Anterior cerebral artery vasculopathy secondary to miliary TB
Images
CASE SUMMARY
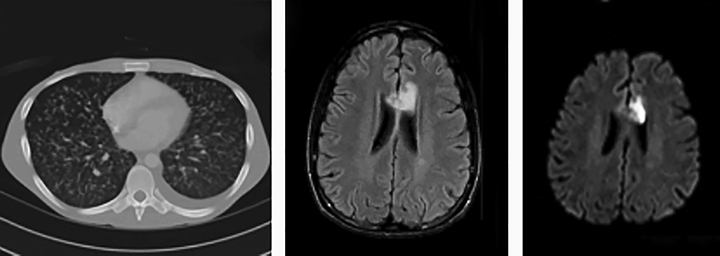
A 28-year-old male patient, recently diagnosed with HIV infection and miliary tuberculosis (TB) based on characteristic chest CT findings and positive sputum culture, presented to the emergency department with new onset of ataxia (Figure 1A).
IMAGING FINDINGS
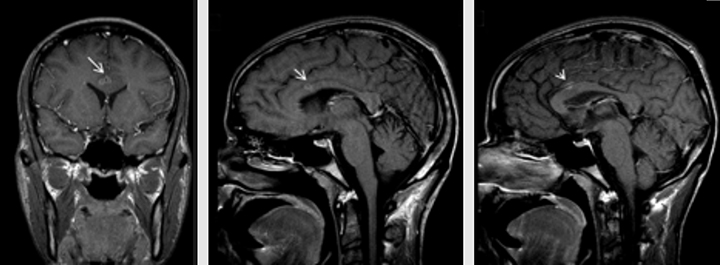
Brain MRI revealed several ring enhancing foci in supratentorial brain consistent with TB granulomas with associated acute infarction in anterior body of corpus callosum (Figure 1B, Figure 1C; Figure 2). Post-contrast images demonstrated linear enhancement surrounding pericallosal arteries consistent with vasculitis. MRI of the cervical spine was unremarkable. The patient’s medical condition improved in the following weeks after starting four drug regimens (isoniazid, ethambutol, pyrazinamide and rifampin) for TB, as well as the Highly Active Antiretroviral Therapy (HAART), and he was discharged.
DIAGNOSIS
Anterior cerebral artery vasculopathy secondary to miliary TB
DISCUSSION
Infectious vasculitis of the CNS may be caused by a variety of pathogens such as EBV, HBV, HCV and TB.1,2 The underlying mechanisms include direct invasion of the vessel wall, deposition of immune complex and cryoglobulinemia.3 Disseminated mycobacterial infection may involve CNS and present as meningitis, abscesses, encephalomyelitis as well as the less common stroke-like infarcts in the setting of cerebral vasculitis.4-6 With regard to CNS vasculitis, disseminated TB may both directly invade the vessel walls as in our patient, or elicit an inflammatory reaction that mostly affects the small cerebral vessels. Although rare, the clinical features of CNS vasculitis caused by TB vary from acute headaches, seizures and focal neurologic deficits to chronic confusion states and personality changes. Therefore, both the clinical and radiological diagnosis of CNS vasculitis in the setting of disseminated TB is challenging. In particular, this diagnosis should be considered in any young and immunocompromised patient that presents with neurologic signs and symptoms that can be explained by multiple infarcts in various vascular territories.7 In fact, most of the previous studies about infectious CNS vasculitis reported a variety of neurologic signs and symptoms as the presenting manifestation; however, our patient only presented with ataxia that may be explained by the early-stage and limited involvement of the brain. In terms of radiologic findings, presence of stroke-like lesions in different stages possibly secondary to spasm or occlusion of the arteries should prompt suspicion for TB vasculitis,7 especially in the immunocompromised patient. Moreover, other etiologies such as toxoplasmosis and lymphoma which are more common causes of neurologic involvement of HIV patients should also be considered.
CONCLUSION
TB granulomas can cause focal vasculitis of intracranial arteries resulting in brain infarction. Imaging findings include single or multiple ring enhancing granulomas with associated vascular wall enhancement. Familiarity of radiologists with this entity is essential.
REFERENCES
- Castro Caldas A, Geraldes R, Neto L, et al. Central nervous system vasculitis associated with hepatitis C virus infection: a brain MRI-supported diagnosis. J Neurol Sci. 2014;336(1-2):152-154.
- Carod Artal FJ. Clinical management of infectious cerebral vasculitides. Expert Rev Neurother. 2016;16(2)205-221.
- Scolding NJ. Central nervous system vasculitis. Semin Immunopathol. 2009;31(4)527-536.
- Pandit V, Valsalan R, Seshadri S, et al. Disseminated tuberculosis presenting as mesenteric and cerebral abscess in HIV infection: case report. Braz J Infect Dis. 2009;13(5)383-386.
- Masoodi I, Farooq O, Ahmad I, et al. Acute disseminated encephalomyelitis as the first presentation of CNS tuberculosis: report of a case with brief review. Ger Med Sci. 2010;8:Doc32.
- Kondo A, Mori K, Iwata J, et al. Caseous necrotic granuloma in the pituitary stalk due to nontuberculous Mycobacteria (Mycobacterium tokaiense) infection: case report. Neurol Med Chir (Tokyo). 2006;4680-83.
- Wang Y, Li Q, Zhen X, et al. Immunologic cerebral vasculitis and extrapulmonary tuberculosis: an uncommon association. J Clin Diagn Res. 2015;9(9)OD03-OD05.
Citation
S E, K P, SA N.Anterior cerebral artery vasculopathy secondary to miliary TB. Appl Radiol. 2017; (12):16-17.
December 7, 2017