Eagle Barrett Syndrome (also known as prune-belly syndrome [PBS]) in an adult
Images

Prepared by Christopher Wen, MD and Allen J. Cohen, PhD, MD from the Department of Radiological Sciences; and Dorothy J. Marquez, MD from the Department of Medicine, University of California, Irvine Medical Center, Orange, CA.
CASE SUMMARY
A 17-year-old Hispanic adolescent boy presented to the emergency department with a 6-hour history of right flank pain and hematuria. Recently, in a South American country, he had had a diagnosis of bilateral hydronephrosis and a right orchiectomy for an undescended testis. Laboratory results were remarkable for a white blood cell count of 11,000 and a urine analysis of 2+ white blood cells and 50 red blood cells/high-power field. The serum creatinine was 1.1 mg/dL. The clinicians suspected pyelonephritis, and a noncontrast computed tomography (CT) scan of the abdomen and pelvis was performed (Figure 1). An intravenous urogram (IVU) was also obtained 12 days later (Figure 2). The patient was seen in the urology clinic, where a physical examination found a descended left testis and an empty right hemiscrotum. The patient was treated with antibiotics for a urine culture positive for Escherichia coli .
DIAGNOSIS
Eagle Barrett Syndrome (also known as prune-belly syndrome [PBS]) in an adult
IMAGING FINDINGS
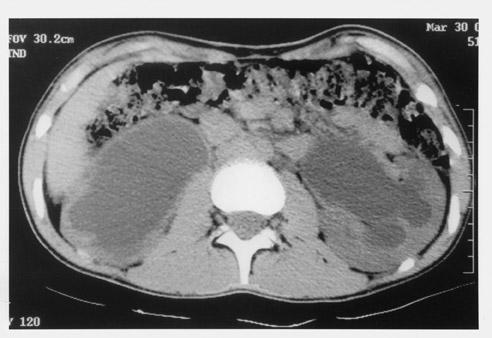
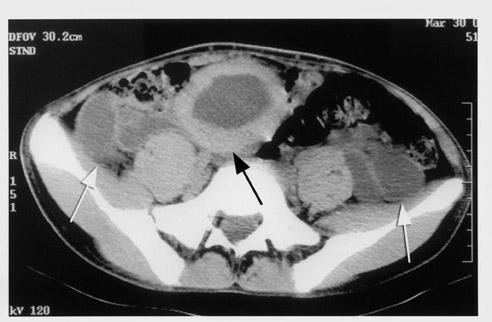
Noncontrast CT scan of the abdomen shows massive hydronephrosis, with the right kidney worse than the left (Figure 1A), marked bilateral redundant hydroureter, a thick-walled bladder, and absent abdominal wall musculature (Figure 1B). A postvoid film from an IVU showed a poorly functioning right kidney with a massive renal pelvis and marked left hydronephrosis and redundant hydroureter (Figure 2).
DISCUSSION
Prune-belly syndrome is a congenital disorder characterized by the clinical triad of cryptorchidism, hypoplasia of the abdominal musculature, and abnormalities of the urinary tract. The term "prune belly" reflects the characteristic wrinkled appearance of the abdominal wall in the newborn due to the complete or partially complete absence of abdominal wall muscles. In adolescent and adult life, the abdomen often assumes a smooth "pot-belly" configuration. In the United States, the incidence of PBS is 1 in 35,000 to 50,000 live births; it occurs in all races. There are other associated anomalies, including clubfoot, intestinal malrotation, pulmonary dysplasia, congenital hip dislocation, and cardiac defects due to the sequela of oligohydraminos in utero. 1 Ninety-five percent of cases occur in males. Diagnosis is made in utero using ultrasound (US) or in the neonate with characteristic clinical findings. The diagnosis is suspected in the fetus when US imaging reveals an enlarged bladder, dilated ureters, and an abnormal abdominal wall. However, the same constellation of US findings can be caused by posterior urethral valves (PUV) with severe hydroureteronephrosis. Amniotic fluid volume may be normal or decreased in neonates with PBS. Occasionally, PBS can be seen in older children or adults with renal failure, recurrent infections, or hypertension.
Morbidity relates to the degree of dilation of the urinary tract, in which poor ureteral peristalsis and weak forward propulsion of urine in the ureters results in stasis, infection, and stone formation. Renal failure results from underlying renal dysplasia and the aforementioned complications of urinary stasis. Twenty percent of patients are stillborn, 30% die of renal failure or urosepsis within the first 2 years of life, and the remaining 50% have varying degrees of urinary pathology.
In the 1970s, half of the patients with PBS died in early infancy. Currently, the survival rate has improved markedly. The severe abdominal distention also is marked by pulmonary hypoplasia related to the patient's large abdominal contents and compromise of the thorax during fetal development.
Older theories postulated that lower urinary tract obstruction at the level of the prostate caused overdistension of the bladder. In turn, hydroureter and hydronephrosis developed. The mass effect from the dilated upper urinary tract interfered with descent of the testes and development of abdominal wall musculature. 1 Newer hypotheses ascribe the syndrome to a gestational insult disrupting mesodermal development. Embryogenesis of the abdominal wall musculature and lining of the genitourinary tract are consequently damaged. 1 The genetic basis of PBS is uncertain. An X-linked defect is suggested by the predominance of affected males. However, females can be affected, casting doubt upon this observation.
Hydronephrosis and varying degrees of renal dysplasia are present in >50% of cases. There may be clubbing of the calyces, narrowing of infundibula, and cyst formation. The ureters often exhibit gross dilation, elongation, and tortuosity due to replacement of smooth muscle with fibrous tissue. The distal ureter is more affected than the proximal ureter. Often, the bladder is enlarged and nontrabeculated because of the replacement of smooth muscle by collagen. It can be elongated and attached to a patent urachus or urachal diverticulum superiorly. The prostate is markedly hypoplastic, leading to dilation of the prostatic urethra. The anterior urethra is abnormal in 70% of cases, often in the form of a scaphoid megalourethra. Females can have urethral atresia. Virtually all males have bilateral undescended testes. Females usually have normal ovaries, but abnormalities of the uterus and vagina.
Historically, the diagnosis was made based on: 1) physical examination; 2) a chest radiograph showing hypoplastic lungs and distended flanks; and 3) IVU findings of dilated and clubbed renal calyces, markedly dilated and tortuous ureters, and a large vertical trabeculated bladder. Radiologic findings in PBS that distinguish it from PUV include greater dilation and redundancy of the distal thirds of the ureters and anterior urethral abnormalities. 2,3 In some rare cases, urethroscopy may be necessary to differentiate these entities. With the increasing use of noncontrast CT to evaluate the genitourinary system, awareness of the appearance of PBS on CT is important.
TREATMENT AND PROGNOSIS
The prognosis depends on the severity of the abnormalities. The presentation can range from stillborn fetuses to older children with recurrent infections and renal insufficiency. Orchiopexy is required due to the increased risk of malignancy in undescended testes. Repair of the abdominal wall musculature is not simply cosmetic, as it plays an important role in pulmonary, bladder, and intestinal function and is crucial in the surgical management of these patients. 4
CONCLUSION
The diagnosis of PBS should be made in an adult whose CT scans show renal hypoplasia, hydronephrosis, redundant hydroureter, and deficient anterior abdominal musculature.