Scimitar syndrome
By Gustainyte V, Miller M, Towbin T, Towbin AJ, Neville Kucera J





CASE SUMMARY
After a 20-week routine fetal anatomy scan, a 31-year-old G1P0 female was referred for a fetal echocardiogram for a suspected ventricular septal defect. The fetal echocardiogram noted cardiac dextroposition, a hypoplastic right lung, and possible right lower pulmonary vein drainage to the inferior vena cava. Follow-up fetal MRI was performed at 30 weeks’ gestation.
IMAGING FINDINGS
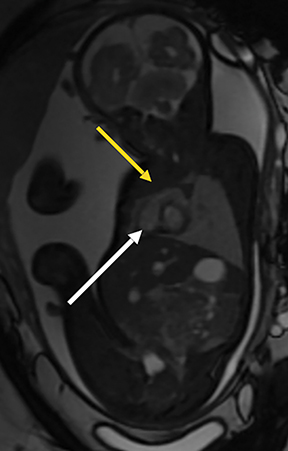
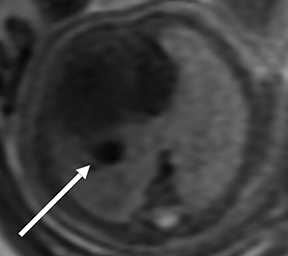
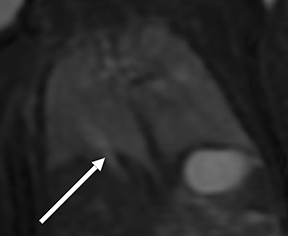
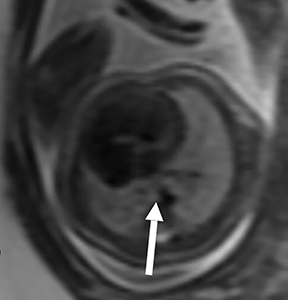
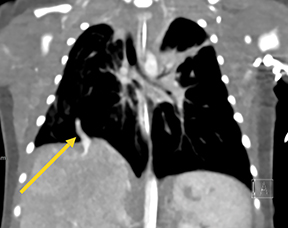
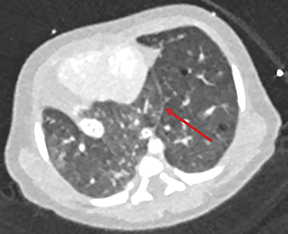
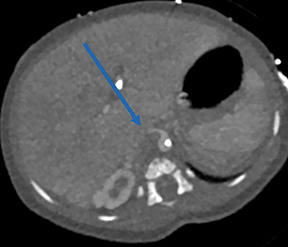
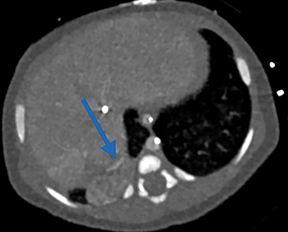
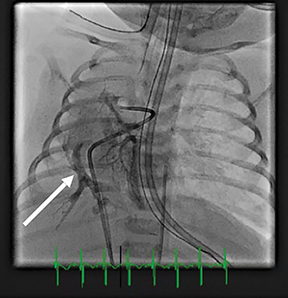
Fetal MRI at 30 weeks’ gestation demonstrated dextroposition of the heart and right lung hypoplasia (Figure 1). There was an abnormally large vessel in the right lower thorax (Figure 2) draining into the inferior vena cava, consistent with a scimitar vein. The right pulmonary artery was hypoplastic (Figure 3) compared to the contralateral side. Additionally, the images revealed lung parenchyma crossing the midline and in communication posterior to the pericardium, consistent with horseshoe lung (Figure 4). A right lower lobe lesion was noted, with an abnormal arterial branch originating off the aorta, and supplying the lesion, diagnostic for pulmonary sequestration (Figure 5).
Postnatally, a chest CT angiogram performed at 3 days of age (Figure 6) was consistent with the fetal MRI findings confirming a) right lung hypoplasia; b) the scimitar vein; c) the horseshoe lung; and d) pulmonary sequestration, with aberrant arterial supply from the aorta to the sequestration. Cardiac catheterization at 12 days of age (Figure 7) showed dual drainage of multiple segments of the right lung both anomalously via the scimitar vein and directly to the left atrium.
DIAGNOSIS
Scimitar syndrome
DISCUSSION
Scimitar syndrome, also referred to as hypogenetic lung syndrome, is a constellation of congenital anomalies that include partial anomalous pulmonary venous return to the inferior vena cava either above or below the diaphragm. This is most commonly accompanied by various degrees of right lung and right pulmonary artery hypoplasia.1 Without the abnormal pulmonary vein; ie, the scimitar vein, the pathology cannot be defined as Scimitar syndrome.2
The incidence of Scimitar syndrome ranges from 1 to 3 per 100,000 live births and a 2:1 female predominance.2 The clinical features of scimitar syndrome vary considerably. Patients are either diagnosed early (infantile type) or late (childhood/adult type).2,3 When they present during infancy, symptoms are usually severe and include failure to thrive, tachypnea, and heart failure. Cyanosis may occur if pulmonary hypertension is present, leading to right-to-left shunt. Symptoms in the childhood/adult type are milder and most commonly include recurrent pneumonia.2
Scimitar syndrome is associated with a number of cardiac and extra-cardiac anomalies. Extra-cardiac abnormalities include pulmonary and pulmonary artery hypoplasia, pulmonary sequestration, horseshoe lung, bronchiectasis, and diaphragmatic hernia.4 A horseshoe lung was present in our patient. This rare congenital pulmonary anomaly is characterized by fusion of the posterobasal portions of the right and left lungs across the midline, with the isthmus crossing behind the pericardium and anterior to the aorta. Approximately 80% of horseshoe lungs occur in association with scimitar syndrome.5
Fetal ultrasound may be the initial modality used to diagnose scimitar syndrome. The condition must be considered when fetal ultrasound reveals right lung hypoplasia and mediastinal shift, with characteristic anomalous drainage of any pulmonary vein. The diagnosis can be confirmed postnatally by radiography, angiography, or transthoracic or transesophageal echocardiography, CT angiography (CTA), or magnetic resonance angiography (MRA).6 The most evident postnatal sign on radiography is mediastinal shift. While each modality can show the scimitar vein (an anomalous pulmonary vein appearing as a curvilinear density in the right lower lobe and directed toward the right hemidiaphragm), CTA or MRA is typically used for diagnosis to show the venous connection with the inferior vena cava and to identify associated abnormalities.6 In our case, fetal MRI accurately confirmed the diagnosis and detailed the associated findings; to our knowledge, this has not been previously described.
CONCLUSION
Scimitar syndrome is a rare congenital syndrome with multiple associated findings and a wide variety of presentations. Our case demonstrates that fetal MRI can be successfully utilized to confirm a diagnosis of Scimitar syndrome and to identify associated anomalies. Early diagnosis is important in directing management, particularly in infants with severe symptomatology.
REFERENCES
- Konen, E, Raviv-Zilka, L., Cohen, R., et al. Congenital Pulmonary Venolobar Syndrome: Spectrum of Helical CT Findings with Emphasis on Computerized Reformatting. RadioGraphics. 2003; 23(5): 1175-1184.
- Cicek, S, Arslan, AH, Ugurlucan, M, et al. Scimitar Syndrome: The Curved Turkish Sabre. Seminars in Thoracic and Cardiovascular Surgery: Pediatric Cardiac Surgery Annual. 2014; 7(1): 56-61.
- Huddleston, C, Exil, V, Canter, C, et al. Scimitar syndrome presenting in infancy. Ann Thorac Surg. 1999; 67(1): 154-159.
- Di Filippo, S. Epidemiology and Physiopathology of Scimitar Syndrome. In: The Complete Reference for Scimitar Syndrome. Anatomy, Epidemiology, Diagnosis and Treatment. 2017; 57-66.
- Hussain, FB, Saadi, AA. Horseshoe Lung. Int J Ped Adolesc Med. 2014; 1(2): 102-103.
- Cruz-Martinez, R, and Gratacos, E. Scimitar Syndrome. In: Obstetric Imaging: Fetal Diagnosis and Care (2nd Ed). 2018: 22-25.
Prepared by Dr. Gustainyte while at the Department of Diagnostic Radiology, the University of South Florida, St. Petersburg, FL; Dr. Miller and Dr. Kucera while at Johns Hopkins University All Children’s Hospital, St. Petersburg, FL; Dr. Richard Towbin while a Radiologist at Phoenix Children’s Hospital, Phoenix, AZ; and Dr. Alexander Towbin while a Radiologist at Cincinnati Children’s Hospital, Cincinnati, OH.
