COVID-19 Diagnostic Imaging Recommendations
Images

COVID-19, the infectious disease caused by SARS-CoV-2, has had an immense global impact since its emergence from Wuhan, China in late 2019, and its declaration by the World Health Organization as a pandemic in March 2020. As a result, the scientific community has found itself in a race against time to control the spread of the disease with efforts aimed at early disease recognition and isolation of affected patients. Medical imaging has emerged as a useful tool in this race.
Clinical Presentation
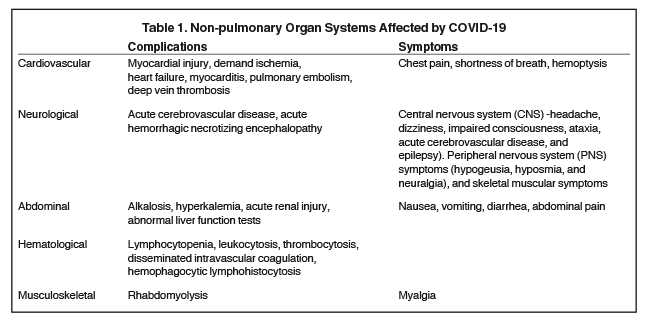
SARS-CoV-2 infection typically presents with nonspecific symptoms, ranging from fever, cough, shortness of breath and fatigue,1, 2 to gastrointestinal manifestations such as nausea, vomiting, and diarrhea (Table 1). The clinical presentation of COVID-19 overlaps with that of other respiratory viral illnesses, highlighting the critical role for diagnostic testing, including that of medical imaging.
The “COVID-19 Guidelines for Clinical Specimens” issued by the Centers for Disease Control and Prevention (CDC) recommends viral nucleic acid testing of samples collected from the upper or lower respiratory tract. The sensitivities for reverse transcription polymerase chain reaction (RT-PCR) testing are 32% for pharyngeal swab samples, 63% for nasal swab samples, and 93% for bronchoalveolar lavage fluid samples.4 Yet turnaround times for results range from hours to more than a week, likely secondary to scarcity of laboratories with PCR capabilities, and supply shortages. As a result, the U.S. Food and Drug Administration has issued multiple emergency use authorizations (EUA) to expedite development of faster diagnostic tests. The infection control measures necessary to isolate patients assumed to have COVID-19 have already strained the medical infrastructure, with critical shortages of personal protective equipment (PPE) described in the media worldwide.
Given these circumstances, radiologists are being called upon to help diagnose and treat suspected cases of COVID-19 as quickly as possible, with appropriate guidance from many of the major radiologic societies.
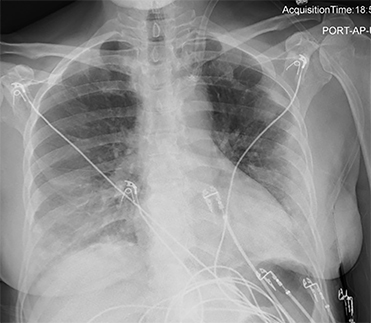
Chest Radiography
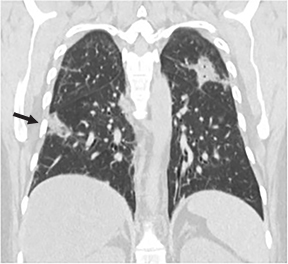
Portable chest radiography (CXR) has the advantage of eliminating the need for patient transfer and may reduce the use of PPE. However, CXR is insensitive in the detection of early disease but it can be useful to establish a baseline and as follow-up imaging for disease progression. Guan, et al,1 and Wong, et al13 found CXR to have a sensitivity of 59% for initial detection of COVID-19-related abnormalities. Radiographic abnormalities, when present, mirror those of computed tomography (CT), with bilateral lower zone- and peripherally- predominant consolidation and hazy opacities, described in detail below (Figure 1).17
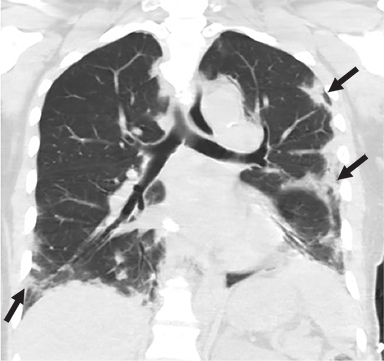
Chest CT
Much of the imaging focus is on CT. In February 2020, Chinese studies revealed that chest CT achieved a higher sensitivity for the diagnosis of COVID-19 compared with initial RT-PCR tests of pharyngeal swab samples.5,6 Subsequently, the National Health Commission of China briefly accepted chest CT findings of viral pneumonia as diagnostic of COVID-19 infection.7,8
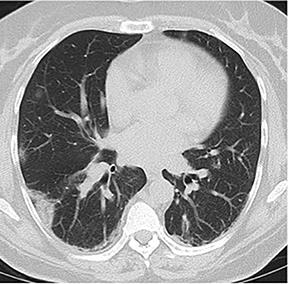
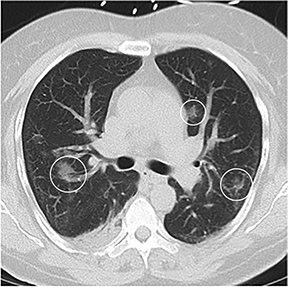
The typical appearance of COVID-19 on chest CT consists of multi-lobar, bilateral, predominantly lower lung zone, rounded ground-glass opacities, with or without consolidation, in a predominantly peripheral distribution (Figure 2).8,9 A “reversed halo” pattern and crazy paving (septal thickening) can also be seen.9 However, such findings are nonspecific; the differential diagnosis includes organizing pneumonia and other infections,10 drug reactions, and other inflammatory processes. Consequently, using CT to screen for COVID-19 may result in false positives. Moreover, the presence of abnormalities not typically associated with COVID-19 infection, including pure consolidation, cavitation, thoracic lymphadenopathy, and nodules suggests a different etiology (Figure 3).8,9
COVID-19-related chest CT abnormalities are more likely to appear after symptom onset, though they may also precede clinical symptoms. In a retrospective study by Bernheim et al, 44% of patients presenting within 2 days of symptom onset had an abnormal chest CT, while 91% presenting within 3-5 days and 96% presenting after 6 days had abnormal chest CTs.9 Shi et al found ground-glass opacities in 14 of 15 asymptomatic healthcare workers with confirmed COVID-19.11 Similarly, of 82 asymptomatic passengers with COVID-19 on the Diamond Princess cruise ship, 54% had findings of viral pneumonia on CT.12
In a prospective study by Wang et al, meanwhile, pure ground-glass opacities were the only abnormalities seen prior to symptom onset. Subsequently, 28% of patients developed superimposed septal thickening 6 to 11 days after symptom onset.13 Architectural distortion evolving from ground-glass opacities appeared later in the disease course, likely reflecting organizing pneumonia13 and early fibrosis. Long-term follow-up imaging also is needed to determine the sequelae of SARS-CoV-2 infection. In a retrospective study by Das et al, 33% of patients who recovered from MERS-CoV developed pulmonary fibrosis;14 a similar outcome following COVID-19 is likely.
Lung Ultrasound
Lung ultrasound offers low-cost, point-of-care evaluation of the lung parenchyma without ionizing radiation. The modality is especially useful in resource-limited settings.15 Peng et al found that sonographic findings in patients with COVID-19 correlated with typical CT abnormalities.16 The predominantly peripheral distribution of lung involvement facilitates sonographic visibility. Characteristic findings include thickened and irregular pleural lines, B lines (edema), and the eventual appearance of A lines (air) during recovery. Peng et al suggest that ultrasound may be useful to monitor recruitment maneuvers and guide prone positioning.16
Society Recommendations
Given the advantages and disadvantages of each of these modalities, the major radiologic societies generally advise taking a cautious approach to screening or diagnostic use of imaging in cases of suspected COVID-19. The American College of Radiology (ACR), for example, recommends against using CT for screening or as a first-line test. Instead, the College recommends that CT “be used sparingly and reserved for hospitalized, symptomatic patients with specific clinical indications…” The ACR does recommend portable CXR in ambulatory care facilities when medically necessary.
More recently, the ACR has acknowledged that “locally constrained resources are a factor in decision-making;” however, the ACR strongly cautions against the use of chest CT to “inform decisions on whether to test a patient for COVID-19, admit a patient, or provide other treatment.” The ACR states, “a normal CT should not dissuade a patient from being quarantined or provided other clinically indicated treatment when otherwise medically appropriate.”
Similarly, in a comprehensive consensus statement published in the April 2020 issues of Radiology and Chest, the Fleischner Society, an international, multidisciplinary medical society for thoracic radiology, set down appropriate, limited circumstances under which imaging may be used to evaluate patients with suspected or confirmed COVID-19, based on individual risk factors, risk of disease progression, and severity of symptoms.18
“The value of an imaging test relates to the generation of results that are clinically actionable either for establishing a diagnosis or for guiding management, triage, or therapy,” the Fleischner Society statement reads in part. “That value is diminished by costs that include the risk of radiation exposure to the patient, risk of COVID-19 transmission to uninfected healthcare workers and other patients, consumption of PPE, and need for cleaning and downtime of radiology rooms in resource-constrained environments.”
The Fleischner Society statement presents three scenarios with varying levels of pretest probability, risk of disease progression, and patient symptom severity, which guide the need for imaging. Mild respiratory disease is differentiated from moderate-to-severe respiratory disease based on the presence or absence of significant pulmonary dysfunction or damage. Pretest probability is classified as low (sporadic transmission), moderate (clustered transmission), or high (community transmission). Risk factors for disease progression include: age > 65 years, cardiovascular disease, diabetes, chronic respiratory disease, hypertension, and immune-compromised state. Importantly, imaging modality (CXR or chest CT) is left to the discretion of the clinical teams, given varying degrees of resources and expertise.
Mild Features of COVID-19
Imaging should be obtained in patients with mild respiratory features consistent with COVID-19 under a few circumstances: 1) the patient has risk factors for disease progression AND positive COVID-19 testing OR high pre-test probability in the absence of COVID-19 testing; 2) patient with mild symptoms clinically deteriorates, regardless of COVID-19 test results.
Moderate-Severe Features of COVID-19
Imaging should be obtained in patients with moderate-to-severe features of COVID-19, regardless of the results or availability of COVID-19 testing. Imaging allows for baseline analysis, risk stratification, assessment of underlying cardiopulmonary abnormalities, and identification of an alternative diagnosis in patients who have tested negative for COVID-19. If an alternative diagnosis is not revealed and CT findings are suggestive of COVID-19, repeat COVID-19 testing should be performed if the pretest probability is high.
Moderate-to-Severe Features of COVID-19 in a Resource-Constrained Environment
If point-of-care COVID-19 testing is not available or results are negative, imaging should be used to triage patients. If an alternative diagnosis is not identified and imaging findings are consistent with COVID-19, a diagnosis of COVID-19 should be presumed in areas of high pretest probability. The Fleischner Society paper recognizes that this guidance differs from other published recommendations; it is based upon the panelists’ direct experience with these clinical scenarios.
In addition to the above scenarios, the Fleischner Society paper recommends against the daily use of CXR in stable intubated patients with COVID-19, and supports the use of chest CT in patients with pulmonary functional limitations after resolution of COVID-19.
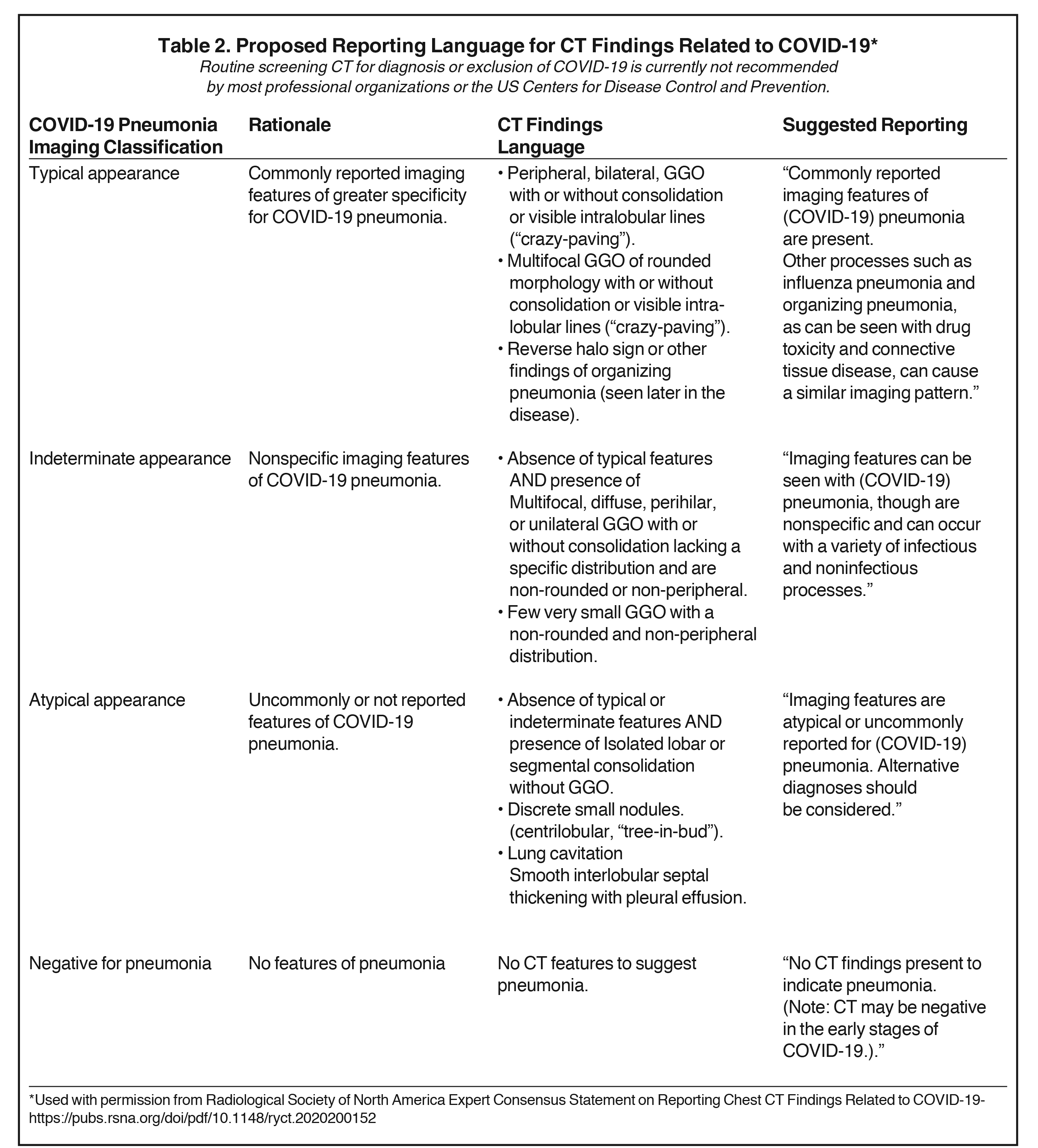
The Radiological Society of North America (RSNA), together with the ACR and Society of Thoracic Radiology, issued a consensus statement that although CT should not be used to diagnose COVID-19, radiologists must be prepared to interpret CT performed on patients suspected of having COVID-19, as well as incidental pulmonary findings consistent with COVID-19 infection. The RSNA has created a standardized reporting template to help improve communication with providers and contribute to efficient patient care (Table 2).19
Other radiologic organizations have also taken steps or issued guidelines to ensure the safe, appropriate use of medical imaging with respect to COVID-19. The Society of Advanced Body Imaging has posted to its website a webinar on COVID-19, and the Society of Cardiovascular Computed Tomography recommends rescheduling non-urgent imaging studies, in accordance with CDC guidelines.20 Similarly, the North American Society for Cardiovascular Imaging recommends consolidating imaging studies and substituting noninvasive tests for semi-invasive or invasive tests. The American Journal of Neuroradiology published an article, “What Neuroradiologists as Citizens of the World Need to Know,” summarizing the virology, epidemiology, presentation, diagnosis, and treatment of COVID-19.21 The ACR recommends that nuclear medicine ventilation scans not be used unless absolutely necessary and only if appropriate infection control precautions are met. It also advocates postponement of elective magnetic resonance imaging studies.
Physician Resources and Future Implications
With respect to COVID-19’s effects on staffing, efforts have been made to diminish crowding in reading rooms, rotating staff across multiple sites when possible and establishing home picture archiving communication system (PACS) capability via actual PACS and virtual desktop infrastructure. While radiologists with risk factors for disease severity are working remotely wherever possible, in areas of higher COVID-disease prevalence, trainees and some attending physicians are being re-deployed on the front lines of patient care. The decrease in study volume related to cancellation of elective services is requiring radiology practices to adjust their business plans.22 In a recent article published in Radiology, Cavallo and Forman state that minimizing staffing disruption will be necessary to restore or exceed baseline capacity in anticipation of a potential rebound in imaging study volume in the aftermath of the pandemic.22 They suggest devising strategies to reduce overhead expenses, while noting that staffing adjustments such as furloughs, salary cuts, bonus suspensions, and layoffs may be unavoidable. While patients who have had deferral of imaging studies will predictably return to restore volume, practices can expect to receive a lower payout given a substantial decrease in patients with private insurance.22 The recently passed CARES Act and pending legislation will likely provide an element of relief to practices through loans and tax deferments.22
Conclusion
The COVID-19 pandemic has confronted the radiology community with a series of challenges that are unprecedented in recent history. In promoting the judicious use of imaging to facilitate and maximize the quality of patient care, all radiologists play a critical role in helping to prevent, control, and halt the spread of the disease.
References
- Guan WJ, Ni ZY, Hu Y, et al. Clinical Characteristics of Coronavirus Disease 2019 in China [published online ahead of print, 2020 Feb 28. N Engl J Med. 2020; NEJMoa2002032. doi:10.1056/NEJMoa2002032
- Huang C, Wang Y, Li X et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet. 2020;395(10223):497-506. doi:10.1016/s0140-6736(20)30183-5
- Pan L, Mu M, Ren HG, et al; on behalf of the Wuhan Medical Treatment Expert Group for COVID-19. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study [published online March 5, 2020. Am J Gastroenterol. doi:10.14309/ajg.0000000000000620
- Wang W, Xu Y, Gao R, et al. Detection of SARS-CoV-2 in Different Types of Clinical Specimens. JAMA. Published online March 11, 2020. doi:10.1001/jama.2020.3786
- Ai T, Yang Z, Hou H et al. Correlation of Chest CT and RT-PCR Testing in Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology. 2020:200642. doi:10.1148/radiol.20202006426.
- Fang Y, Zhang H, Xie J et al. Sensitivity of Chest CT for COVID-19: Comparison to RT-PCR. Radiology. 2020:200432. doi:10.1148/radiol.2020200432
- Yuen KS, Ye ZW, Fung SY, Chan CP, Jin DY. SARS-CoV-2 and COVID-19: The most important research questions. Cell Biosci. 2020; 10:40. Published 2020 Mar 16. doi:10.1186/s13578-020-00404-4
- Zu Z, Jiang M, Xu P et al. Coronavirus Disease 2019 (COVID-19): A Perspective from China. Radiology. 2020:200490. doi:10.1148/radiol.2020200490
- Bernheim A, Mei X, Huang M et al. Chest CT Findings in Coronavirus Disease-19 (COVID-19): Relationship to Duration of Infection. Radiology. 2020:200463. doi:10.1148/radiol.2020200463
- Hope M, Raptis C, Shah A, Hammer M, Henry T. A role for CT in COVID-19? What data really tell us so far. The Lancet. 2020;395(10231):1189-1190. doi:10.1016/s0140-6736(20)30728-5
- Shi H, Han X, Jiang N et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. The Lancet Infectious Diseases. 2020;20(4):425-434. doi:10.1016/s1473-3099(20)30086-4
- Inui S, Fujikawa A, Jitsu M et al. Chest CT Findings in Cases from the Cruise Ship “Diamond Princess” with Coronavirus Disease 2019 (COVID-19). Radiology: Cardiothoracic Imaging. 2020;2(2):e200110. doi:10.1148/ryct.2020200110
- Wang Y, Dong C, Hu Y, et al. Temporal Changes of CT Findings in 90 Patients with COVID-19 Pneumonia: A Longitudinal Study. Radiology. 2020:200843. doi:10.1148/radiol.2020200843
- Das KM, Lee EY, Singh R, et al. Follow-up chest radiographic findings in patients with MERS-CoV after recovery. Indian J Radiol Imaging. 2017;27(3):342–349. doi:10.4103/ijri.IJRI_469_16
- Stewart KA, Navarro SM, Kambala S, et al. Trends in Ultrasound Use in Low and Middle Income Countries: A Systematic Review. Int J MCH AIDS. 2020;9(1):103–120. doi:10.21106/ijma.294
- Peng QY, Wang XT, Zhang LN; Chinese Critical Care Ultrasound Study Group (CCUSG). Findings of lung ultrasonography of novel corona virus pneumonia during the 2019-2020 epidemic [published online ahead of print, 2020 Mar 12]. Intensive Care Med. 2020;1–2. doi:10.1007/s00134-020-05996-6
- Wong HYF, Lam HYS, Fong AH-T, et al. Frequency and Distribution of Chest Radiographic Findings in COVID-19 Positive Patients. Radiology. 2019:201160. doi:10.1148/radiol.2020201160
- Rubin G, Haramati L, Kanne J et al. The Role of Chest Imaging in Patient Management during the COVID-19 Pandemic: A Multinational Consensus Statement from the Fleischner Society. Radiology. 2020:201365. doi:10.1148/radiol.2020201365
- Simpson S, Kay F, Abbara S et al. Radiological Society of North America Expert Consensus Statement on Reporting Chest CT Findings Related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA. Radiology: Cardiothoracic Imaging. 2020;2(2):e200152. doi:10.1148/ryct.2020200152
- Mahajan A, Hirsch J. Novel Coronavirus: What Neuroradiologists as Citizens of the World Need to Know. American Journal of Neuroradiology. 2020;41(4):552-554. doi:10.3174/ajnr.a6526
- Choi AD, Abbara S, Branch KR, et al. Society of Cardiovascular Computed Tomography Guidance for Use of Cardiac Computed Tomography Amidst the COVID-19 Pandemic. J Cardiovasc Comput Tomogr. 2020. doi:10.1016/j.jcct.2020.03.002
- Cavallo, J. and Forman, H., 2020. The Economic Impact of the COVID-19 Pandemic on Radiology Practices. Radiology epub https://pubs.rsna.org/doi/10.1148/radiol.2020201495.
Citation
C C, R H, CS W. COVID-19 Diagnostic Imaging Recommendations. Appl Radiol. 2020; (3):10-15.
May 4, 2020