Chemoembolization via intrahepatic collateral arteries
By Sze DY

Case Summary
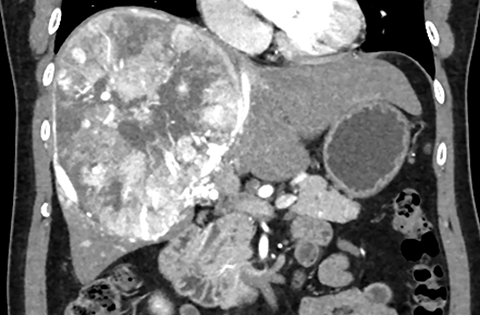
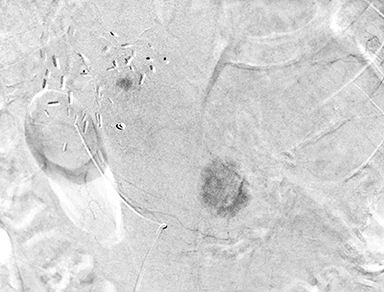
A 53-year-old man with chronic hepatitis B presented with elevated transaminases while taking herbal supplements, but was otherwise asymptomatic, Child-Pugh A5 and ECOG performance status 0. Workup included nonreactive hepatitis B surface antigen, negative hepatitis C antibody, negative colonoscopy except for small hemorrhoids, negative antinuclear antibody, negative alpha-1 antitrypsin and ceruloplasmin tests. He transferred his care to a second hospital and underwent hepatic ultrasonography, revealing a 16 cm mass, confirmed on multiphasic CT scan to be a hepatocellular carcinoma (Figure 1). He then transferred his care to a tertiary care hospital, where he underwent a trisegmentectomy.
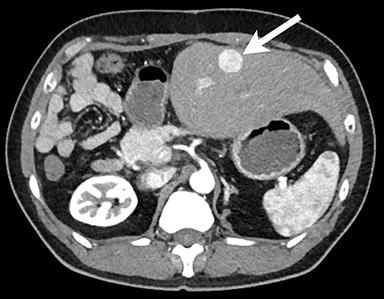
One year after “curative” resection, follow-up imaging revealed a hypervascular lesion in segment 3 measuring 2.1 cm, indicative of recurrence (Figure 2). A second possible lesion in the fissure of the ligamentum venosum was measured at 0.8 cm, and was felt to be inaccessible for ablation (Figure 2). The patient’s liver function remained Child-Pugh A5, but his performance status had deteriorated mildly to status 1 after surgery. He was referred for hepatic angiography and chemoembolization.
Imaging Findings
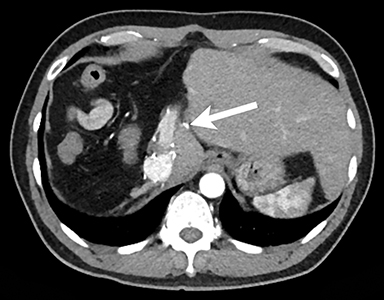
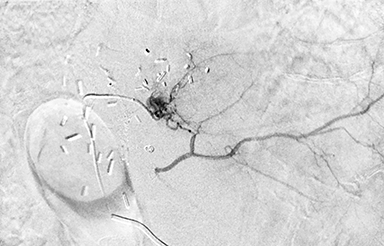
Initial hepatic angiography revealed postsurgical distortion of the arterial anatomy, with proximal occlusion of the segment 2 and segment 3 arteries with distal reconstitution from intrahepatic collateral vessels (Figure 3). Parenchymal phase imaging confirmed two hypervascular lesions (Figure 3).
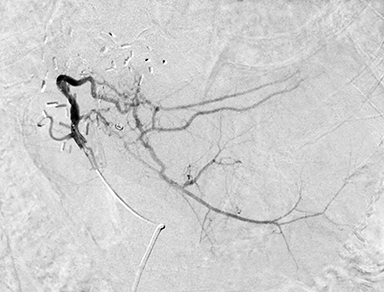
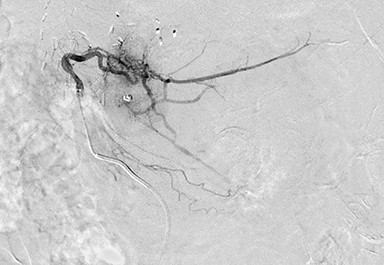
Although the collateral vessels appeared too small in diameter and too tortuous to accommodate standard microcatheters, treatment was attempted using a Fathom 0.014” guidewire (Boston Scientific, Marlborough, MA) and a 2.8-Fr SeQure® microcatheter (Guerbet, Roissy CdG, France). (At the time, smaller-diameter SeQure® microcatheters had not yet been released).
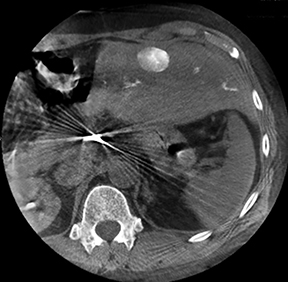
The submillimeter branch supplying the falciform cleft was successfully selected, and the lesion treated with doxorubicin-loaded LC beads 100-300 µm (BTG, London, England) until stasis of the tumor-feeding branch (Figure 4) was achieved. Likewise, the tortuous intrahepatic collateral vessel to segment 3 was selected and the segment 3 lesion was also treated with drug-eluting LC beads (Figure 4). Completion angiography confirmed disappearance of tumor blushes but maintenance of flow in nontarget vessels (Figure 5), and unenhanced cone-beam CT confirmed retention of contrast medium in the treated lesions (Figure 5).
Follow-up MR imaging at 3 months revealed complete response of the ligamentum venosum lesion and partial response of the segment 3 lesion. Residual disease was treated with percutaneous microwave ablation.
Discussion
Microcatheter design must balance the demands of: 1) adequate lumen to accommodate viscous or particle-containing injected fluids; 2) flexibility to navigate tortuosities without causing vessel injury; and 3) longitudinal stiffness to allow pushability. Additional features may include shaped tips, torqueability, and characteristics that help reduce reflux.
Conclusion
Selectivity of catheterization and treatment has substantial impact on outcomes of transarterial chemoembolization. Navigation of small, tortuous vessels is possible using the SeQure® microcatheter, even using the large 2.8-Fr version. Although this case cannot demonstrate the reflux reduction features of the of the SeQure® microcatheter, it demonstrates the flexibility and pushability that allowed selection of small, tortuous vessels. Future studies using radiopaque microspheres may be performed to test the controlled reflux feature.
Suggested Reading
- Miyayama S, Mitsui T, Zen Y, Sudo Y, Yamashiro M, Okuda M, Yoshie Y, Sanada T, Notsumata K, Tanaka N, Matsui O. Histopathological findings after ultraselective transcatheter arterial chemoembolization for hepatocellular carcinoma. Hepatol Res. 2009; 39:374-81.
- Mokin M, Waqas M, Setlur Nagesh SV, Karkhanis NV, Levy EI, Ionita CN, Siddiqui AH. Assessment of distal access catheter performance during neuroendovascular procedures: measuring force in three-dimensional patient specific phantoms. J Neurointerv Surg. 2019; 11:619-622.
- Ogata N, Goto K, Uda K. An evaluation of the Physical Properties of Current Microcatheters and Guidewires. The Development of the “Catheter-glide Approach” in Response to Weaknesses of Current Materials. Interv Neuroradiol. 1997; 3:65-80.
- Zoarski GH, Mathis JM, Hebel JR. Performance characteristics of microcatheter systems in a standardized tortuous pathway. AJNR Am J Neuroradiol. 1998; 19:1571-6.
Dr. Sze is Professor of Vascular and Interventional Radiology, Stanford University, Stanford, CA.
