Lemmel’s syndrome

CASE SUMMARY
A 60-year-old woman who had undergone cholecystectomy 1 year previous presented with abdominal pain and jaundice. On physical examination, there was tenderness in the right hypochondrium. Her blood investigations revealed total bilirubin 2.12 mg/dl, direct bilirubin 1.2 mg/dl, aspartate amino transferase 78 IU/L, alanine aminotransferase 85 IU/L, alkaline phosphatase 305 IU/L with normal serum amylase and lipase.
IMAGING FINDINGS
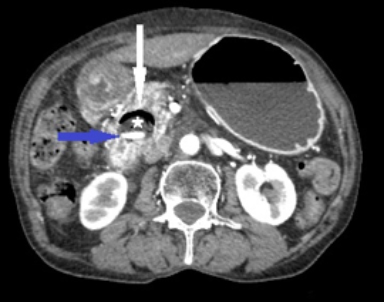
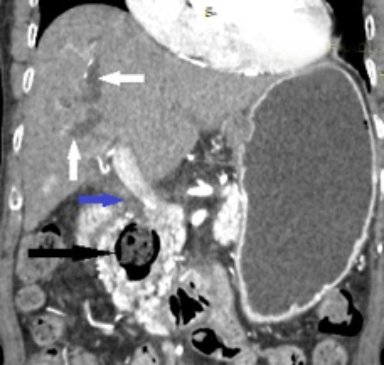
Ultrasound showed dilated central and peripheral biliary radicals with a dilated CBD, which measured 10.2mm in maximum caliber. The distal CBD couldn`t be assessed because of air shadows. No apparent cause was found on ultrasound. For further evaluation, a contrast-enhanced CT of the abdomen was performed. Axial and coronal CT images showed the diverticulum measuring 3.6 x 3.1 x 3.3c m (AP x Trans x CC) arising from the medial wall of the second part of the duodenum and lying in the pancreaticoduodenal groove. It was filled with air, fluid, and enterolith (Figure 1). Oral contrast was seen entering it in continuation with the duodenal lumen (Figure 2). The diverticulum was compressing the distal CBD, leading to proximal dilation of intra- and extrahepatic biliary radicals (Figure 3).
DIAGNOSIS
Lemmel’s syndrome. Differential diagnosis includes other causes of obstructive jaundice, such as choledocholithiasis, choledochal cyst, bile duct stricture, periampullary tumors, and pancreatic pseudocyst.
DISCUSSION
Lemmel’s syndrome is a pancreaticobiliary disease secondary to periampullary duodenal diverticulum compressing the distal common bile duct. Diverticula from the duodenum are common; the term “peri-ampullary diverticulum” is used for outpouching of duodenal mucosa that develops within 2 or 3 cm from the ampulla of Vater.1 Lemmel first described peri-ampullary diverticula compressing the distal common bile duct, leading to cholestatic jaundice, and called it Lemmel’s syndrome.2 They are classified into three types depending on the position of the papilla in relation to the diverticulum. In type I, the most common, the major papilla is located within the diverticulum. In type II, the papilla is located in the margin of the diverticulum; and in type III, the papilla is located near the diverticulum.3 These are largely asymptomatic; fewer than 10% are symptomatic. They are complicated by perforation and diverticulitis, and sometimes they cause pancreaticobiliary disease.4-6
Pancreaticobiliary complications of juxta-ampullary duodenal diverticulum include chlolestatic jaundice, choledocholithiasis, cholecystisis, cholangitis, and pancreatitis.7-9 The diverticular pouch is seen in continuation with the duodenal lumen; it contains food particles, air, and fluid. The pouch acts as a nesting area for bacterial growth, predisposing the patient to diverticulitis, peri-ampullary inflammation, and sometimes pancreatitis.10
Cross-sectional imaging, such as CT and MRCP, is extremely helpful in demonstrating peri-ampullary duodenal diverticulum as outpouching from the medial aspect of the duodenum. Oral contrast with multiplanar CT may show contrast material entering the diverticulum to establish the diagnosis. ERCP is another alternative that can be therapeutic, as it can be used to perform sphrincterotomy drainage.4 Surgical excision of the diverticulum is another treatment option.11
CONCLUSION
Lemmel’s syndrome should be considered a rare cause of obstructive jaundice; it should be considered in the absence of choledocholithiasis and/or lesions in the head of the pancreas. Fluid-filled diverticulum can mimic cystic neoplasms of the pancreas and pancreatic pseudocyst. High index of suspicion, along with the use of multiplanar CT and MRCP, are diagnostic in most cases.
REFERENCES
- Lobo DN, Balfour TW, Iftikhar SY, Rowlands BJ. Periampullary diverticula and pancreaticobiliary disease. Br J Surg. 1999;86:588–597.
- Lemmel G. Die Klinische Bedeutung der Duodenal Divertikel. Arch Verdauungskrht. 1934;46: 59-70.
- Zoepf T, Zoepf DS, Arnold JC, Benz C, Riemann JF. The relationship between juxtapapillary duodenal diverticula and disorders of the biliopancreatic system: Analysis of 350 patients. Gastrointest Endosc. 2001; 54:56–61.
- Wu SD, Su Y, Fan Y, Zhang ZH, Wang HL, Kong J, Tian Y. Relationship between intraduodenal peri-ampullary diverticulum and biliary disease in 178 patients undergoing ERCP. Hepatobiliary Pancreat Dis Int. 2007; 6:299–302.
- Gudjonsson H, Gamelli RL, Kaye MD. Symptomatic biliary obstruction associated with juxtapapillary duodenal diverticulum. Dig Dis Sci. 1988;33:114–121.
- Egawa N, Anjiki H, Takuma K, Kamisawa T. Juxtapapillary duodenal diverticula and pancreatobiliary disease. Dig Surg. 2010;27:105–109.
- Castilho Netto JM. Speranzini MB. Ampullary duodenal diverticulum and cholangitis. Sao Paulo Med J. 2003; 121:173–175.
- Tan NC, Ibrahim S, Chen CM, Tay KH. Periampullary diverticulum causing biliary stricture and obstruction. Singapore Med J. 2005; 46:250–251.
- Vitturi N, Simoni F, De Stefano F, Orlando R, Lirussi F, Realdi G. Paravaterian diverticula presenting as acute cholangitis in two very elderly patients. J Gastrointest. 2010;19:220–221.
- San Román AL. Moreira VF. García M. Merono E. Boixeda D.Direct compression by a duodenal diverticulum causing common bile duct obstruction. Endoscopy. 1994;26:334.
- Yoneyama F, Miyata K, Ohta H, Takeuchi E, Yamada T, Kobayashi Y. Excision of a juxtapapillary duodenal diverticulum causing biliary obstruction: report of three cases. J Hepatobiliary Pancreat Surg. 2004;11:69-72.
Prepared by Nishant Nayyar while a Junior Resident, Shikha Sood while an Assistant Professor, and Ashwani Tomar, while a Professor, in the Department of Radiodiagnosis, Indira Gandhi Medical College, Shimla, India.
