Creutzfeldt-Jakob disease: Two cases
CASE SUMMARY
Case No. 1: A 65-year-old male patient was presented to our neurology clinic with unwilled movement of the upper and lower extremities, disordered speech, walking instability, and amaurosis, the inability to count his fingers. The patient reported visual impairment started gradually two years previous. Anti-parkinsonism treatment prescribed by a local neurologist did not cause any clinical improvement, despite being used as directed.
Case No. 2: A 67-year-old female presented to the neurology clinic with unwilled movement of the upper and lower extremities, disordered speech, walking instability, and amaurosis.
IMAGING FINDINGS
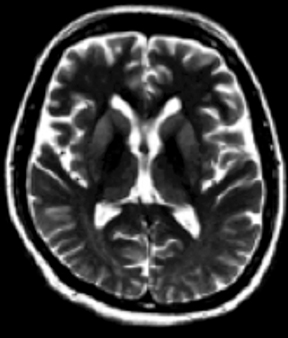
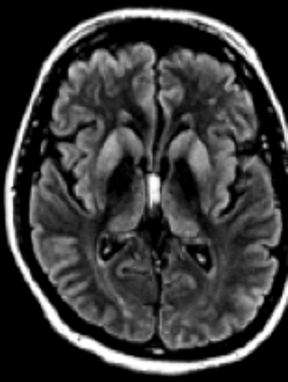
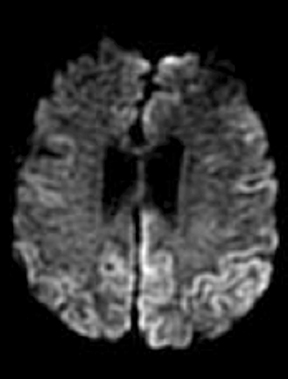
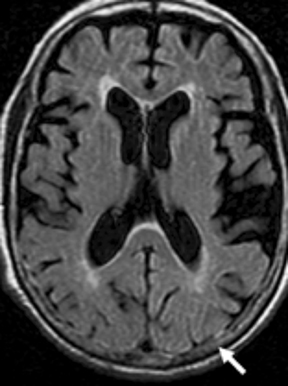
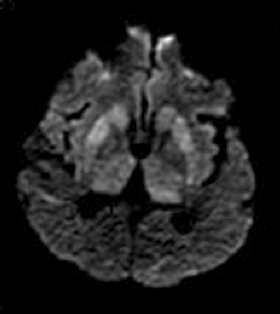
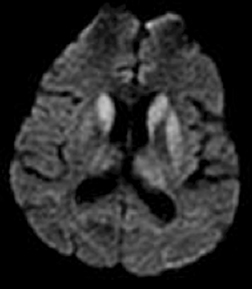
In the first case, X-rays of the chest and CT of the brain (contrast and noncontrast-enhanced) did not show any pathologic findings of brain parenchyma and lungs. An electronencephalogram registered slow dysrhythmia, accompanied by irritative specific activity and multifocal changes. A repeat EEG seven days later revealed similar changes. An MRI brain scan revealed high signal intensity on T2-weighted imaging and fluid attenuated inversion recovery (FLAIR) sequences in the caudate and putamen bilaterally. Diffusion-weighted images showed bilateral symmetric hyperintense signals in gyriform cortical, lesions spreading in both cerebral hemispheres that were more pronounced in FLAIR and DWI sequences (Figure 1). The results were highly suggestive of Creutzfeldt-Jakob disease.
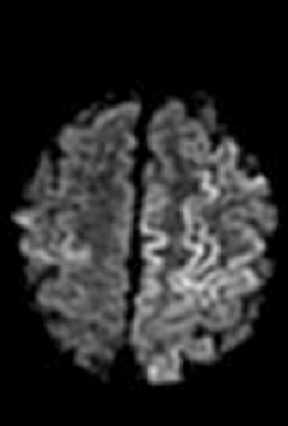
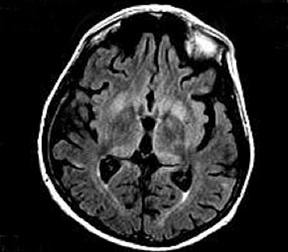
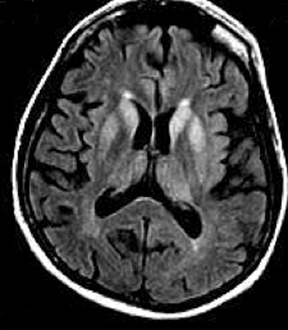
In the second case, X-rays of the thorax and CT scans of the brain (plain and contrast) did not show pathologic findings. An EEG registered slow, irregular activity from 2.5 to 4.5 Hz that represented generalized bi- and triphase complex joined by slow pseudoperiodic waves/picks. LTSH, pathogenic protein marker 14-3-3, was isolated. Brain MRI revealed high signal intensity on T2-weighted imaging and fluid attenuated inversion recovery (FLAIR) sequences in the caudate and putamen bilaterally (Figure 2). Diffusion-weighted images showed bilateral symmetrical hyperintense signals in the caudate and putamen and hypointense signal on apparent diffusion co-efficient (ADC) maps in the corresponding areas, suggestive of restricted diffusion. The lesions were characteristic for Creutzfeldt-Jakob disease.
DIAGNOSIS
Creutzfeldt-Jakob disease
DISCUSSION
Creutzfeldt-Jakob disease (CJD) is a rare entity and cerebral imaging is considered to be of little value for definite ante-mortem diagnosis and is usually undertaken to exclude other illnesses.1 However, recent studies have shown that MRI is a valuable diagnostic tool with a reasonable sensitivity of 61-90% and a high specificity of 94% for CJD.2 MRI also helps in differentiating sporadic CJD from variant CJD.1 In sporadic CJD, the T2 prolongation and reduced diffusion are noted mostly in the corpus striatum, followed by the neocortex and posterior and medial thalami. But in variant CJD, abnormalities are most frequent in the posterior (pulvinar) and medial thalami followed by the periaqueductal gray matter and striatum, and less commonly in the neocortex.3 The other notable MRI finding in variant CJD is periaqueductal gray matter high signal without any cerebral atrophy.1 Sporadic CJD usually appears at 50 to 70 years of age, comprising 90% of all cases. The diagnosis of sporadic CJD is based on clinical symptoms along with imaging, pathology, and laboratory tests including EEG, and CSF and serum analysis for specific proteins, such as the S-100 protein, Tau protein, 14-3-3 protein.4 Behavioral and visual disturbances, progressive dementia, myoclonus, and cerebellar, akinetic mutism, pyramidal, and extrapyramidal symptoms are among the clinical findings, while one-third of patients present with fatigue, sleep disturbances, and decreased appetite. Dementia, ataxia, and myoclonus are considered the CJD triad. Ataxia is a late-stage symptom and myoclonus has been suggested as a reaction to auditory and tactile stimuli.5 On T2W MRI, hyperintense areas can be found in the caudate nucleus, putamen, globus pallidus, and thalamus. Diffusion-weighted MRI may indicate bilateral symmetrical hyperintense signals in the basal ganglia and/or cortex cerebri. Diffusion-weighted MRI has been considered a proper modality for CJD diagnosis in early disease.6
Shiga et al6 noted that the diffusion-weighted MRI had higher sensitivity for CJD (92%) compared to FLAIR sequences (41-59%), T2W (36-50%), EEG (50-78%), CSF protein 14-3-3 (84%) or neuron-specific enolase (73%). Diffusion weighted MRI is more tolerant with respect to motion artifacts than T2W and FLAIR images; abnormalities can be detected as early as three weeks after symptom appearance, even before the appearance of periodic triphasic waves on EEG.6 The combination of FLAIR and DWI has a sensitivity, specificity, and accuracy of over 90% in differentiating CJD from other dementias.7 The multifocal cortical and subcortical hyperintensities confined to gray matter in DWI may be more useful than the CSF protein 14-3-3.8
CJD symptoms can be similar to those of viral encephalitis, Hashimoto encephalitis, and amyotrophic lateral sclerosis. Therefore, they must be considered along with other clinical and para-clinical findings for CJD diagnosis. EEG is a diagnostic modality with sensitivity near 64% and specificity between 74 and 91%.5 In our cases, EEG showed typical changes for CJD. Gozke et al reported the case of a 70-year-old man with behavioral changes, insomnia, irritability, and weakness. EEG findings were nonspecific, while diffusion-weighted MRI showed hyperintense signal changes in the cortex.5,9 We were able to confirm that DWI has a higher conspicuity for the detection of cortical changes compared with FLAIR.6,7,10,11 Our cases showed typical EEG and MRI signs and positive 14-3-3 protein results, which are important clues for CJD diagnosis.
CONCLUSION
Patients who have progressive dementia should be evaluated with MRI and CSF analysis for CJD-specific proteins should be considered. Diffusion-weighted imaging can detect characteristic lesions in most patients with CJD regardless of the presence of PSWCs. DWI is the most sensitive test for early clinical diagnosis of CJD; consideration should be given to its inclusion in the clinical diagnostic criteria of CJD.
REFERENCES
- Schröter A, Zerr I, Henkel K, Tschampa HJ, Finkenstaedt, M, and Poser S. Magnetic resonance imaging in the clinical diagnosis of Creutzfeldt-Jakob disease. Arch. Neurol. 2000; 57(12):1751–1757.
- Zeidler M, et al. The pulvinar sign on magnetic resonance imaging in variant Creutzfeldt-Jakob disease. Lancet. 2000; 355(9213): 1412–1418, Apr. 2000.
- Krasnianski A, et al. Clinical findings and diagnostic tests in the MV2 subtype of sporadic CJD. Brain. 2006;129: 2288–2296.
- Masters, CL, Harris, JO, Gajdusek, DC, Gibbs, CJ, Bernoulli, C, and Asher, DM. Creutzfeldt- Jakob disease: Patterns of worldwide occurrence and the significance of familial and sporadic clustering. Ann. Neurol. 1979; 5(2):177–188.
- Gozke E, Erda N. Creutzfeldt-Jacob Disease: a case report. Cases J.. 2008; 146.
- Shiga Y, et al. Diffusion-weighted MRI abnormalities as an early diagnostic marker for Creutzfeldt-Jakob disease. Neurology..2004; 63(3): 443–449.
- Young GS, et al.Diffusion-weighted and fluid-attenuated inversion recovery imaging in Creutzfeldt-Jakob disease: High sensitivity and specificity for diagnosis. AJNR. Am. J. Neuroradiol. 2005; 26(6): 1551–1562.
- Mendez OE, Shang J, Jungreis CA, and Kaufer, DI. Diffusion-weighted MRI in Creutzfeldt-Jakob disease: A better diagnostic marker than CSF protein 14-3-3? J. Neuroimaging. 2003; 13(2):147–151.
- Praveen KS, Sinha S, Chandrasekhar HS, Vijayan J, and Taly AB. Sporadic onset Creutzfeldt-Jacob disease: Interesting MRI observations. Neurol. India. 2006; 54(4): 418–420.
- Bahn MM and Parchi P. Abnormal diffusion-weighted magnetic resonance images in Creutzfeldt-Jakob disease. Arch. Neurol. 1999; 56(5): 577–583.
- Matoba M, Tonami H., Miyaji H, Yokota H, and Yamamoto I. Creutzfeldt-Jakob disease: serial changes on diffusion-weighted MRI. J. Comput. Assist. Tomogr. 2001; 25(2): 274–277.
Prepared by Dr. Shatri while an Assistant Professor and Radiologist at the Clinic of Radiology, University Clinical Centre of Kosovo, Prishtina, Kosovo; and Dr. Kabashi while a Radiologist at the Clinic of Radiology, University Clinical Centre of Kosovo, Prishtina, Kosovo.
