Accessory ossicles and sesamoid bones: Spectrum of pathology and imaging evaluation




















Dr. Kalantari is a Radiology Resident, Dr. Seeger is a Professor and Chief, Musculoskeletal Radiology, Dr. Chow is an Assistant Clinical Professor, and Dr. Motamedi is an Assistant Clinical Professor, Department of Radiology, David Geffen School of Medicine at UCLA, Los Angeles, CA. Presented in part at the 106th Annual Meeting of the American Roentgen Ray Society, Vancouver, Canada, May 2006.
Accessory bones, or ossicles, are considered to be normal anatomic variants. Sesamoid bones are ovoid nodular bones, often small, found embedded within a tendon or joint capsule. Although accessory ossicles and sesamoid bones are generally considered clinically insignificant anatomic variations, they can become symptomatic. Traumatic conditions include acute fracture, stress fracture, and pseudarthrosis. Neoplastic and arthritic conditions are also encountered, as well as inflammatory and degenerative disorders.
This article reviews a spectrum of accessory ossicle and sesamoid pathology and provides guidelines for the preferred imaging modality for the suspected abnormality. We discuss some of the more commonly symptomatic bones, namely the os acromiale, os styloideum, metacarpal and hallux sesamoids, patella, os trigonum, os calcaneus secundarius, accessory navicular, os peroneum, and os intermetatarseum.
Os acromiale
There are normally 3 acromial ossification centers that fuse between 22 and 25 years of age. An os acromiale results from the failure of 1 of these centers to fuse. The anterior ossification center is termed the pre-acromion, the middle is the meso-acromion, and the posterior is the meta-acromion. The basi-acromion forms the point of attachment of these 3 ossification centers to the scapula. A number of subtypes of os acromiale have been described. The most common variant is nonfusion between the meso- and meta-acromion. 1 The prevalence of os acromiale in radiographic and anatomic studies ranges between 1% and 15%.
An os acromiale can contribute to shoulder impingement symptoms. Contraction of the deltoid muscle may pull the os acromiale downward, causing it to impinge on the rotator cuff. 2-4 Abnormal motion may lead to an osteophytic spur at the pseudarthrosis, which may also impinge on the cuff.
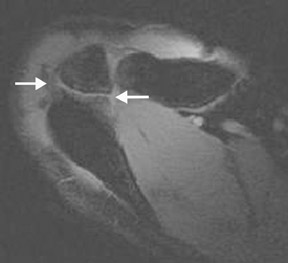
The diagnosis of os acromiale may be made on axillary projection radiographs, computed tomography (CT), or magnetic resonance imaging (MRI). MRI may show marrow edema and degenerative changes at a pseudarthrosis (Figure 1).
Os styloideum (carpal boss)
The os styloideum is an ununited bony protuberance, located on the dorsum of the wrist at the base of the second and third metacarpals. The association between dorsal wrist pain or fatigability and an os styloideum is known as carpal bossing (carpe bossu disease). Symptoms of carpal bossing may result from osteoarthritis, an overlying ganglion or bursitis, or from an extensor tendon slipping over the ossicle. 5
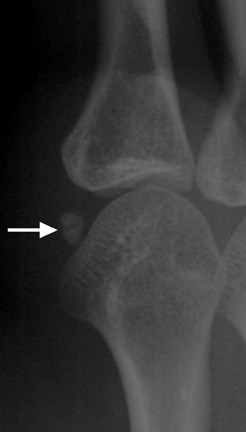
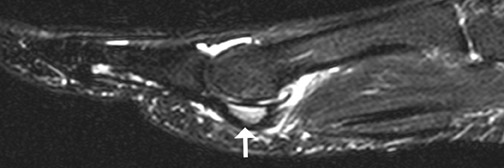
The lateral radiographic view best profiles the os styloideum (Figure 2). CT may show degenerative disease at a pseudarthrosis, and MRI will show edema related to abnormal motion (Figure 2).
Sesamoid bones of the hand
Most people have 5 sesamoid bones in each hand: 2 at the thumb metacarpophalangeal (MCP) joint, 1 at the interphalangeal joint of the thumb, 1 at the MCP joint of the index finger, and 1 at the MCP joint of the small finger. 6 Traumatic, inflammatory, and arthritic conditions can affect the sesamoid bones of the hand. Thumb sesamoid fractures usually result from hyperextension injury to the MCP joint. These fractures may be associated with rupture of the palmar plate or accessory collateral ligaments. 7 Radiography is usually sufficient for diagnosis; however, oblique views are often necessary for the diagnosis of a fracture (Figure 3).
Patella
Patella fractures are usually transverse, often resulting from rapid flexion against a fully contracted quadriceps. Osteochondral fractures may result from a direct blow or patellar dislocation. Children are vulnerable to this type of fracture because of patellar mobility.
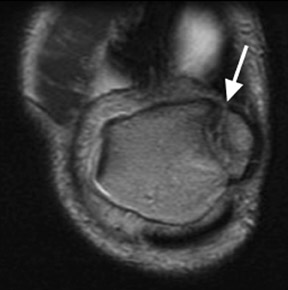
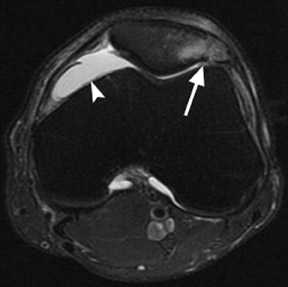
Differentiation of an acute patella fracture from a bipartite patella may be difficult. The bipartite patella is a synchondrosis, found in 1% to 2% of the population (Figures 4 and 5). Bipartite patellas are classified into 3 types. Type I is located at the inferior pole (5% of all cases), type II is at the lateral patellar margin (20%), and type III is at the superolateral margin (75%). Most (98%) remain asymptomatic, but direct trauma may disrupt the synchondroses (Figure 4). 8 A dorsal defect of the patella is sometimes associated with bipartite or multipartite patella, which is seen as a focal lucency in the superolateral patella covered by articular cartilage (Figure 5). 9
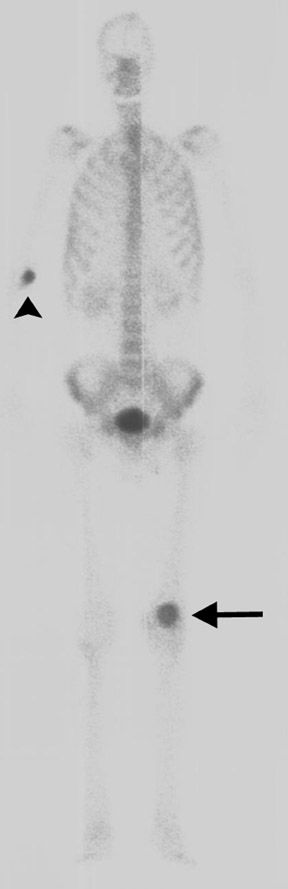
Other categories of disease that affect the patella include degenerative or metabolic disease and benign or malignant primary or metastatic tumors (Figures 6 and 7). Reported tumors include chondroblastoma, histiocytosis, giant cell tumor, simple bone cyst, brown tumor of hyperparathyroidism, hemangioma, osteochondroma, lipoma, and osteoblastoma. Malignant tumors include lymphoma and hemangioendothelioma. Metastatic tumors and myeloma are rare.
Os trigonum
Between 8 and 13 years of age, an ossification center forms posterior to the talus. Normally, this ossification center fuses with the talus within 1 year. In approximately 7% of the population, it remains separate and is referred to as the os trigonum. The os trigonum is corticated and articulates with the lateral talar tubercle through a synchondrosis. Os trigonum syndrome results from repetitive microtrauma or acute forced plantar flexion of the foot. The chondro-osseous border of the synchondrosis may be injured either as a chronic stress fracture or, less frequently, as an acute fracture. 10
An os trigonum is usually round or oval with well-defined corticated margins, whereas a fracture of the lateral tubercle typically has irregular serrated margins between the fragment and the posterior talus. Lateral radiographs obtained with the foot in plantar flexion may show the os trigonum impinged between the posterior tibia malleolus and the calcaneal tuberosity (Figure 8). MRI is very useful in establishing the diagnosis of os trigonum syndrome (Figure 8). Because of its location between the medial and lateral talar tubercles, inflammatory changes may be seen in the flexor hallucis longus tendon in patients with os trigonum syndrome. 10
Os calcaneus secundarius
The os calcaneus secundarius is an accessory ossicle of the anterior facet of the calcaneus, which may be mistaken for a fracture of the anterior process. Radiographically, the os calcaneus secundarius is best seen on the medial oblique view (Figure 9). Although it is uncommon for an os calcaneus secundarius to cause symptoms, range of motion of the subtalar joint may be limited by the ossicle, clinically resembling a calcaneonavicular coalition. 11
Accessory navicular (os tibiale externum, os naviculare secundarium)
There are 3 types of accessory navicular. 12,13 Type I, or os tibiale externum, occurs when an ossification center forms a sesamoid bone within the tibialis posterior tendon, near the navicular insertion. Type I ossicles are generally well-defined round or oval bones, measuring approximately 2 to 3 mm in diameter, and are located up to 5 mm medial and posterior to the medial aspect of the navicular. In type II accessory navicular, the ossification center measures approximately 9 to 12 mm in size, and resides adjacent to the tubercle of the navicular bone. A residual cartilaginous synchondrosis joins the triangular type II ossicle approximately 1 to 2 mm medial and posterior to the navicular. The majority or entire tibialis posterior tendon inserts on the type II accessory ossicle. The type III accessory navicular, or cornuate navicular, is a prominent navicular tuberosity, which is essentially a type II ossicle connected to the medial aspect of the parent navicular by an osseous bridge.
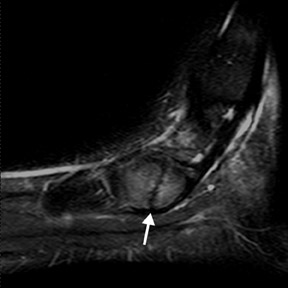
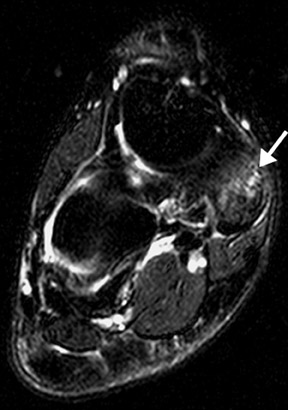
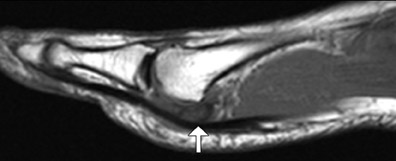
Of the 3 patterns, the type II accessory navicular is most commonly associated with medial foot pain. 14,15 A valgus stress injury may fracture the synchondrosis, resulting in abnormal motion. MRI is the most specific imaging modality for detecting the symptomatic accessory navicular, showing edema in the bone and soft tissues (Figures 10 and 11).
Os peroneum
The os peroneum is an oval or round ossicle located within the substance of the distal peroneus longus tendon near the cuboid. Fractures of the os peroneum result from direct trauma or indirect stress from dorsiflexion of the foot (Figure 12). Fractures of the os peroneum are typically associated with peroneus longus tendon dysfunction, which may be either acute or chronic. 16,17
Os intermetatarseum
Os intermetatarseum is present in approximately 1% of feet. It is situated superiorly between the first and second metatarsal bases. 18 It may articulate with the medial cuneiform or be attached to the first metatarsal base. The ossicle is best visualized on the anteroposterior view. It may be round, oval, kidney-shaped, linear, or even resemble a rudimentary metatarsal (Figure 13). Although infrequently symptomatic, an os intermetatarseum may cause dorsal midfoot pain from compression of the medial branch of the deep peroneal nerve.
Hallux sesamoids
The hallux sesamoids can be associated with acute or stress fractures. 18 Although much less common than stress fractures, avascular necrosis of the hallux sesamoid bones should be considered in the differential diagnosis of persistent forefoot pain. 19 The tibial sesamoid is more likely to fracture than the fibular sesamoid because of weight-bearing mechanics (Figure 14). 20 Compared with a fractured sesamoid, a bipartite bone is usually larger and has smooth margins.
In addition to standard radiographic views, an axial sesamoid projection is often helpful. MRI will show edema if the bone is fractured (Figure 15).
Conclusion
We have reviewed a spectrum of pathology involving accessory ossicles and sesamoid bones. These normal anatomic variations may, in fact, represent the source of patient symptomatology. The identification of key imaging characteristics can help determine whether or not to attribute clinical symptoms to these structures.
