Osteochondroma of the right mandible
By Novick D, Semenoff A, Collins K, Victor N, Lev S, Shah S


CASE SUMMARY
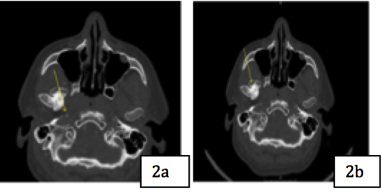
A 39-year-old male with history of dyslipidemia presented to the clinic complaining of progressively worsening right jaw pain, clicking, and “jaw shifting.” The patient stated that the pain had begun in 2003, but had progressively worsened over the years and was now accompanied by headaches and the inability to close his jaw on the right side. He had no allergies and was not taking any medications. His social history was non-contributory. There was no reported trauma or recent travel. Vital signs were within normal limits. Upon physical examination, the patient had a large growth of his right mandibular condyle with severe leftward deviation of the mandible, resulting in malocclusion (Figure 1).
IMAGING FINDINGS
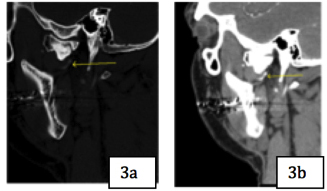
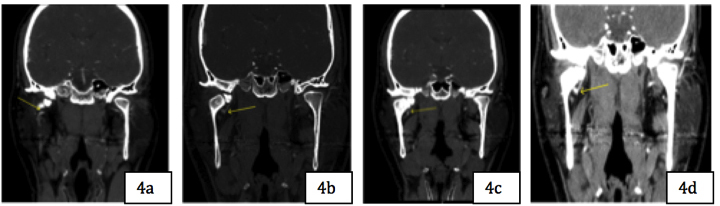
A computed topography angiogram (CTA) of the head and neck with and without contrast and a maxillofacial CT without contrast were obtained (Figures 2-4). These revealed a well-corticated, expansile, and irregular osseous productive lesion at the right mandibular condyle compatible with, but not specific for, a benign appearing neoplasm. Of particular importance was the proximity of the lesion to the right internal maxillary artery and its numerous branches.
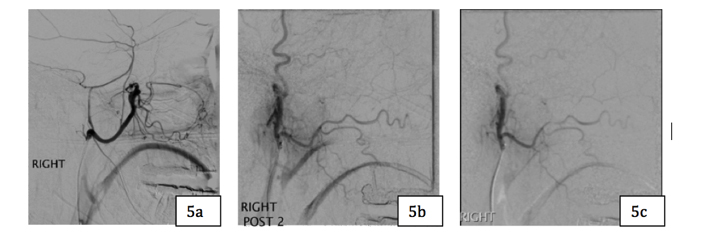
The patient underwent a combined diagnostic angiogram and transcatheter embolization prior to the planned surgical intervention and removal of the mass. Angiography demonstrated that the right internal carotid artery as well as the right external carotid artery and its numerous branches were patent, with no evidence of internal to external anastomosis. Furthermore, no retinal blush was seen, permitting us to proceed (Figure 5). A 2.8 French 150cm microcatheter was advanced over the wire through the 5- French Headhunter. After engaging the right internal maxillary artery, the 00.018 GT glidewire was removed and macerated pledgets of Gel-Foam were given through the microcatheter at the ostium until the artery was occluded (Figure 5). Post Gel-Foam embolization DSA of the right internal maxillary artery demonstrated complete occlusion of the artery. (Figure 5).
The patient tolerated the procedure without complication and was transferred to the post-anesthesia care unit (PACU) in stable condition and then to the surgical intensive care unit (SICU) for further monitoring.
The patient remained in the SICU for one day, and was cleared for next day resection of the osseous lesion by the OMFS surgeons. As planned, the patient underwent right odontogenic TMJ reconstruction with an alloplastic joint replacement, left sagittal split osteotomy of the mandible, and Lefort I osteotomy of the maxilla with abdominal fat harvest (Figure 5). The bony mass was completely removed and the specimen was sent to pathology for histopathological characterization.
DIAGNOSIS
Osteochondroma of the right mandible. Differential includes chondrosarcoma, endrosarcoma, and chondromyxoid fibroma.
DISCUSSION
Osteochondromas are the most common primary benign bone tumor, accounting for 20%-50% of all benign bone tumors and 10-15% of all bone tumors. They are an outgrowth of existing bone near a growth plate and are composed of underlying cortical and medullary bone, covered by a hyaline cartilaginous cap.1 Any bone that develops by endochondral ossification has potential for malignant transformation. Transformation to osteochondroma most commonly, occurs in children and young adults, predominantly in long bones of the limbs. Osteochondromas are typically asymptomatic and do not require surgical resection. However, when occurring on the jaw, their enlargement and exophytic growth can lead to significant facial deformities, as well as masticatory and occlusive symptoms and pain.2
Several surgical approaches may be considered. One of the most common surgical options is a Lefort I osteotomy.3 Although complications are considered very rare, vascular compromise can be especially devastating.3-6 Embolization has been shown to be a safe and effective treatment option for bleeding and vascular injuries, as well as postoperative AVMs and pseudoaneurysms.3-7 It has been amply demonstrated that the role of embolization has expanded well beyond treatment of intraoperative complications to include the management of refractory epistaxis, preoperative prophylaxis of vascular tumors, and as an adjunct in skull base surgery.8
Postoperative complications are well documented and the role of preoperative embolization is strongly recommended in maxillofacial and odontogenic surgeries. Potentially important intraoperative complications leading to severe blood loss and the need for transfusion, whether secondary to vascular injury or prolonged surgeries, are well documented, especially in prolonged surgeries.9,10 Furthermore, reports of odontogenic procedures requiring higher rates of transfusion is higher than those reported for similar procedures.10
In a retrospective study of a single institution looking at four different types of odontogenic surgeries, several variables were assessed for predictors to blood loss, including age, gender, BMI, surgery time, as well as pre- and postoperative HGB and HCT. The mean operative time was 5hrs 32 min. The only clinically significant predictor of intraoperative blood loss was intraoperative time.2 In our case, the OMF surgeons reported excellent hemostatic control throughout the operation, no intraoperative complications, and successful postoperative hemostasis. Preoperative embolization in odontogenic dentofacial corrective surgeries should be considered especially for lengthy procedures with the potential for blood loss.
CONCLUSION
The use of preoperative embolization not only has an important and expanding role as a valuable adjunct in preparing for vascular trauma and neoplasms, as well as skull-based procedures.8 Preoperative embolization in lengthy dentofacial corrective surgeries is rapidly becoming recognized for the integral role it plays in minimizing blood loss.
REFERENCES
- Murphy MD, Choi JJ, Kransdorf MJ, Flemming DJ, Gannon, FH. Imaging of Osteochondroma: Variants and Complications with Radiologic-Pathologic Correlation. AFIP Archives. 2000; 1407-1433.
- Kwon YE, Choi KS, An CH, Choi SY, Lee JS, An SY. Recurrent Osteochondroma of Mandibular Condyle: A Case Report. Imaging Sci Dent. 2017 Mar; 47(1): 57-62.
- Embolization of pseuoanurysm of the internal maxillary artery after orthognathic surgery. https://www.ncbi.nlm.nih.gov/pubmed/21119417
- Pseudoaneurysm of the Facial Artery occurred after the Mandibular Sagittal Split Ramous Osteotomy https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3661081/
- Avelar RL, Goelzer JG, Becker OE, de Oliveira RB, Raupp EF, de Magalhãe PS, et al. Embolization of pseudoaneurysm of the internal maxillary artery after orthognathic surgery. J Craniofac Surg. 2010;21:1764–1768. doi: 10.1097/SCS.0b013e3181f40393.
- Chepla KJ, Totonchi A, Hsu DP, Gosain AK. Maxillary artery pseudoaneurysm after Le Fort I osteotomy: treatment using transcatheter arterial embolization. J Craniofac Surg. 2010; 21:1079–1081. doi: 10.1097/SCS.0b013e3181e20693.
- H.-W. Jo, Y.-S. Kim, D.-H. Kang, S.-H. Lee, and T.-G. Kwon, Pseudoaneurysm of the facial artery occurred after mandibular sagittal split ramus osteotomy. Oral Maxillofac Surg. 2013 Jun; 17(2): 151–154. doi: 10.1007/s10006-012-0339-4
- Risley J1, Mann K, Jones NS. The role of embolisation in ENT: An update. J Laryngol Otol. 2012 Mar;126(3):228-35. doi: 10.1017/S00222 15111003148
- Faverani LP1, Ramalho-Ferreira G, Fabris AL, Polo TO, Poli GH, Pastori CM, Marzola C, Assunção WG, Garcia-Júnior IR. Intraoperative blood loss and blood transfusion requirements in patients undergoing orthognathic surgery. Oral Maxillofac Surg. 2014 Sep;18(3):305-10. doi: 10.1007/s10006-013-0415-4.
- Maisa O Al-Sebaei. Predictors of intre-operative blood loss and blood transfusion in orthognathic surgery: a retrospective cohort study in 92 patients. Patients Safety in Surgery. doi.org/10.1186/s13037-014-0041-6
Prepared by Dr. Novick while a resident, PGY-4, Department of Radiology; Dr. Semenoff while chief resident, PGY-4, Department of Oral and Maxillofacial Surgery; Dr. Victor while with the Department of Oral and Maxillofacial Surgery; Dr. Lev while Chief of the Department of Neuroradiology; and Dr. Shah while Chief of the Department of Interventional Radiology, Nassau University Medical Center, East Meadow, NY; and Ms. Collins, while an MS-3 Student at the New York Institute of Technology, College of Osteopathic Medicine, Old Westbury, NY.
