Enterprise Imaging: CT radiation dose management
Images
Sir Godfrey Newbold Hounsfield was an English electrical engineer credited with developing the diagnostic imaging technique of computed tomography (CT) and with creating the first commercially viable CT scanner in Hayes, England, back in 1972. Sir Hounsfield would no doubt be proud of the success of this technology in health care. Thanks to his invention, exploratory surgery, once commonplace in ‘diagnostics,’ is now a rare procedure. Undoubtedly an invaluable diagnostic tool, the number of CT examinations ordered in the United States(U.S.) has grown from 26 million in 1998 to 85.3 million in 2011.1 Medical exposure to ionizing radiation constitutes nearly half of the total radiation exposure of the U.S. population from all sources. Americans are exposed to > 7 times as much ionizing radiation from medical procedures today than during the early 1980’s, due in most part to the higher utilization of CT.2
While the trajectory in the growth of CT volume is not as steep as the double-digit growth experienced in the 2000s, the continued upward trend in usage and the direct correlation to increased risk of cancer opens up CT radiation dose management to many opportunities to find the perfect balance between the acceptance of the risks associated with radiation versus the benefits to be gained from the use of radiation.
Fundamentals of dose parameters: A push towards personalized dose protocols
A significant part of the challenge of patient dose management in CT arises from the fact that overexposure in CT is frequently not detected. In contrast to film-based radiography, where overexposure results in a dark image, increasing dose in CT and other digital imaging techniques results in images with less noise (improved visual appearance) and fewer streak artifacts, although not necessarily with greater diagnostic information. Hence, we often find that image quality in CT often exceeds the clinical requirements for diagnosis.
This of course points to the importance of being able to accurately measure and quantify the radiation dose. While the ultimate goal is a personalized approach to radiation dose management, we have to start with the basics. All CT units display the Computed TomographyDose Index (CTDI), a measure of the quantity of radiation output by the scanner for a particular study. This is often displayed alongside the dose length product (DLP), which is an indicator of the integrated radiation dose of an entire CT examination.
These measurements, however, are based on measuring the absorbed dose in a cylindrical acrylic phantom with a 10-cm pencil ion chamber in the phantom’s center hole and again in one of the phantom’s peripheral holes. This is arguably practical, but it is not personalized to the specific patient.
Radiation dose units include absorbed dose, which is the energy absorbed per unit mass of tissue; equivalent dose, which takes into account the radiation weighting factor; and effective dose, which takes into account the relative sensitivities of various tissues to radiation. The effective dose allows the health care provider to make an estimate of relative patient risk.
However, every patient is unique, and data from phantom-based simulations is not quite the real thing, since most of the data is averaged out and less specific. This is pushing for a level of scanning protocol optimization and dose personalization that we have not seen before.While most CT scanners do a good job of reporting the amount of energy they emit, it often takes sophisticated analysis to determine what this means at a personalized level to each patient.
Going beyond the headline news
Public hype around radiation dose exposure has reached an all-time high with the increasing use of airport scanners and threats to boycott the scans and opt for pat-downs instead. While airport scanners are worthy catalysts for debate on radiation dose management, the reality is that these are, in the larger scheme of things, quite harmless. One scan from a typical “backscatter” security scanner might deliver 0.005to 0.01 millirem—far below the 10,000 millirem considered the danger threshold. A traveler would require > 1,000 such scans in a year to reach the effective dose equal to one standard chest x-ray.
News related to radiation dose and CT scanning often hits the media in the worst ways possible, and unfortunately, makes the headlines quite often. In 2008, Cedars-Sinai Medical Center in Los Angeles revealed that, over a period of 18 months, 206 patients received 8 times the dose normally delivered using a CT brain-perfusion scan. This exacerbated nationwide concerns that patients are exposed to excess radiation during medical testing. A Los Angeles Times article about the incident described the scanner error in almost Hollywood terms: Somebody should have noticed. But nobody did—everybody trusted the machines.3
But these attention-grabbing headlines are not far and few in between. The radiation overdoses point to a problem well-documented in medicine over the last decade—the need for multiple backup systems to catch mistakes and a more organized approach to managing CT utilization.
Managing CT utilization
Radiation exposure from CT scans is cumulative over a patient’s lifetime. The risk associated with a radiation dose from a single CT scan is relatively small when compared with the clinical benefit of the procedure. But patients are increasingly undergoing multiple CT scans and other radiation-based procedures, which can lead to unnecessary radiation risk. The increasing utilization can be categorized into 3 components:
- Appropriate imaging: targeted towards expedience of diagnosis and more often based on satisfying appropriateness criteria as defined by the American College of Radiology (ACR);
- Inappropriate imaging: mostly variants of defensive medicine, patient demands and even self-referrals; and,
- Screening exams.
Handling the challenges of increased CT utilization can be boiled down to 3 basic areas:
- Imaging appropriateness and decision support: The ACR advises that no imaging exam should be performed unless a clear medical benefit outweighs any associated risk.
- Dose optimization: This entails choosing imaging parameters and performing the exams to yield optimal diagnostic information while minimizing overall dose to the patient.
- Dose limitation: This includes ensuring that we keep dose to the patient ‘as low as reasonably achievable’ (ALARA), a guiding principle that requires the lowest radiation dose that will yield the most appropriate image quality for a particular patient to enable the correct clinical decision.
Pediatric imaging and dose management challenges
Numerous academic publications and other print media have highlighted startling statistics about children and CT imaging. JAMA Pediatrics recently published the results of the HMORN Cancer Research Network (CRN) study that tracked an increase in CT use over a15-year period.4 It was found that increased use of CT in pediatrics, combined with the wide variability in radiation doses, resulted in many children receiving a high-dose examination. The researchers projected that the 4 million CT scans of the head, abdomen/pelvis, chest or spine in the U.S. pediatric population could cause 4,870 future cancers. They also stated that this number could be reduced dramatically—by62%—if doses were reduced by using standardized protocols and guidelines, such as Image Gently, and by eliminating unnecessary imaging.
The use of CT doubled for children under age 5 and tripled for children aged 5 to 14 between 1996 and 2005. CT use remained stable in2006 and 2007, and then began to decline. Startling, too, was the variability in the radiation doses administered where effective doses varied from 0.03 to 69.2 mSv per scan.
A now famous separate Duke study5 from 2000 to 2006 found that while the pediatric emergency department (ED) patient volume increased in that time period by just 2%, and triage acuity remained stable, the number of pediatric ED scans increased by 435% for chest CTs and 366% for cervical spine CTs. These findings were shocking, given that children are at greater risk from a given dose of radiation compared with adults due to their body’s increased radiosensitivity and the greater period of time in which to manifest these changes.
Obesity and CT radiation dose risks
Obese patients often face higher radiation exposure from CT scans. Research shows that the internal organs of obese men receive 62% more radiation during a CT scan than those of average-weighted men.6 Often, when technicians use normal equipment settings to performa CT scan on an obese patient, the resulting images are blurry, as the x-ray photons have to travel further and make their way through extra layers of fatty tissue. As a result, the equipment is adjusted to a more powerful setting, producing better image quality, but exposing the obese patient to unnecessary additional radiation. There is, however, promising work being done on personalized phantoms and ultra-realistic, 3-dimensional computer models of patients, resulting in much more accurate and personalized protocols.
State dose legislation: The California effect
In October 2010, California Gov. Arnold Schwarzenegger signed a new radiation patient protection law that mandates strict procedures and reporting requirements for CT scanners and radiation therapy procedures, as well as reporting of radiation overdoses to the state Department of Public Health. All CT systems must record the dose of radiation on every study by putting the data directly in the radiology report or attaching the protocol page to the actual radiology report. Connecticut and Texas have already followed California’s example with their own legislation; other states are expected to enact similar reporting requirements.
Modality vendor innovations
When differentiating CT capabilities, dose is now king. The CT-slice wars have now given way to the dose wars among modality vendors, and this is deemed a positive development.
Providers have become more discriminating regarding dose-reduction strategies, resulting in dose moving up the decision tree and becoming very influential in new CT purchases. Improvements in dose management technology are evident in most CT scanners, particularly in the next-generation systems.
CT modality vendors are getting creative and innovative around radiation-dose reduction and management. GE’s VCT and the Discovery CT750 HD CT scanners received kudos for their dose-reduction capabilities and ASiR (Adaptive Statistical Iterative Reconstruction)technology. Philips is approaching dose reduction with better protocols and image reconstruction. The company’s Brilliance iCT 256 scores highly, and there is much progress made with the iDose and iDose4 packages. Siemens is being viewed as another leader in dose optimization. The company’s plus points include development of IRIS and SAFIRE (iterative reconstruction), with dose optimization technologies,such as CARE Dose 4D. Toshiba is providing software upgrades that allow reduced dose and faster procedure speeds, especially on the Aquilion ONE 320-detector row CT.
Add-on or packaged iterative reconstruction software is now proven to reduce noise while creating a clearer CT image at a lower dose.Recent studies have shown significant reduction of radiation dose, up to 40% to 50%, with some vendors claiming a 50% to 70% CT dose reduction with no compromise in image quality and diagnostic value.
Continued innovation
The cry for better innovation in radiation dose reduction continues to be heeded, and every year, we see progressive advancements in various areas. Some of the highlights include:
- Stopping excessive radiation exposure before it occurs by using a unique software platform (DoseMonitor™ PHS Technologies Group,LLC ), which identifies patients who may be at risk for ionizing radiation overexposure at the time a test is ordered.7
- Automatic tracking of radiation dose exposure, with patient-size adjusted dose correction.8
- Automated extraction of radiation dose information for CT.9
- Including ability to extract information from dose sheets produced by legacy CT scanners that cannot generate DICOM radiation dose structured reports.
ACR’s National Radiology Dose Registry,10 which started as a pilot program, now entails an improvement process that includes more vendors, incorporates patient size, and ongoing work with Integrating the Healthcare Enterprise (IHE) on Radiation Exposure Monitoring(REM) Profile.
Future of dose management
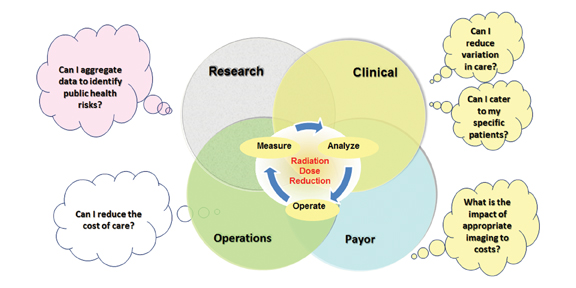
The effective management of radiation dose has a broad set of needs across health care domains, as represented in Figure 1. Minimizing unnecessary radiation is becoming a priority for medical imaging facilities, especially with increasing oversight now commonplace from state regulatory agencies and accrediting bodies. A significant driving force, too, is value-based imaging, with imaging appropriateness being a key requirement.
Perhaps the lowest-hanging fruit in the journey to effective CT radiation-dose management is broadening awareness, including heightened patient and public education, stating the facts, and clearing the confusion. A number of professional association initiatives have a lotto offer, and these include the Image Gently alliance, which raises awareness of opportunities to lower radiation dose in the imaging of children; the Step Lightly campaign for interventional dose reduction; and the Image Wisely campaign, an ACR-RSNA task force on radiation protection for adults.
When sophisticated and expensive equipment become available in hospitals and imaging centers, there are inevitable pressures to expand applications. Today, we are seeing an increase not just in the utilization of CT scans but also in the wider availability of CT scanners and an increasing set of indications for CT use. This subsequently leads to a rapid increase in the number of protocols, and, ultimately, to protocol variance and complexity. As a responsible industry, we must continue to push for greater levels of personalized dose-management capabilities and automation along with technological advancements in every facet of the CT imaging workflow.
References
- 2012 CT market outlook report. IMV Medical Information Division. http://www.imvinfo.com/index.aspx?sec=def&sub=dis&pag=dis&ItemID=200081. Accessed August 6, 2013.
- Ionizing radiation exposure of the population of the United States. National Council on Radiation Protection & Measurements. NCRP. http://www.ncrppublications.org/reports/160.Accessed August 6, 2013.
- Zarembo A. Cedars-Sinai radiation overdoses went unseen at several points. Los Angeles Times. http://articles.latimes.com/2009/oct/14/local/me-cedars-sinai14. Updated October 14, 2009. Accessed August 1, 2013.
- Miglioretti DL, Andrew Williams A. The use of computed tomography in pediatrics and the associated radiation exposure and estimated cancer risk. JAMA Pediatr. 2013;167:8.
- Broder J, Fordham LA, Warshauer DM. Increasing utilization of computed tomography in the pediatric emergency department. Emerg Radiol. 2007;14:227-232.
- Ding A, Mille MM, Liu T, et al. Extension of RPI-adult male and female computational phantoms to obese patients and a Monte Carlo study of the effect on CT imaging dose. Phys Med Biol. 2012;57:2441-2459.
- DoseMonitor. DoseMonitor™ PHS Technologies Group, LLC. www.dosemonitor.com. Accessed August 1, 2013.
- Image Safely. www.imagesafely.com. Accessed August 1, 2013.
- Radiation Dose Intelligent Analytics for CT Examinations. www.radiancedose.com. Accessed August 1, 2013.
- Dose Index Registry. Am Coll Radiol. http://www.acr.org/Quality-Safety/National-Radiology-Data-Registry/Dose-Index-Registry. Accessed August 1, 2013.