Xanthogranulomatous pyelonephritis: The uncommon complications of the uncommon disease




Chronic xanthogranulomatous pyelonephritis (XGP) represents a rare type of granulomatous inflammation characterized by unilateral enlargement of a kidney, hydronephrosis and replacement of renal parenchyma by cysts containing serosanguinous fluid, with resultant loss of normal renal function. It frequently presents with recurrent non-healing subacute to chronic urinary infection and inflammation due to large obstructing or staghorn calculus. In our cases, along with classical CT findings of this uncommon disease, we present an unusual constellation of complications and disease severity, which are rarely reported despite the abundance of cases in the literature.3,6
In this report are two companion cases of diffuse and focal XGP with internal and external decompression, resulting in partial small bowel obstruction in the first case and osteomyelitis with nephrocutaneous fistula in the second case.
Patient 1
CASE SUMMARY
A 45-year-old woman with past medical history of rheumatoid arthritis and anemia presented to the emergency department with complaints of worsening abdominal pain, nausea and vomiting for three days. Review of systems was significant for unintentional weight loss of 14 pounds over the last two to three months with malaise and fatigue, in the absence of fever and chills. Patient also reported history of renal stones, but denied any dysuria or hematuria. Upon admission, the following laboratory test abnormalities were found: urinalysis showed 1+ occult blood, 3+ leukocyte esterase, >180 WBC/HPF, 7 RBS/HPF with mild anemia (Hgb 8) and leukocytosis (WBC 13) on CBC. Blood and urine cultures were negative.
IMAGING FINDINGS
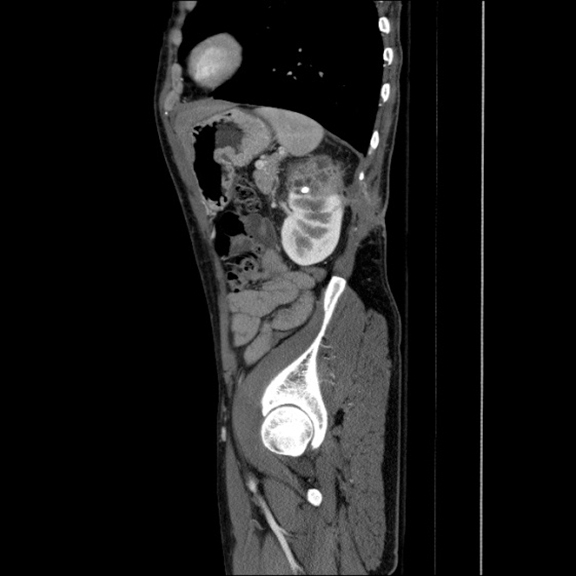
Contrast-enhanced CT abdomen and pelvis was obtained as part of the initial work-up for patient’s presenting complaints. CT revealed markedly abnormal appearance of the left kidney (Figure 1) with surrounding extensive inflammatory changes and small loculations of fluid throughout all of the retroperitoneal compartments, likely representing small urinomas and/or abscesses. Inflammation extended to the descending colon, body and tail of the pancreas, as well as small bowel mesentery resulting in partial small bowel obstruction. Final diagnosis was chronic diffuse XGP. Subsequent MAG3 scan revealed complete loss of renal function of the left kidney. Total left nephrectomy was recommended by urological surgery consult once small bowel obstruction resolves and patient is able to tolerate surgery.
Patient 2
CASE SUMMARY
A 48-year-old man with past medical history of non-healing ulcer on the left lower back for six months status post recent antibiotic treatment, presented to the hospital with dull left flank and back pain, generalized malaise and dysuria. At the time of admission, CBC and BMP demonstrated no abnormalities. On physical exam, patient had left flank tenderness with a large area of induration over left paraspinal muscles with central ulcer draining serosanguinous fluid. Urinalysis showed 1+ occult blood, 3+ leukocyte esterase, >180 WBC/HPF and 42 RBC/HPF. Urine and blood cultures were negative. Wound culture was positive for coagulase negative staphylococcus species.
IMAGING FINDINGS
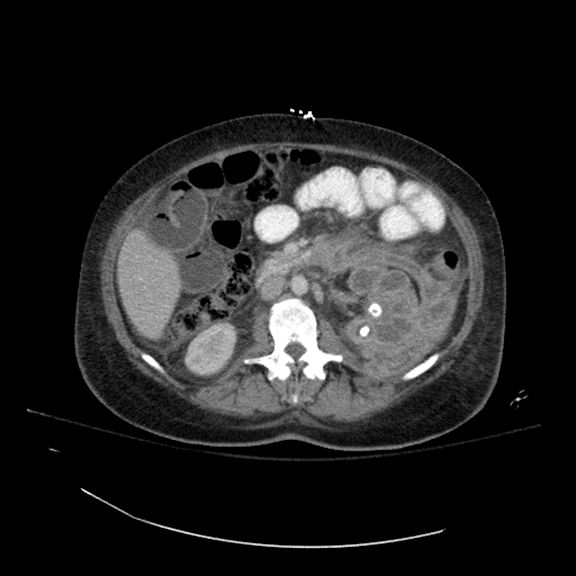
CT abdomen and pelvis revealed abnormal appearance of the upper pole of the left kidney (Figure 2) with inflammatory changes extending into posterior pararenal space, paraspinal muscles and subcutaneous tissues with fistulous tract to the skin surface, as well as sclerotic changes in 11th and 12th left posterior ribs concerning for osteomyelitis. Inflammatory changes were also present in the left paracolic gutter with wall thickening and enhancement of the short segment of descending colon surrounded by a small amount of free fluid. Patient was started on antibiotic therapy. MAG3 scan demonstrated absence of renal function of left upper pole, and normal function in lower pole with sharp demarcation of radioisotope uptake in the interpolar region. Partial nephrectomy was recommended by urologic surgery consult once patient completes antibiotic treatment for suspected osteomyelitis.
DISCUSSION
XGP is an uncommon chronic granulomatous renal infection resulting in loss of renal function. The renal tissue is replaced by xanthogranulomatous material and serosanguinous fluid filled cysts infiltrated by lipid-laden macrophages (foam cells). XGP can be focal or diffuse.2 There is no predilection for either kidney, with women being more commonly affected than men.
There is highly variable clinical presentation of XGP with acute symptoms of urinary tract infection (dysuria, hematuria, fever, chills and flank pain) or chronic, nonspecific symptoms (weight loss, malaise and anorexia). Etiologies of XGP include chronic renal obstruction, infection (e.g. E.Coli, Proteus mirabilis, Staphylococcus aureus), prolonged antibiotic use, abnormal lipid metabolism, lymphatic obstruction and renal ischemia.3
Although ultrasound can be used for initial assessment of patient with complicated UTI and suspected pyelonephritis, and can raise suspicion or diagnose XGP, a preferred radiologic modality is CT abdomen and pelvis with contrast as it provides highly specific imaging findings and accurate assessment of the renal involvement along with extrarenal extent of disease.1,5 CT scan usually reveals focal or diffuse enlargement of the involved kidney, with thinning of the cortex with dilated calyces with thick walls (“bear paw” sign), absence of function, and a large or “staghorn” calculus in the renal pelvis. Inflammatory changes may spread along the fascial planes throughout the retroperitoneum, commonly involving adjacent organs, such as pancreas and colon, or abdominal wall; CT examination provides excellent visualization of these findings, needed for adequate surgical planning.
CONCLUSION
XGP can present as indolent disease even in cases of internal/external decompression with an abscess/urinoma or fistula formation with only mild constitutional symptoms. Since chronic inflammation can lead to progressive renal tissue replacement and loss of renal function and affect adjacent organ systems, a prompt evaluation with contrast-enhanced CT is needed for adequate diagnosis to assess the extent and severity of the disease is advised.
REFERENCES
- Craig WD, Wagner BJ, Travis MD. Pyelonephritis: Radiologic-pathologic review. RadioGraphics. 2008;28(1):255-276.
- Fan CM, Whitman GJ, Chew FS. Xanthogranulomatous pyelonephritis. AJR Am J Roentgenol. 1995;165(4):1008-1008.
- Goldman SM, Hartman DS, Fishman EK, Finizio JP, Gatewood OM, Siegelman SS. CT of xanthogranulomatous pyelonephritis: Radiologic-pathologic correlation. AJR Am J Roentgenol. 1984;142(5):963-969.
- Beachley MC, Ranniger K, Roth F-J. Xanthogranulomatous pyelonephritis. AJR Am J Roentgenol. 1974;121(3):500-507.
- Kim JC. US and CT findings of xanthogranulomatous pyelonephritis. Clinical Imaging. 2001;25(2):118-121.
- Tolia BM, Iloreta A, Freed SZ, Fruchtman B, Bennett B, Newman HR. Xanthogranulomatous pyelonephritis: Detailed analysis of 29 cases and a brief discussion of atypical presentations. J Urol. 1981;(126):437-442.
Prepared by Dr. Motuzko while a PGY-3 Diagnostic Radiology Resident, and Dr. Germaine while serving as an Assistant Professor in Diagnostic Radiology, at Cooper University Hospital, Camden, NJ.
