Acute quadriplegia in a patient with bacterial pericarditis
Images


CASE SUMMARY
A 53-year-old male presented with fevers and acute onset, progressive weakness involving all four extremities over the course of three days. His past medical history was significant for an episode of treated Streptococcus (unspeciated) pericarditis, diagnosed nine months prior to current presentation. No recent history of trauma, IV drug abuse, or spinal surgery was reported.
On admission, the patient was afebrile. Neurologic evaluation revealed normal mental status with intact cranial nerves. Strength was completely absent in both lower extremities, though 3/5 in both upper extremities, with hypoesthesia below the nipple line. No meningeal signs were reported.
Admission laboratory values showed an elevated white blood count of 21.1 K/mcL with slightly elevated C-reactive protein. Cerebrospinal fluid and blood cultures yielded no growth. A transthoracic echocardiogram revealed normal left ventricular size and function, without evidence of vegetations or pericardial effusion.
IMAGING FINDINGS
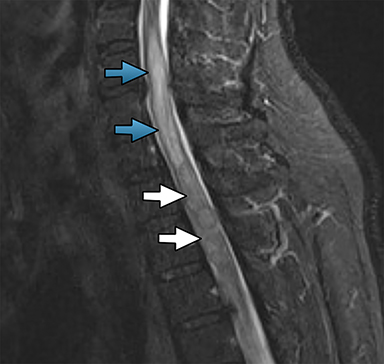
Magnetic resonance imaging (MRI) of the thoracic spine demonstrated heterogeneous STIR-weighted signal abnormality involving the T1 to T3 levels with extensive surrounding edema. T1-weighted imaging demonstrated corresponding hypointense signal abnormality. Post-contrast imaging revealed a thin rim of enhancement surrounding the lesion (Figure 1). There was no evidence of spondylodiscitis or epidural abscess. Given the rapid clinical presentation, these findings raised the suspicion for an intramedullary spinal cord abscess (ISCA).
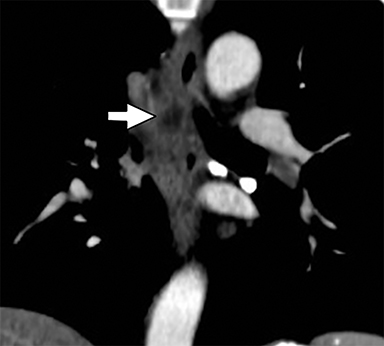
Subsequent computed tomography (CT) of the chest, abdomen, and pelvis demonstrated a peripherally enhancing fluid collection in the subcarinal/paraesophageal region worrisome for suppurative lymph node/abscess (Figure 2). No additional sources of infection were identified.
The patient developed complete quadriplegia with fecal incontinence soon after the MRI. An emergent decompression of the thoracic spine was performed with an intraoperative ultrasound confirming liquefied material within the upper thoracic spinal cord, compatible with intramedullary abscess formation. Myelotomy resulted in drainage of purulent fluid. Following the procedure, intravenous vancomycin, cefepime, and a steroid regimen were initiated. Cultures from the purulent material were positive for Streptococcus viridans.
Postoperatively, the patient regained partial return of upper extremity motor function, though demonstrated persistent paraplegia with persistent hypoesthesia below the nipple line. He was ultimately discharged to a rehabilitation center where physical and occupational therapy were initiated.
DIAGNOSIS
Intramedullary spinal cord abscess
DISCUSSION
The spinal cord fluid culture from our patient grew Streptococcus viridans, which is a known causative agent of indolent pericarditis.3 Although the pericardial fluid cultures from the patient’s initial presentation yielded no growth, the corresponding gram stain did show gram positive cocci in pairs compatible with Streptococcus bacterium. We theorize that the causative agent for the patient’s prior episode of pericarditis was S. viridans. The infection then spread from the pericardium to the subcarinal/paraesophageal region via the submesothelial lymphatics4 and entered the bloodstream before seeding the spinal cord. Alternatively, Batson’s venous plexus may have served as a pathway for the spread of infection. Our review of the literature demonstrates that this is the first reported case of ISCA secondary to bacterial pericarditis.
ISCAs are exceedingly uncommon, having been reported approximately 100 times in the literature,1 with the majority of these cases are attributed to staphylococcus and streptococcus species.2 While most reports in children are associated with spinal dysraphisms,5 the most common origin in adults is hematogenous, often secondary to an aggressive lung infection or endocarditis.6,7 Symptoms on presentation vary depending on the location of the lesion, and can include back pain, motor/sensory deficits, urinary incontinence, and/or fever.1,6
As spinal cord abscesses expand, they spread along white matter tracts and create mass effect on the surrounding cord parenchyma. Early diagnosis of a suspected ISCA requires a contrast-enhanced MRI, the preferred modality due to its detailed characterization of spinal canal structures. The imaging features of a T2/STIR hyperintense lesion within the cord as well as peripheral enhancement and surrounding medullary edema in the setting of rapid onset neurological compromise are most suggestive of an ISCA.2 The characteristic expansion of the cord by intramedullary cord abscesses helps distinguish these lesions from extramedullary infections. The primary imaging-based differential diagnosis includes intramedullary neoplasms, such as ependymomas and astrocytomas, both of which can present as T1 iso to hypointense and T2 hyperintense lesions with associated areas of enhancement, with the former frequently containing areas of hemorrhage.8 However, often times imaging alone is not sufficient to distinguish these entities. Ultimately, a thorough history and physical exam is essential, as the clinical presentation of neoplasms is classically that of gradual neurological decline. In the pediatric population, MRI not only aids in diagnosis but also provides value in excluding the presence of a congenital dermal sinus, an important risk factor for spinal cord abscesses in younger patients.6
Urgent surgical intervention, involving targeted laminectomy and myelotomy, followed by long term antibiotic therapy are the standard of care in limiting neurologic sequelae and improving overall functional status.5 If not treated promptly, prognosis is often poor with limited neurological recovery and possible mortality.6,9
CONCLUSION
Although extremely rare, the diagnosis of ISCA is essential for the radiologist to consider in a patient with rapid neurologic decline. If not treated in the acute setting, these infections can result in extremely unfavorable outcomes. Although intramedullary neoplasms can mimic the imaging appearance of ISCA, diagnosis can be made in conjunction with imaging findings and a thorough history and exam.
REFERENCES
- Candon E, Frerebeau P. Bacterial abscesses of the spinal cord: Review of the literature (73 cases). Revue Neurol. 1994;150(5):370-376.
- Condette-Auliac S, Lacour J, Anxionnat R, Braun M, Wagner M, Moret C, Bracard S, Picard L. MRI aspects of spinal cord abscesses: Report of 5 cases and review of the literature. J Neuroradiology. 1998 Oct;25(3):189-200.
- Tu C, Cheng S, Yang S, Hsieh T, Jiau S. Indolent purulent pericarditis due to viridans streptococcus infection successfully treated by pericardiocentesis and penicillin G. Acta. Cardiology Sinica. 2008; 24:1136.2.
- Venuta F, Rendina E. The lymphatic system in thoracic oncology. Thorac Surg Clin. 2012; 22(2):ix-x.
- Al Barbarawi M, Khriesat W, Qudsieh S, Qudsieh H, Loai AA. Management of intramedullary spinal cord abscess: Experience with four cases, pathophysiology and outcomes. Eur Spine J. 2009;18(5):710-717.
- Iwasaki M, Yano S, Aoyama T, Hida K, Iwasaki Y. Acute onset intramedullary spinal cord abscess with spinal artery occlusion: a case report and review. Eur Spine J. 2011;20:S294-S301.
- Fernandez-Ruiz M, Lopez-Medrano F, Garcia-Montero M, Hornedo-Mugiro J, Aguado J. Intramedullary cervical spinal cord abscess by viridans group Streptococcus secondary to infective endocarditis and facilitated by previous local radiotherapy. Intern Med. 2009;48(1):61-64.
- Koeller KK, Rosenblum RS, Morrison AL. Neoplasms of the spinal cord and filum terminale: Radiologic-pathologic correlation. Radiographics. 2000;20(6):1721-1749.
- Kurita N, Sakurai Y, Taniguhi M, Terao T, Takahashi H, Mannen T. Intramedullary spinal cord abscess treated with antibiotic therapy: Case report and review. Neurol Med Chir. 2009;49:262-268.
Citation
P S, R C, P R.Acute quadriplegia in a patient with bacterial pericarditis. Appl Radiol. 2017; (2):35-37.
February 8, 2017