Anti-NMDA receptor encephalomyelitis
Images



CASE SUMMARY
A 17-year-old female presented with two days of acute psychosis, which progressed to catatonia and unresponsiveness. During the first several days of inpatient admission, she experienced progressive bilateral extremity clonus, hyperreflexia, and urinary retention. Lumbar puncture revealed CSF lymphocyte-predominant pleocytosis and also oligoclonal bands, indicating intrathecal synthesis of immunoglobulin. EEG showed generalized slowing with diffuse delta brushes, consistent with encephalopathy.
IMAGING FINDINGS
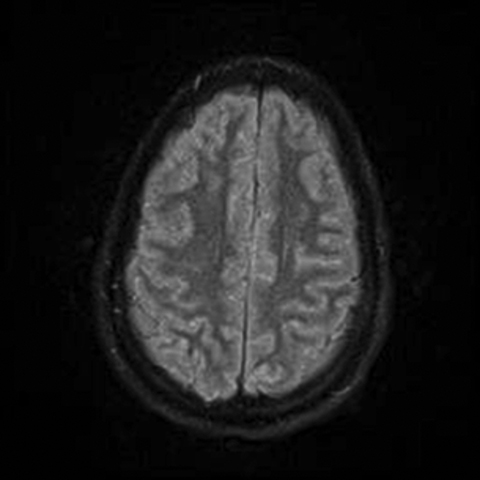
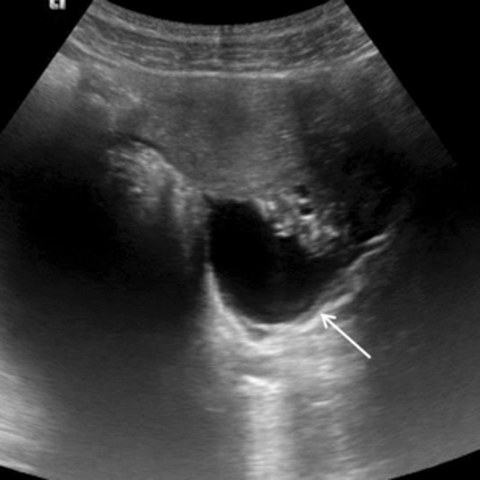
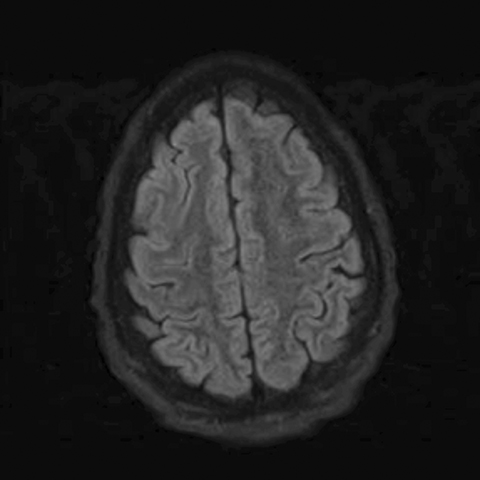
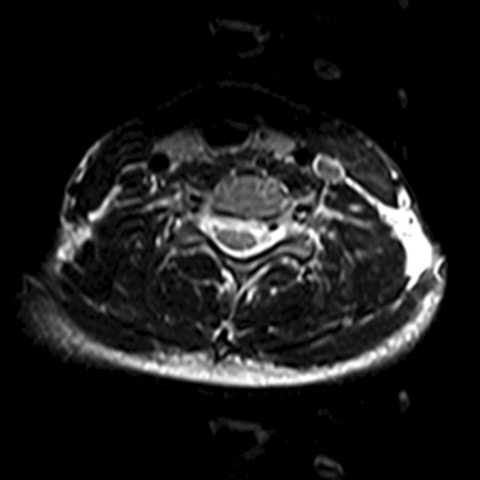
MRI of the brain and spine was obtained approximately one week after admission. The FLAIR sequence of the brain revealed abnormal sulcal hyperintensity over the cerebral convexities (Figure 1) (the patient was not on supplemental oxygen). T2WI of the spine demonstrated mild abnormal hyperintensity within the central portion of the cervical spinal cord (Figure 2), without associated enhancement. An axial image of the lumbosacral spine incidentally demonstrated a cystic left adnexal mass (Figure 3a), confirmed on a subsequently performed pelvic ultrasound (Figure 3b); a differential diagnosis of simple cyst versus cystic teratoma was provided.
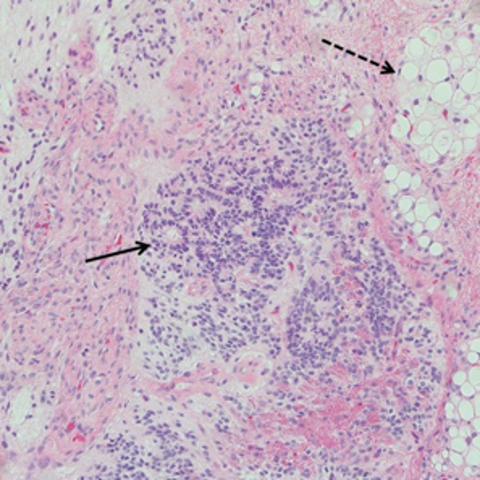
Due to the brain and spine imaging findings, and in combination with the cystic adnexal mass, autoimmune encephalitis was suspected. An autoimmune panel was obtained, and the CSF anti-NMDA receptor antibody level was found to be positive at a 1:4 dilution. The patient subsequently underwent left oophorectomy, which confirmed the presence of a left ovarian immature teratoma (Figure 4).
The patient was treated for anti-NMDA receptor encephalomyelitis with immunosuppressive therapy, including rituximab and steroids, and plasmapheresis. Gradual improvement in mental status and motor function followed. By four months post-admission, the patient had returned to baseline status with the exception of mild residual extremity weakness. Post-treatment follow-up brain and spine MRI showed resolution of the previous imaging findings (Figure 5).
DIAGNOSIS
Anti-NMDA receptor encephalomyelitis
DISCUSSION
Anti-NMDA receptor encephalitis is an autoimmune syndrome which has become increasingly recognized since its discovery in 2007.1,2 This syndrome disproportionately affects women (10:1 female to male ratio in one series), and as many as 25% of patients may have severe outcomes including prolonged deficits or death.3
Typical clinical features of anti-NMDA receptor encephalitis include a prodromal fever or headache, followed by psychiatric symptoms such as mood disorders, psychosis, unresponsiveness, catatonia, dyskinesia, memory problems, autonomic instability, and hypoventilation. Cardiac dysrhythmias and seizures have been described. Laboratory findings include CSF pleocytosis, oligoclonal bands, and detection of anti-NMDA receptor antibodies.1,3,4
Brain MRI in anti-NMDA receptor encephalitis can be normal, or can show variably distributed parenchymal T2/FLAIR hyperintensities or foci of enhancement, often in the medial temporal and parietal lobes, with or without mild meningeal enhancement.1,2,5 The imaging findings appear to correlate with the pathologic findings, which include parenchymal atrophy, gliosis, and IgG deposits predominantly involving temporal lobes and hippocampi with a lesser degree of involvement in the neocortex, basal ganglia, basal forebrain, and rarely the cerebellum. Mild inflammatory infiltration of the leptomeninges can be seen. B-cells and plasma cells are found in perivascular spaces.1
A key feature of this diagnosis is that it is frequently associated with ovarian teratomas (59%). Other associations include various autoimmune syndromes and viral encephalitides.1,3,4,6,7 In rare cases, anti-NMDA receptor antibodies have been described with other tumor types, including small cell lung cancer, sex-cord stromal tumor, testicular or mediastinal teratoma, lymphoma, neuroblastoma, and neuroendocrine tumor.2,3
Identification of tumor is critical, because tumor patients have a more robust immune response and better outcomes are associated with early tumor resection.3 Other prognostic factors include severity and type of symptoms, including duration of catatonia.4 Treatment typically includes high-dose steroids with IVIG, plasmapheresis, cyclophosphamide, and/or rituximab.3,4
The mechanism underlying the development of teratoma-related NMDA receptor autoantibodies has been suggested to be innate immune reaction against mature or immature neuronal cells within a teratoma. Subsequently, as distant NMDA-expressing neural tissues become targeted by antibodies, new antigens can become exposed, fostering the development of “epitope spreading” with the appearance of additional anti-neuronal autoantibodies. These may include anti-myelin basic protein, ANA, thyroid-peroxidase antibodies, and anti-dsDNA.1,5,7,8
Relative to encephalitis, myelitis is a rare association with anti-NMDA receptor antibody syndrome. Symptoms include difficulty walking, lower extremity sensory deficit, urinary incontinence, and flaccid paraplegia, reported to occur both before6,8 or after5,9,10 onset of encephalitis symptoms. Imaging findings include multifocal or longitudinally extensive hyperintense lesions of the spinal cord on T2WI, with or without enhancement. Spinal cord pathologic findings include IgG deposition, microglial nodules at the ventral horns, endoneural edema, and Wallerian degeneration.1 Reported treatment course and outcomes are similar to the more common encephalitis cases.
CONCLUSION
Anti-NMDA receptor encephalomyelitis is an increasingly recognized autoimmune syndrome. Females are affected most commonly, and there is a frequent association of this syndrome with the presence of underlying ovarian teratoma. Myelitis is an uncommon manifestation of this syndrome, but should be considered in the appropriate setting in patients with acute myelopathy. Early recognition and treatment are important for optimal patient outcome.
REFERENCES
- Tüzün E, Zhou L, Baehring JM, et al. Evidence for antibody-mediated pathogenesis in anti-NMDAR encephalitis associated with ovarian teratoma. Acta Neuropathol. 2009 Dec;118(6):737-743.
- Dalmau J, Lancaster E, Martinez-Hernandez E, et al. Clinical experience and laboratory investigations in patients with anti-NMDAR encephalitis. Lancet Neurol. 2011 Jan;10(1):63-74.
- Dalmau J, Gleichman AJ, Hughes EG, et al. Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol. 2008 Dec;7(12):1091-1098.
- DeSena AD, Greenberg BM, Graves D. Three phenotypes of anti-N-methyl-D-aspartate receptor antibody encephalitis in children: prevalence of symptoms and prognosis. Pediatr Neurol. 2014 Oct;51(4):542-549.
- Kruer MC, Koch TK, Bourdette DN, et al. NMDA receptor encephalitis mimicking seronegative neuromyelitis optica. Neurology. 2010 May 4; 74(18):1473–1475.
- Outteryck O, Baille G, Hodel J, et al. Extensive myelitis associated with anti-NMDA receptor antibodies. BMC Neurol. 2013;13:211.
- Schäbitz WR, Rogalewski A, Hagemeister C, Bien CG. VZV brainstem encephalitis triggers NMDA receptor immunoreaction. Neurology. 2014 Dec 9;83(24):2309-2311.
- Pennington C, Livingstone S, Santosh C, et al. N-methyl D-aspartate receptor antibody encephalitis associated with myelitis. J Neurol Sci. 2012 Jun 15;317(1-2):151-153.
- Taylor RB, Mason W, Kong K, et al. Reversible paraneoplastic encephalomyelitis associated with a benign ovarian teratoma. Can J Neurol Sci. 1999 Nov;26(4):317-320.
- Lekoubou A, Viaccoz A, Didelot A, et al. Anti-N-methyl-D-aspartate receptor encephalitis with acute disseminated encephalomyelitis-like MRI features. Eur J Neurol. 2012 Feb;19(2):e16-7.
Citation
K PJM, S L, S P. Anti-NMDA receptor encephalomyelitis. Appl Radiol. 2016;(12):35-37.
December 9, 2016