Virtual colonoscopy: A storm is brewing



Dr. Vining is a Professor of Diagnostic Radiology and the Medical Director of the Image Processing and Visualization Laboratory, University of Texas M.D. Anderson Cancer Center, Houston, TX.
Dr. Vining discloses that he has received royalties from Wake Forest University and Bracco, Inc., for virtual colonoscopy-related products.
A storm is brewing around virtual colonoscopy (VC) and whether radiologists or gastroenterologists will ultimately control this technology. Imagine the following: in the near future, a patient who requires colorectal cancer (CRC) screening walks into a local gastroenterologist's office,obtains a VC examination, which is read by a nurse practitioner, and, following consultation with a gastroenterologist, undergoes immediate optical colonoscopy (OC) for evaluation of tiny polyps that either cannot be found or turn out to be residual feces. Meanwhile, a radiologist working with this practice interprets the CT data for extracolonic findings in exchange for a small percentage of the total professional fee. The patient’s insurance (ie, Medicare) is billed for both the VC and OC, which taxpayers ultimately pay. If this sounds far-fetched, read on....
Virtual colonoscopy development
Colorectal cancer is the second leading cause of cancer death in the United States, but it is also one of the most preventable when screening is used to detect and treat early disease. The 5-year survival rate for early stage I CRC is 93%, but when it metastasizes to distant organs and becomes stage IV disease, the survival rate decreases to 8%. 1 Unfortunately, many adults over the age of 50 do not undergo screening,and, as a result, CRC is more often diagnosed in advanced stages. 2 Virtual colonoscopy offers the public a more appealing and less invasive alternative for screening.
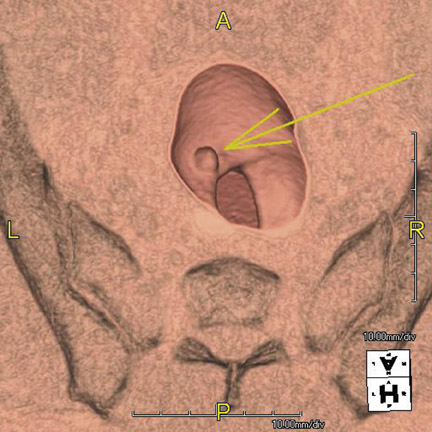
I performed the first VC, also known as CT colonography (CTC), at the Wake Forest University Health Sciences Center in 1993. It has taken nearly 15 years for VC to mature and gain acceptance by policy makers. The basic technique consists of: 1) bowel cleansing and stooltagging, 2) gas insufflation of the colon, 3) CT scanning of the abdomen/pelvis, and 4) 2- and 3-dimensional image analysis of the data toidentify polyps and masses (Figure 1). The first VC examination took 60 seconds to scan a patient using a single-slice helical CT scanner and nearly 8 hours to process the data for a fly-through, but today multidetector CT scanners acquire the data in a few seconds, and processing occurs in real time using inexpensive computers.
Despite the technological advances that have occurred during the past decade (eg, CO 2 insufflation, multidetector CT scanners, stool tagging, computer-assisted diagnosis), a strong lobbying effort on the part of gastroenterologists has delayed the availability of VC in the United States. Since Congress approved reimbursement for CRC screening in the 1997 Balanced Budget Act, the number of colonoscopies conducted annually in the United States has increased from 4 million in 2000 to >14 million in 2002. 3
Handwriting on the wall
Clinical trials that compared VC with OC have shown a dramatic improvement in VC accuracy in the last few years, culminating in 2 major trials that were announced in September 2007. The ACRIN National Colonography Trial enrolled over 2500 patients at 15 sites, and it reported that VC had a 90% sensitivity for the detection of polyps >10 mm. 4 Within a week, Kim 5 published a study comparing VC screening in 3120 patients with OC screening in 3163 patients. Remarkably, VC and OC found an equivalent number of advanced adenomas in each group; more surprisingly, a larger number of cancers were found in the VC group. 5 These 2 studies plus multiple prior published trials from the United States and abroad led the American Cancer Society, the American College of Radiology (ACR), and the United States Multi-Society Task Force to incoorate VC in its screening recommendations that were published in March 2008. 6
As VC has gained acceptance, gastroenterologists now realize that VC will impact their practice. After years of bashing VC as not being good enough and requiring more clinical data, the Future Trends Committee of the American Gastroenterological Association (AGA) published a report in October 2006 stating that they see the handwriting on the wall. 7 This Committee proposed that gastroenterologists should position themselves to play a role in performing and interpreting VC, including advocating for CPT codes in the 91000 series that will allow gastroenterologists to be reimbursed for interpreting and providing VC services, as well as developing specialized training and training requirements for those interested in performing VC interpretation. In an effort to make good on its promise, the AGA published a set of guidelines in 2007 listing the minimum requirements that a gastroenterologist must satisfy in order to become certified to read VC examinations. 8
Battle lines are drawn
Currently the Centers for Medicare and Medicaid Services (CMS) approve reimbursement for VC only when it follows a failed “diagnostic” colonoscopy, not a failed “screening” colonoscopy (Figure 2). 9 Following the inclusion of VC in the American Cancer Society's screening guidelines, CMS launched a National Coverage Analysis for Screening Computed Tomography Colonography for Colorectal Cancer (CAG-00396N) in May 2008. This seeks to expand reimbursement for screening indications. The final report of this analysis is due in February 2009. 10 Expanded reimbursement could have a huge impact on increasing screening and reducing CRC deaths, but it could also have substantial economic consequences for CMS and taxpayers. A public comment period held May-June 2008 drew responses from many individuals and organizations, including the ACR and the AGA. Of course, the ACR is in favor of expanded reimbursement, but the AGA stated that it would support VC only if certain conditions were met, 11 including:
- Reporting of ALL polyps (which is contradictory to the ACR Practice Guideline for the Performance of CTC in Adults that states reporting of polyps >5 mm is not recommended because of the low incidence of those lesions having malignant potential) 12 ;
- Allowing patients in consultation with their physician to determine whether or not to remove those polyps; and
- Enacting a coverage policy that would encourage rapid follow-up procedures (ie, colonoscopy) and that correspondingly would not create a disincentive for physicians (ie, gastroenterologists) who refer those procedures.
Reading between the lines, if such conditions are approved by CMS, then the gastroenterologists will have an unrestrained ability to perform colonoscopy on any little lump or bump that they might discover if they or their clinical assistant should be allowed to read VC exams. It is also the position of many prominent gastroenterologists to create a split-fee arrangement with radiologists so that radiologists will be relegated to reading only the extracolonic portions of a CT scan for a small portion of the professional fee, and, if radiologists refuse to participate, then they will outsource radiology services, even to foreign providers! 13
Dispelling popular myths
Gastroenterologists frequently try to discredit VC with the following myths:
- Colonoscopy is the “gold standard.” There are no published studies to validate this claim. In fact, studies comparing back-to-back colonoscopies on the same patients have reported OC miss rates of 22% for polyps, even in the hands of expert endoscopists. 14 Studies such as Pickhardt’s 15 landmark VC study have shown VC to outperform OC. Finally, the accuracy of screening colonoscopy has been shown tobe dependent on how much time a gastroenterologist spends performing the examination. 16
- If VC finds a polyp, then colonoscopy is needed for polyp removal, so why not undergo colonoscopy in the first place? The vast majority of polyps are benign, hyperplastic polyps, and <5% of the asymptomatic screening population has a significant adenomatous polyp. 5 Hence, if OC is the primary screening method, then >95% of the asymptomatic population would undergo OC unnecessarily with its inherent risks of bowel perforation and anesthesia.
- The radiation dose associated with VC is prohibitive. Radiation dose is a valid concern, but researchers are striving to mitigate this risk by using low-dose techniques, even as low as 10 mAs (compared with a conventional CT scan that might use a dose of 200 mAs). 17 Hence, the radiation risk from VC with low-dose techniques can be on the order of 1 to 2 mSv, which is far below the range that has been associated with potential cancer and multidetector CT use. 18 Alternatively, VC can be performed using MRI, but the availability of MRI scanners is a temporary hurdle, at least for today.
Actions to take
Radiologists are already overworked due to the exponential increase in imaging studies during the past decade, and as a result, we have become complacent about the ownership of new technologies. In the meantime, gastroenterologists are purchasing CT scanners and attending training programs to get ready for CMS approval of reimbursement for VC screening. 19 However, if radiologists act quickly and take certain steps to position ourselves to maintain control of VC, we will not risk losing this technology, as we have done with cardiac imaging. Some initiatives include:
- Taking a stronger, vocal interest in VC. Radiologists are better trained to read an entire CT examination, especially when disease crosses organ boundaries to involve both the colon and adjacent anatomy. We need to establish ourselves as the imaging experts in order to counter claims that endoscopists and nurse practitioners are as good as radiologists in reading VC exams. 20
- Beginning a dialogue with community gastroenterologists and primary care physicians. Radiology practices need to be willing to provide same-day, on-demand VC services for failed “diagnostic” colonoscopy examinations in advance of the anticipated reimbursementfor screening VC.
- Developing practice guidelines for appropriately working-up extracolonic findings. Perhaps offering immediate but limited ultrasound evaluation to resolve indeterminate liver and renal lesions will help to mitigate the gastroenterologists' cry that they should be the ones performing VC in their offices.
- Providing consistent, high-quality reports of VC findings that can be rapidly delivered to the patient and referring clinician. Utilization of the CT Colonography Reporting and Data System (C-RADS) and participation in the ACR’s CTC Registry will help to strengthen ourposition in the field. 21,22
- Challenging any proposals by gastroenterologists to split the professional fee for reading colonic and extracolonic portions of a VCCT scan, including legislative lobbying if necessary. There are many problems with fee-splitting arrangements, not the least of which is malpractice liability, radiologists will certainly be held liable when gastroenterologists fail to make a correct diagnosis if they should be allowed to interpret only the intraluminal portion of a VC scan.
All is not lost, at least not yet
Much of the rhetoric coming from the gastroenterology community is coming from a few but very vocal and rabid gastroenterologists. In fact, a survey of 2400 AGA members regarding their interest in VC resulted in only 588 responses, of which one third said that they would want to perform VC, another third said that they would not perform it but would support their colleagues, and the final third said that gastroenterologists should not perform VC. 23 In reality, radiologists and gastroenterologists will need to work together along with surgeons and oncologists to provide comprehensive CRC screening and treatment services. If CRC screening really takes off, then there will not be enough gastroenterologists available in this country to perform the necessary therapeutic colonoscopies that will be generated. Although radiologists specializing in VC may eventually become employees of large, multispecialty clinics specializing in colorectal disease, it is paramount that the role and expertise of the radiologist be maintained.
