Superficial siderosis
By Cheah WH
CASE REPORT
A 75-year-old woman with underlying hypertension and dyslipidemia was referred to our neuromedical clinic for a one-year history of unsteady gait and bilateral hearing loss (left greater than right). She claimed no history of acute weakness or fall. She described the unsteadiness as stable; however, she said she felt more left-side clumsiness than right. On examination she was alert, conscious, and full GCS. She had a positive cerebellar sign in which she demonstrated broad-based gait, difficulty in turning, and a positive Romberg’s test. An eye examination showed unsustained nystagmus at lateral gaze. The power of all four limbs was preserved and reflexes were normal, despite her dependence on a cane for walking. Left-ear hearing loss was noted.
The initial working diagnosis was neurodegenerative disease to rule out cause, silent stroke, or paraneoplastic manifestation. Subsequently, the patient was scheduled for CT brain, MRI brain /MRA, MRI cervical spine, and a blood test. Blood count and renal and liver function tests were normal. No drug treatment was commenced; however, the patient was referred for physiotherapy.
IMAGING FINDINGS
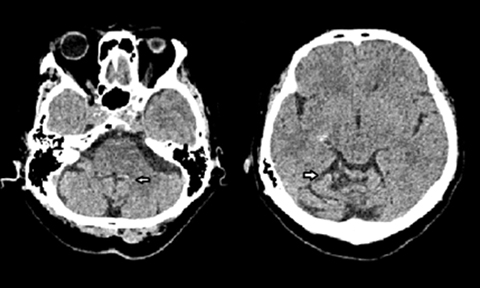
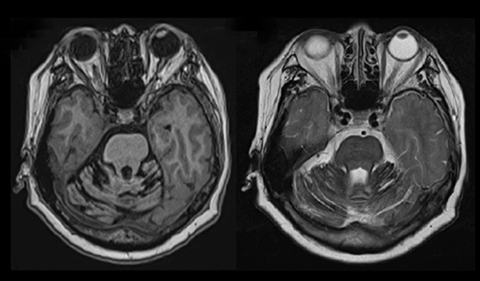
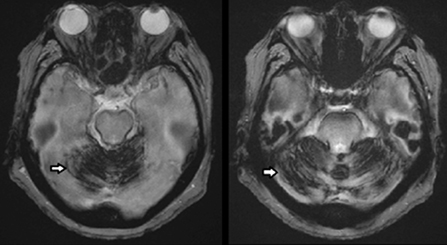
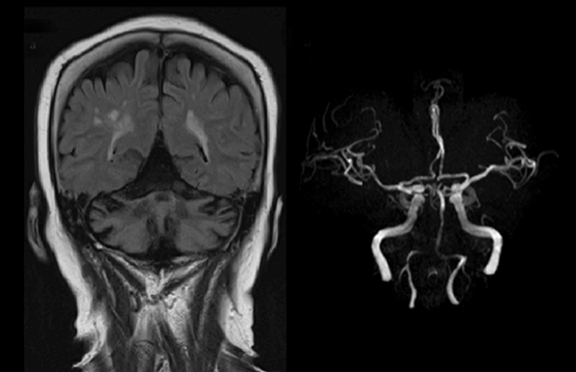
Initial nonenhanced CT brain images showed subtle hyperdensities along the subarachnoid region of the cerebellum (Figure 1). An MRI of the brain showed cerebellar atrophy with T1W/T2W (Figure 2) hypointense rim around the cerebellum, midbrain, pons, and medulla oblongata. This region demonstrates blooming artifact on gradient echo (GRE, Figure 2, 3) as hemosiderin deposits are more conspicuous. No focal brain parenchymal lesion or acute infarct was seen. MRI angiogram of cerebral vessels showed no significant stenosis (Figure 4). On MRI cervical spine, there was degenerative disc disease of the cervical spine with no significant spinal canal stenosis or nerve root impingement.
No cause was identified for the hemosiderin depositions in posterior fossa structures. As the patient’s symptoms were not progressive and her goal was to improve balance, she was referred for physiotherapy and continued care in the outpatient clinic.
DIAGNOSIS
Superficial siderosis
DISCUSSION
Superficial siderosis (SS), also known as marginal siderosis or central nervous system siderosis, is an uncommon and insidious cause of progressive neurological deterioration characterized by widespread free iron and hemosiderin deposition along the leptomeninges.1 Chronic recurrent subarachnoidal hemorrhage with bleeding into the cerebrospinal fluid is the cause of deposition of hemosiderin. The condition is characterized by the clinical triad of sensorineural hearing loss, cerebellar ataxia, and pyramidal signs.2 Due to its low prevalence, SS often goes undetected at initial evaluation and patients are commonly misdiagnosed with another neurodegenerative process. Indeed, in the past SS was diagnosed mainly at autopsy; however, with the advent of MRI, the condition has been found to be more common than previously assumed.3 It must be considered in all patients with cerebellar syndrome of unknown cause.
Common etiologies include trauma (including cervical nerve root avulsions/brachial plexus injuries), neoplasm (eg, oligodendroglioma, ependymoma, and astrocytoma), and vascular lesions (including arteriovenous malformations, cavernomas, aneurysms, and fragile capillary regrowth after brain surgery.2 However, in approximately one-fourth of cases no cause is found, even at autopsy.4 Research has found that a single episode of subarachnoid haemorrhage is usually not sufficient to result in this condition. SS has a predilection for the cerebellum and the eighth cranial nerve. This may be explained to some extent by blood pooling in the posterior fossa. In addition, the vestibulocochlear nerve has a long glial segment that predisposes the nerve to iron deposition and, hence, axonal injury.5 Finally, the presence of Bergmann glial cells in the cerebellum that display increased ferritin synthesis makes it preferentially affected.6
Most patients present with the clinical triad of sensorineural hearing loss (95% of cases), cerebellar ataxia (88%) and pyramidal signs (76%).7 Other less common manifestations include dementia, urinary bladder incontinence, sensory deficits and other cranial nerve dysfunction. When symptomatic, SS results in progressive and irreversible CNS damage. Notably, the degree of imaging abnormality does not always correlate with degree of clinical impairment.
Early detection in some cases with an identified cause of bleeding allows treatment that may prevent progression of the disease. The imaging study of choice is MRI, which is highly sensitive and specific for SS. A linear rim of T1W/T2W hypointensity coating the surface of the brain and sometime extending along the cranial nerves is pathognomonic. This finding has been speculated to be secondary to the presence of hemosiderin. Therefore, gradient-echo imaging or susceptibility-weighted imaging are the best and most sensitive sequences to evaluate SS due to its magnetic susceptibility effects, also known as blooming artifact.
Symptomatic patients normally undergo an initial CT brain scan; findings will show a rim of mild hyperdensity around the brain stem, as well as cerebellar atrophy. When SS is diagnosed using imaging, efforts must be directed to identify the source of recurrent subarachnoid hemorrhage. Contrast-enhanced MR studies and MRA through the circle of Willis should be obtained. In the absence of an intracranial abnormality, further evaluation should include MR imaging of the spine to look for spinal cord lesions. If no source is identified, further evaluation with conventional catheter angiography may be warranted to exclude a vascular lesion.
Primary differential diagnoses include meningoangiomatosis and neurocutaneous melanosis. Meningoangiomatosis is a rare, benign disease characterized by leptomeningeal calcifications and hamartomatous proliferation of meningeal cells along the leptomeninges and cortex. In neurocutaneous melanosis, on the other hand, multiple cutaneous nevi will be seen. Imaging reveals melanin deposits within the parenchyma and leptomeninges; these deposits appear similar to those in SS.
Assessing clinical outcomes is difficult in light of the disease’s slow progression. There is currently no effective treatment; previous attempts to treat with iron chelation have been unsuccessful.8
CONCLUSION
Superficial siderosis of the central nervous system is a rare and insidious condition that must be considered in all patients with cerebellar syndrome of unknown cause in order to avoid delays in diagnosis and treatment. Determining the underlying cause is crucial, as eliminating the source of bleeding may halt further disease progression.
REFERENCES
- Weekamp H, Huygen P, Merx J, Kremer H, Cremers CW. Longitudinal analysis of hearing loss in a case of hemosiderosis of the central nervous system. Otology & neurotology. 2003;24(5):738-742.
- Bracchi M, Savoiardo M, Triulzi F, Daniele D, Grisoli M, Bradac GB, et al. Superficial siderosis of the CNS: MR diagnosis and clinical findings. Am J Neuroradiol. 1993;14(1):227-236.
- Messori A, Di Bella P, Herber N, Logullo F, Ruggiero M, Salvolini U. The importance of suspecting superficial siderosis of the central nervous system in clinical practice. J Neurol, Neurosurg & Psych. 2004;75(2):188-190.
- Trevor Hughes J, Oppenheimer D. Superficial siderosis of the central nervous system. Acta Neuropathologica. 1969;13(1):56-74.
- Gauci J, Grech R, Aquilina J. Superficial siderosis following posterior fossa exploration. Brain Disord Ther. 2015;4(184):2.
- Kumar N. Neuroimaging in superficial siderosis: an in-depth look. Am J Neuroradiol. 2010;31(1):5-14.
- Fearnley JM, Stevens JM, Rudge P. Superficial siderosis of the central nervous system. Brain. 1995;118(4):1051-1066.
- Koeppen AH, Michael SC, Li D, Chen Z, Cusack MJ, Gibson WM, et al. The pathology of superficial siderosis of the central nervous system. Acta neuropathologica. 2008;116(4):371.
Prepared by Dr. Hun while a Radiologist at Universiti Sultan Zainal, Abidin, Malaysia.
