45-year-old man with left-upper-quadrant abdominal pain
Images

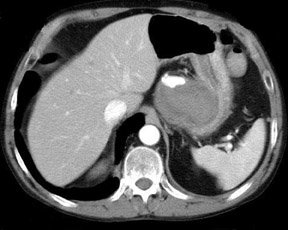

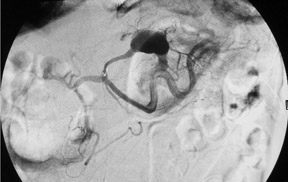


Ruptured intracystic pseudoaneurysm of the left gastric artery, which complicated pancreatitis
Findings
An initial noncontrast CT of the abdomen revealed a 9.9 × 6.0-cm hemorrhagic mass of the pancreatic body (Figure 1). A subsequent contrast-enhanced CT showed a 2.4-cm ruptured pseudoaneurysm of the left gastric artery within a large pancreatic pseudocyst (Figure 2). The patient was transferred to our hospital for endovascular treatment of his pseudoaneurysm. The left gastric artery was selectively injected and exhibited a leaking pseudoaneurysm (Figure 3).
Discussion
A visceral pseudoaneurysm is a serious complication of pancreatitis that occurs angiographically in up to 10% of the cases.1 The pathophysiology is proposed to be autodigestion of the peripancreatic arterial wall secondary to released proteolytic enzymes or erosion of a pseudocyst into the artery and conversion of its cavity into a pseudoaneurysm. The most commonly involved vessels include the splenic, gastroduodenal, and pancreaticoduodenal, which account for up to 90% of total pseudoaneurysm involvement.2 Involvement of the left gastric artery is very unusual, with only 5 cases published in the literature.2-5 Dahan et al4 described successful left gastric artery coil embolization of a ruptured pseudoaneurysm in 1997. The left gastric artery is rarely involved because of its cephalad position with relation to the pancreas. Our patient had a large 9.9-cm pseudocyst extending cephalad from the body of the pancreas, which extended into and abutted the left gastric artery. Subsequent arterial wall degradation led to pseudoaneurysm formation and rupture. Fortunately, the pseudoaneurysm was intracystic, which acted to partially tamponade the aneurysm rupture. Pseudo-aneurysm rupture in association with a pseudocyst, as in our case, is reported in 15% to 20% of cases.2 Recognition of this rare complication is extremely important; it has a reported mortality rate of up to 29% with treatment and up to 90% without treatment.6 Unusual complications have been described secondary to left gastric pseudoaneurysms, including hemosuccus pancreaticus (hemoductal pancreatitis) and wirsungorrhagia (direct pseudoaneurysm rupture into the duct of Wirsung).4,5 CT, angiography, and ultrasound have all been successful in the identification of the pseudoaneurysm and are acceptable diagnostic modalities. Both surgery and endovascular embolization have traditionally been proposed for treatment. Management of pseudo-aneurysms related to pancreatitis is essential because of the high mortality rate without treatment as described above.1,6,7 Surgical treatment of pseudoaneurysms is initially successful in 70% to 85% of cases but is also associated with mortality rates of 20% to 25%.8 There is a lower mortality rate of 16% reported if the pseudoaneurysm is in the body or tail of the pancreas.8 Percutaneous embolotherapy has a higher reported initial success rate of between 78% and 100% and a lower overall mortality rate of up to 16%.2,9-11 Recurrent hemorrhage with embolotherapy has been reported in up to 37% of cases.2 Catheter embolization options for peripancreatic pseudoaneurysms include metallic coils (as in our case), cyanoacrylate glue, gelatin sponge, interlocking detachable coils, ethiodized oil, particles of dura mater, vasopressin, and2,10,12,13 Direct percutaneous embolization with metallic coils or thrombin under fluoroscopic guidance was also proposed as a viable alternative by Araoz et al14 and Luchs et al.15 The most common technique reported uses a combination of metallic coils and a gelatin sponge. The only major embolic complication described in multiple studies was distal embolization of glue with resultant partial duodenal and partial splenic infarction.2,10 Both the surgical and endovascular literature proposes initial embolization in pancreatic head pseudoaneurysms, with subsequent surgical intervention, if necessary and possible, in the case of recurrent hemorrhage. Initial management of pseudoaneurysms adjacent to the pancreatic body and tail in surgical candidates is still controversial because of the relatively lower mortality rate in this region; such patients should be managed on a case-by-case basis.
Conclusion
Left gastric artery pseudoaneurysm is a rare but serious complication of pancreatitis. Only 5 cases were found in the literature. Although rare, vessels need to be followed and examined closely in pancreatitis and especially in pancreatic pseudocysts to make this potentially lifesaving diagnosis. Endovascular coiling is a minimally invasive and effective alternative to surgical intervention.
- White AF, Baum S, Buranasiri S. Aneurysms secondary to pancreatitis. AJR Am J Roentgenol. 1976;127:393-396.
- Boudghéne F, L’Hermainé C, Bigot JM. Arterial complications of pancreatitis: Diagnostic and therapeutic aspects in 104 cases. J Vasc Interv Radiol. 1993;4:551-558.
- Smith RE, Fontanez-Garcia D, Plavsic BM. Gastrointestinal case of the day. Pseudoaneurysm of the left gastric artery as a complication of acute pancreatitis. RadioGraphics. 1999;19:1390-1392.
- Dahan H, Arrivé L, Monnier-Cholley L, et al. Imaging of a case of wirsungorrhagia [in French]. J Radiol. 1997;78:589-591.
- Kapoor S, Rao P, Pal S, Chattopadhyay TK. Hemosuccus pancreaticus: An uncommon cause of gastrointestinal hemorrhage. A case report. JOP. 2004;5:373-376.
- Stabile BE, Wilson SE, Debas HT. Reduced mortality from bleeding pseudoaneuryms and pseudoaneurysms caused by pancreatitis. Arch Surg. 1983;118:45-51.
- Mandel SR, Jaques PF, Sanofsky S, Mauro MA. Nonoperative management of peripancreatic arterial aneurysms. A 10-year experience. Ann Surg. 1987;205:126-128.
- Itani MS, Sumrani N. Pancreatic pseudoaneurysm. EMedicine 2002; topic 2732. Available at http://www.emedicine.com. Accessed March 4, 2005.
- Salam TA, Lumsden AB, Martin LG, Smith RB 3rd. Nonoperative management of visceral aneurysms and pseudoaneurysms. Am J Surg. 1992;164:215-219.
- Gabelmann A. Görich J, Merkle EM. Endovascular treatment of visceral artery aneurysms. J Endovasc Ther. 2002;9:38-47.
- Vujic I, Andersen BL, Stanley JH, Gobien RP. Pancreatic and peripancreatic vessels: Embolization for control of bleeding in pancreatitis. Radiology. 1984;150:51-55.
- Hama Y, Kaji T, Iwasaki Y, et al. Transcather embolization of a superior mesenteric artery pseudoaneurysm. A case report. Acta Radiol. 1999;40:649-651.
- Schoder M, Cejna M, Längle F, et al. Glue embolization of a ruptured pseudoaneurysm via the gastroduodenal artery. Eur Radiol. 2000;10:1335-1337.
- Araoz PA, Andrews JC. Direct percutaneous embolization of visceral artery aneurysms: Techniques and pitfalls. J Vasc Interv Radiol. 2000;11:1195-1200.
- Luchs SG, Antonacci VP, Reid SK, Pagan-Marin H. Vascular and interventional case of the day. Pancreatic head pseudoaneurysm treated with percutaneous thrombin injection. AJR Am J Roentgenol. 1999;173:830-834.