Extranodal Rosai-Dorfman disease of the kidney
By Tesfay A, Bashiti R, Greenlee J, Lincoln D, Hurley P, Govil H



CASE SUMMARY
A 28-year-old female with no significant medical history presented with abdominal pain, nausea, and vomiting, along with left-sided abdominal mass of approximately 6 months’ duration with progressive enlargement. The patient denied any loss of appetite, weight loss, cough, chest pain, shortness of breath, or urinary or bowel symptoms. Physical exam revealed a firm, palpable mass in the left hemi-abdomen. No direct or rebound tenderness was appreciated. Laboratory evaluation showed mild iron deficiency anemia.
IMAGING FINDINGS
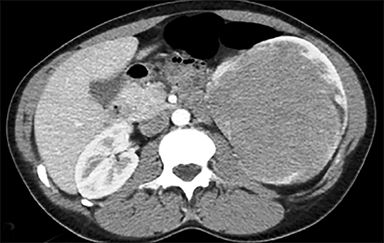
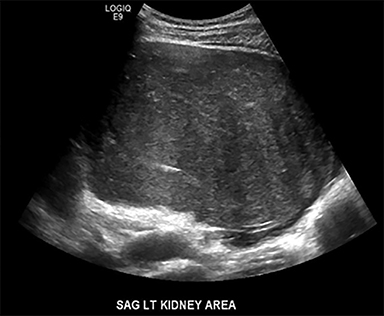
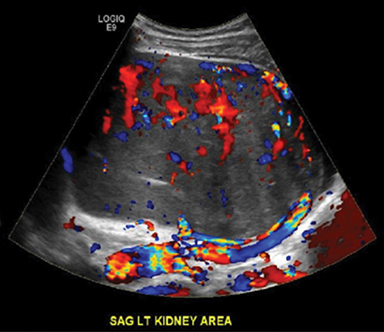
A CT scan of the abdomen demonstrated a 9.3 × 8.2 × 17.5 cm heterogeneously enhancing left renal mass, with significant mass effect and displacement of adjacent structures. The left renal vein and inferior vena cava were patent without evidence of intraluminal filling defect or tumor thrombus. Left para-aortic lymphadenopathy was also noted, with the largest lymph node measuring 2.2 × 1.8 cm (Figure 1). Retroperitoneal ultrasound showed a large heterogeneous solid mass with increased color Doppler flow. There was calyceal dilation noted with a rind of renal cortical tissue along the superior aspect of the mass (Figure 2). A CT-guided biopsy of the renal mass lesion was subsequently performed by interventional radiology.
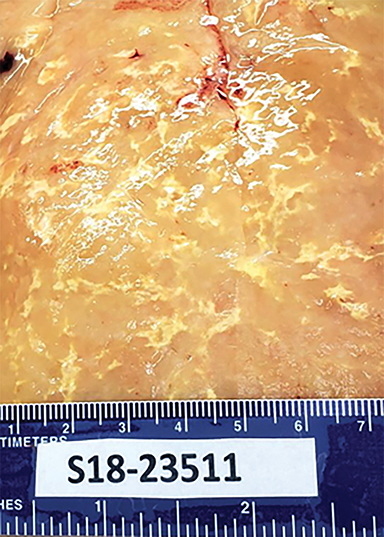
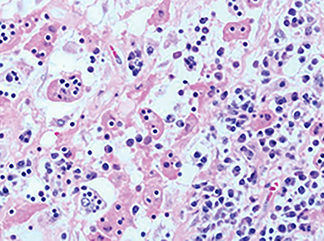
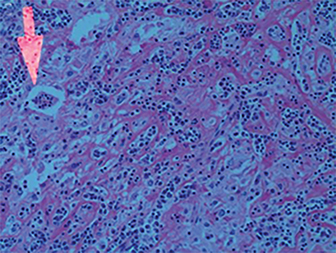
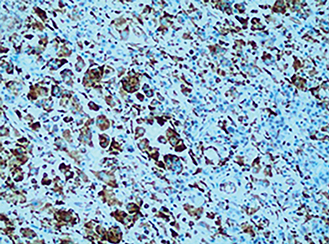
Pathology sections from the left kidney demonstrated a lesion composed predominantly of histiocytes with admixed plasma cells and lymphocytes and focal evidence of emperipolesis. Immuno-stains showed histiocytes to be CD68 positive and negative for CD1A. S-100 showed diffuse positivity in the histiocytes. Cytokeratin was negative and PAX-8 highlighted background lymphocytes. The presence of emperipolesis and S-100 immunostaining are most consistent with extranodal Rosai-Dorfman disease (Figure 3).
Patient was referred to to surgery for left radical nephrectomy via a sub-costal incision. Intra-operative findings demonstrated a bulky renal mass, which was removed en bloc.
DIAGNOSIS
Extranodal Rosai-Dorfman disease
DISCUSSION
Rosai-Dorfman disease (RDD), also referred to as sinus histiocytosis with massive lymphadenopathy (SHML), is a rare, benign proliferative histiocytic disorder first described in 1969 by Rosai and Dorfman.1,2 The most common presentation of Rosai-Dorfman disease is painless lymphadenopathy; most commonly bilateral cervical with constitutional symptoms. In about 43% of patients the disease may also arise in extranodal sites and almost any organ can be involved.3
The imaging findings of RDD are very nonspecific, with a wide differential diagnosis which includes benign and malignant neoplasm, infection and other mass lesion etiologies. As such, diagnosis depends on tissue sampling and pathology demonstrating diffuse histiocytosis with presence of emperipolesis and S-100 immunostaining.4
Genitourinary, specifically renal involvement has been rarely described. A case of an adult female with a retroperitoneal pelvic mass causing urinary obstruction was described by Leiva, et al.5
Manifestations of extranodal RDD have been treated with surgical resection, medical/chemotherapy and radiation therapy; however surgical therapy has been the most successful and definitive treatment.5,6 The most commonly reported sites of extranodal involvement are the skin and soft tissue; this usually presents as well-defined papules to palpable masses, with or without satellite lesions.7
Our patient presented with a slowly growing left sided abdominal mass over a period of 6 months. Emergency presentation was precipitated by sudden pain over the left side of the abdomen. During initial clinical evaluation, there were no systemic constitutional symptoms described or lymphadenopathy other than a palpable left sided abdominal mass. A CT scan of the abdomen did demonstrate a large left renal mass and multiple enlarged para-aortic lymph nodes measuring up to 1.8 cm in short axis.
Our case demonstrated classic histological features suggestive of RDD, which included emperipolesis (presence of an intact cell within the cytoplasm of another cell) and diffuse positivity for S-100 immuno-stains. Surgical resection was chosen due to the size of the mass and associated symptomatic mass effect.
CONCLUSION
Extranodal Rosai-Dorfman syndrome accounts for almost half of all clinical presentations; however, renal involvement has been very rarely reported. We present a case of extranodal RDD as a renal mass in a young female patient, with imaging findings and pathologic-diagnosis correlation.
REFERENCE
- Rosai J, Dorfman RF. Sinus histiocytosis with massive lymphadenopathy. A newly recognized benign clinicopathological entity. Arch Pathol. 1969; 87:63-70.
- Rosai J, Dorfman RF. Sinus histiocytosis with massive lymphadenopathy: a pseudolymphomatous benign disorder. Analysis of 34 cases. Cancer. 1972; 30: 1174-1188.
- Calvo Corbella CL, Gil Sierra A, Gallego Gomez P; Móstoles ES. Radiologic Findings in Rosai-Dorfman Syndrome. European Society of Musculoskeletal Radiology: essr2013/P-0106.
- Mantilla JG, Goldberg-Stein S, Wang Y. Extranodal Rosai-Dorfman disease: Clinicopathologic series of 10 patients with radiologic correlation and review of the literature. Am J Clin Pathol. 2016; 145: 211-221.
- Leiva BJ, Bofill RM, Sevin BU, Geiger SJ. Extranodal Rosai-Dorfman disease as a pelvic mass. Int J Gynecol Cancer. 2006; 16:312-315.
- Adeyiga AO, Bandarkar AN. Extranodal Rosai-Dorfman Disease of the Pediatric Female External Genitalia: A Case Report. Int J Radiol Imaging Technol. 2016; 2: 018.
- Mantilla JG, Goldberg-Stein S, and Wan Y. Extranodal Rosai-Dorfman Disease Clinicopathologic Series of 10 Patients With Radiologic Correlation and Review of the Literature. Am J Clin Pathol. 2016; 145(2):211-221.
Prepared by Dr. Tesfay and Dr. Bashiti while at the Department of Diagnostic Radiology; Dr. Greenlee and Dr. Hurley while at the Department of Urology; and Dr. Lincoln while at the Department of Interventional Radiology; and Dr. Govil while at the Department of Pathology; Michigan State University-College of Human Medicine, Southeast Michigan Campus, Providence Hospital, Southfield, MI.
