopsy of posterior lesions using the arm-through-the-hole technique. AJR Am J Roentgenol. 1998; 171(3):615-617.
- Paulis LE, Lobbes MB, Lalji UC, et al. Radiation exposure of digital breast tomosynthesis using an antiscatter grid compared with full-field digital mammography. Invest. Radiol. 2015;50(10):679-685.
- Sumkin, JH (2016, April). Tomosynthesis (DBT) directed biopsy. Presented at the meeting of the Society of Breast Imaging, Austin, TX.
Citation
AR J, KQ S, PT H. Stereotactic breast biopsies: An update in the era of digital tomosynthesis. Appl Radiol. 2018;(9):17-20.
September 22, 2018