Breast arterial calcification: Indicator of coronary artery calcification?
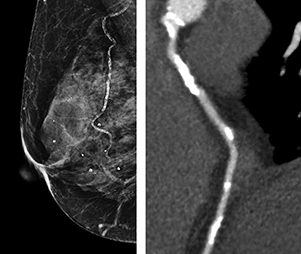
Breast arterial calcification and coronary artery
calcification in two different patients.
Breast arterial calcification (BAC) seen on mammograms of women with suspected angina due to coronary artery disease (CAD) is not an independent predictor of CAD, according to a study from Scotland of over 400 patients published in the June 2019 issue of Clinical Radiology. In fact, the diagnostic accuracy of BAC for this symptomatic patient cohort was poor.
A type of medial artery calcification of small mammary arteries or arterioles that can be seen incidentally on mammography, BAC has been studied extensively to determine if it could be a risk stratification tool for CAD. Prior studies have shown that there is an association between BAC and cardiovascular mortality, but no definitive indicators have been identified for BAC to be used as a risk stratification tool to identify CAD.
A multi-institutional team of researchers from Edinburgh used data from the Scottish Computed Tomography of the HEART (SCOT-HEART) study, a multi-center randomized controlled trial of the use of coronary computed tomography angiography (CCTA) in patients with suspected coronary artery disease, and which demonstrated that the use of CCTA changed the diagnosis and management of patients. For the sub-study, the researchers assessed the prevalence of BAC in patients who had mammograms and the association of BAC with cardiovascular risk factors, coronary artery calcification and CAD disease on CCTA.
The patient cohort included 405 patients, 73% of whom had routine screening mammograms. They identified BAC in 155 breasts of 93 patients. Co-author Michelle C. Williams, a radiologist at the University of Edinburgh British Heart Foundation Centre for Cardiovascular Science and a clinical lecturer in cardiothoracic radiology, and co-researchers reported that patients with BAC had a mean age of 63 compared to 58 who did not, and that they had a higher cardiovascular risk AASIGN score (19 vs 16 respectively).
Interestingly, 27% of the BAC patients had a smoking history compared to 51% in the non-BAC group. Patients with the highest BAC scores also had the highest percentage of non-smokers, 90% compared to 60% of the patients with the lowest BAC scores. They also had the highest percentage of family history of cardiac disease, at 52% compared to 29%.
The patients with BAC were almost evenly divided among the three severity levels of mild, moderate and severe. The authors reported that patients with BAC were more likely to have coronary artery calcification on non-contrast CT (62% compared to 49%) and had a higher median coronary artery calcium score. But patients with BAC had a similar frequency of aortic valve calcification, mitral valve calcification, and thoracic aorta calcification compared to women without BAC.
“In the present study, the absence of BAC had a high negative predictive value (NPV), but a poor positive predictive value (PPV) for the presence and severity of coronary artery calcification,” wrote the authors, adding that “the present study does not support a link between breast arterial calcification and abnormalities in the coronary arteries on non-invasive CT imaging.” They also said their study did not identify a link between breast arterial calcification and CT features of coronary artery disease, suggesting that the association between breast arterial calcification and cardiovascular mortality may be driven by mechanisms other than the presence of obstructive coronary artery disease.
“Worldwide, more women die of cardiovascular disease than breast cancer. It is very important that we find a way to identify and treat women who are at risk, but the mechanisms underlying breast arterial calcification and coronary artery calcification appear to be different,” Dr. Williams wrote in an email to Applied Radiology.
REFERENCE
- McLenachan S, Camilleri F, Smith M, et al. Breast arterial calcification on mammography and risk of coronary artery disease: a SCOT-HEART sub-study. Clin Radiol. 2019;74(6):411-490.