Bartholin’s gland carcinoma





Prepared by Amy Liebeskind, MD and Stephen Machnicki, MD, Department of Radiology, and Dorothy Blackmun, MD, Department of Pathology, Lenox Hill Hospital, New York, NY.
CASE SUMMARY
A 53-year-old woman with no significant medical history presented to her gynecologist with vulvar pruritis. Physical examination revealed a firm mass in the region of the left Bartholin's gland, which was thought to be a Bartholin's gland cyst. The patient was taken to the operating room for a planned marsupialization procedure.
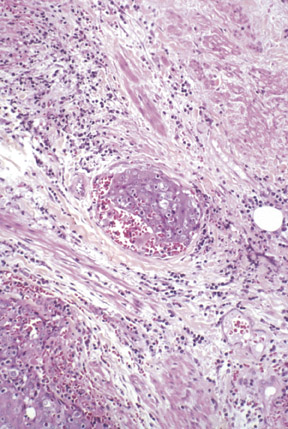
Upon incision of the left vaginal mucosa and exposure of the Bartholin's gland, the gland was found to be solid and enlarged. A tissue specimen was obtained and was sent for pathologic evaluation. Microscopic examination revealed near complete replacement of the Bartholin's gland by invasive poorly differentiated keratinizing squamous cell carcinoma that appeared to arise from the duct of the Bartholin's gland, given the presence of scattered benign-appearing residual vestibular glands (Figure 1A). Extensive necrosis was present, as well as diffuse involvement of soft tissue and skeletal muscle. Vascular (Figure 1B) and perineural invasion were also identified. The margins of the specimen were positive for tumor involvement.
DIAGNOSIS
Bartholin's gland carcinoma
IMAGING FINDINGS
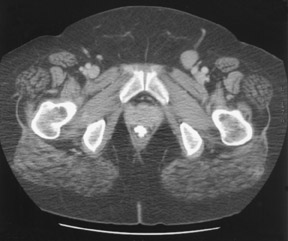
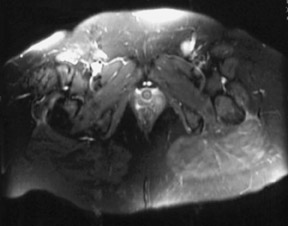
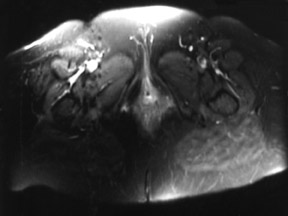
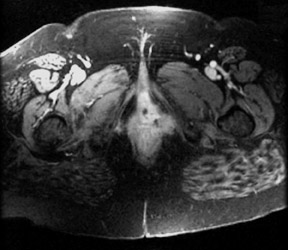
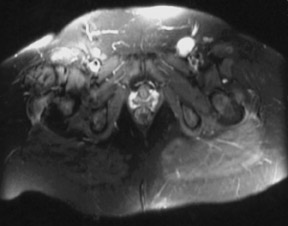
The patient was sent for diagnostic imaging evaluation for tumor staging. Following the receipt of the results of the pathologic examination, a computed tomography (CT) scan of the pelvis was performed that revealed a 2.5 × 2.0 cm left femoral lymph node (Figure 2). No vulvar or other pelvic abnormalities were identified. Magnetic resonance imaging (MRI) of the pelvis was performed on the following day with a 1.5T GE Signa scanner (GE Medical Systems, Waukesha, WI). Axial and sagittal T1-weighted images (repetition time [TR]: 17.6, echo time [TE]: 3), axial, sagittal, and coronal T2-weighted images (axial with fat saturation--TR: 3616, TE: 105; sagittal and coronal--TR: 5450, TE: 45) and postgadolinium axial T1-weighted images with fat saturation (TR: 17.6, TE: 3) of the pelvis were obtained. MR imaging revealed a >3.8 × 1.5 cm mass in the left perineum. The mass was isointense to skeletal muscle on T1-weighted images, mildly hyperintense to skeletal muscle on fat-saturated T2-weighted images (Figure 3), and exhibited enhance-ment following administration of gadolinium (Figure 4). The mass was contiguous with the left posteriolateral aspect of the urethra and the left lateral aspect of the vagina, and extended laterally through the levator ani muscles and into the left ischiorectal fossa. Bilateral lymphadenopathy in the groin was identified, including a 2.5 × 2.0 cm lymph node adjacent to the left femoral vessels that was hyperintense on T2-weighted images (Figure 5), and demonstrated enhancement on postgadolinium images, and a 1.0 cm left superficial inguinal lymph node. Several superficial inguinal lymph nodes in the right groin measuring up to 1.0 cm were also identified.
Subsequently, a CT-guided biopsy of the left femoral lymph node was performed, which revealed metastatic keratinizing squamous cell carcinoma.
DISCUSSION
Since its initial description in 1864 by Klob, fewer than 350 cases of Bartholin's gland carcinoma have been reported. 1 Conclusions regarding the diagnosis and treatment of Bartholin's gland carcinoma are limited due to the relatively small number of patients in any single series; the largest published single-institution series to date included 36 patients. 2 The median age at presentation for patients with Bartholin's gland carcinoma is 50 years. 3 Patients typically present with a painless vulvar mass, 2-4 which frequently leads to a delay in obtaining the correct diagnosis, as many lesions are initially thought to be Bartholin's gland cysts. The majority of Bartholin's gland carcinomas are squamous cell carcinomas or adenocarcinomas; less common histologic types include adenoid cystic carcinomas and undifferentiated neoplasms. 5
The 5-year survival rate for patients with Bartholin's gland carcinoma has been reported to range from 56% 4 to 84%. 2 One series reports a 71% 5-year survival rate with a single positive inguinal node, and a 5-year survival rate <20% in patients with multiple positive inguinal nodes. 3
Current treatment recommendations call for radical local excision with margins ≥1 cm, with inguinal-femoral lymphadenectomy for resectable lesions. 1,2 Resectability depends upon the possibility of removing the tumor with adequate tissue margins without compromising function of nearby organs, such as the bladder and rectum. For nonresectable lesions, neoadjuvant radiation or chemoradiation can be administered, and resection can be performed if neoadjuvant therapy renders the lesion resectable. For patients in whom resectability is not achieved, brachytherapy with interstitial implants can be administered. 1
The role of radiologic imaging in the evaluation of Bartholin's gland carcinoma has not been definitively established. One center reports using preoperative pelvic CT scans to detect pelvic lymph node involvement in patients with clinically involved groin nodes or deeply invasive local lesions; a retroperitoneal lymph node dissection is performed in patients in whom pelvic adenopathy is identified. 1 Patients without radiologic evidence of pelvic adenopathy receive adjuvant therapy based on the status of groin nodes and the extent of local invasion.
While the clinical utility of MR imaging of vulvar and vaginal neoplasms has not been extensively evaluated, it has been suggested that MR could be useful for preoperative staging of these tumors due to the typical relatively high intensity appearance on T2-weighted images of vulvar and vaginal neoplasms compared with the low signal ring surrounding the levator muscle, urethra, and vaginal and rectal muscularis. Because of the relative hyperintensity of tumor tissue, invasion anteriorly into the urethra and posteriorly into the rectum can be appreciated. 6 A recent evaluation of MR imaging of vulvar carcinoma found that tumors >1 cm thick were identified on MR imaging and were isointense to muscle on T1weighted images and showed intermediate-to-high signal on T2 weighted images. The tumors were better visualized on T2-weighted images compared with T1-weighted images or contrast-enhanced images. The authors acknowledge that small primary tumors and thinner, plaque-like lesions were not identified, and suggest that high-resolution imaging with a small field-of-view and thinner sections might enable the identification of smaller lesions. 7
Experience with MR imaging in the evaluation of other gynecologic malignancies lends support for its use in the assessment of Bartholin's gland carcinoma and other vulvar neoplasms. MR imaging is ideal for determining tumor volume, which generally correlates with prognosis; the superior contrast resolution available with MRI allows for accurate measurements. 8 In patients with cervical cancer, MRI has been shown to be up to 93% accurate in measuring tumor size. 9-11 In a study of 99 patients with cervical carcinoma comparing CT and MR imaging, with surgical pathology as a gold standard, MR imaging was superior to CT in tumor detection (sensitivity 75% versus 51%, P <0.005) and overall tumor staging (accuracy 77% versus 69%, P <0.025). 12
Most studies report general equivalence between CT and MR imaging for the evaluation of lymph node metastases; CT is performed more commonly because of lower cost and greater availability. 13 Both CT and MR imaging rely mainly on lymph node size and number to detect abnormalities, resulting in both false-negative results (when tumor is present in nonenlarged nodes) and false-positive results (when benign hyperplastic nodes are assumed to contain tumor). 13 For the evaluation of vulvar carcinoma, one study found MR imaging to be associated with a 40% to 50% sensitivity for the detection of malignant lymph nodes, and a 97% to 100% specificity, depending on the size criteria used. 7 A meta-analysis of studies comparing CT, MRI, and lymphangiography for the diagnosis of lymph node metastases in patients with cervical cancer found no significant difference between the three modalities in overall performance, though there was a trend toward superiority of MR imaging. 14
CONCLUSION
The current case represents the first publication of an MRI study of a Bartholin's gland carcinoma; MRI provided valuable information about the extent of tumor invasion and lymph node involvement. This case illustrates that while both CT and MRI have similar abilities to detect malignant lymphadenopathy, MRI is clearly superior for the identification of a primary tumor as well as staging the local extent of disease, both of which are relevant to both prognosis and treatment planning. Therefore, we suggest that further studies be performed to evaluate the potential role of MRI as the primary radiologic modality in the workup of Bartholin's gland carcinoma.
