Giant bilateral hemorrhagic adrenal myelolipomas
Images

CASE SUMMARY
A 52-year-old male presented with two days of left flank pain associated with nausea and vomiting. Physical exam revealed left flank tenderness; however, serum chemistries and CBC were within normal limits. Abdominal CT showed bilateral adrenal masses, left larger than right. Surgical resection of the lesions yielded well-circumscribed specimens with smooth capsules and heterogenous internal composition consisting of adipose tissue and blood products. The patient experienced an uneventful recovery.
IMAGING FINDINGS
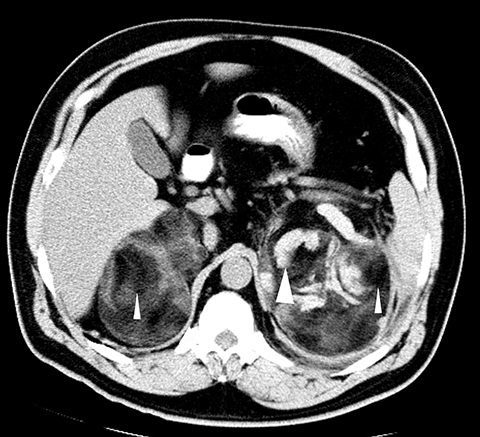
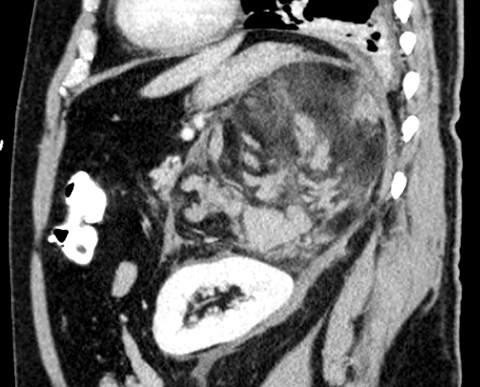
Computed tomography revealed bilateral, left larger than right, heterogeneous, well-circumscribed masses replacing the adrenal glands that contained regions of fat density (Figure 1). Additionally, the left mass exhibited high density areas indicative of hematoma with hemorrhage tracking inferiorly and surrounding the left kidney (Figures 1, 2). The lesions exerted mass effect upon the kidneys, liver, and stom- ach, but did not originate from them (Figures 2, 3).
DIAGNOSIS
Giant bilateral hemorrhagic adrenal myelolipomas
DISCUSSION
Adrenal myelolipomas are rare benign tumors composed of adipose tissue and hematopoietic cells resembling bone marrow.1 They are postulated to arise from metaplasia of adrenal cortical cells when subjected to chronic stress or degeneration.1 Epidemiologically, adrenal myelolipomas comprise 3 percent to 5 percent of primary adrenal tumors and have a mean age at presentation in the sixth decade of life without a particular gender predilection.2 Typically, the lesions are unilateral; however, bilateral tumors occur in about 10 percent of cases.3,4 Although most adrenal myelolipomas do not produce hormones, over 25 cases of associated endocrine dysfunction have been described in the literature, with congenital adrenal hyperplasia and Cushing Syndrome being the most common.5 While usually asymptomatic at discovery, abdominal and back pain may occur in large or hemorrhagic myelolipomas.3
The diagnosis of adrenal myelolipoma can be made with CT, ultrasound, or MRI. Computed tomography findings include a well-marginated, heterogeneous mass with macroscopic fat. In some areas of the lesion, the admixture of adipose and hematopoietic cells results in a “smoky” appearance to the fat with attenuation values approximately 20-30HU.1 In approximately one-quarter of cases, the lesions display internal calcification.2 Distinction is made between the adrenal myelolipoma and adenoma, as the latter is denser and more homogenous than the former. Although retroperitoneal liposarcomas may contain internal fat, they typically have an infiltrative appearance while the borders of adrenal myelolipomas are well-defined by a capsule. While adrenal angiomyolipoma may be a diagnostic consideration, it is much less likely to arise from the adrenal glands than from the kidneys.3
Under ultrasound, adrenal myelolipoma may present as a hyperechoic mass reflecting fatty content, with relatively hypoechoic regions that correspond to areas of myeloid cells. The heterogeneous echogenicity of most lesions reflects the non-uniform mixture of its two primary constituent tissues. Internal calcifications manifest as hyperechoic areas with acoustic shadowing.1 The presence of acute hemorrhage results in areas that are hypoechoic relative to fat.1
On MRI, adrenal myelolipomas may exhibit one of three patterns. Lesions that are primarily composed of adipose tissue are hyperintense masses on T1-weighted sequences and intermediate intensity on T2-weighted sequences.6 Regions of adipose tissue lose signal intensity on fat- suppressed sequences, with persistent areas of signal intensity either representing myeloid elements or hemorrhage.6,1 Opposed-phase imaging also demonstrates the presence of fat as low signal intensity.1 Tumors with mixed fatty and myeloid elements appear heterogenous, exhibiting foci of fatty signal and additional foci of hyperintensity on T2-weighted and contrast-enhanced T1-weighted sequences. Adrenal myelolipomas that are primarily composed of myeloid tissues display hypointensity relative to liver on T1, hyperintensity relative to liver on T2, and enhancement on post-contrast sequences.6
In one series of 75 pathologically proven cases of adrenal myelolipoma, all but two displayed definitive regions of fat on CT.1 In cases of non-classic imaging findings, fine needle aspiration biopsy may be considered for further workup, as demonstration of mature adipocytes and hematopoietic elements is diagnostic of myelolipoma.7
Recommendations for the management of adrenal myelolipomas are predicated on size and symptomatology. For symptomatic myelo- lipomas or those larger than 7 cm, excision is advocated given the propensity of some lesions to grow significantly during the observation period and hemorrhage spontaneously or following minor trauma. For asymptomatic lesions measuring less than 4 cm, the risk of spontaneous hemorrhage is sufficiently small to warrant expectant monitoring. Rare hormonally active lesions should be removed. Following surgical excision, lesions typically do not recur. In cases of bilateral adrenal myelolipoma excision, lifelong steroid substitution is required.3
CONCLUSION
Adrenal myelolipomas are benign tumors composed of mature adipocytes and myeloid tissue. They are typically asymptomatic; however, large or hemorrhagic lesions may elicit abdominal or back pain. Rarely, they are bilateral or hormonally active. On CT, ultrasound and MRI, the tumors are well-circumscribed and follow the attenuation, echogenicity, and signal intensity of fat, which may be altered by the presence of the hematopoietic elements, hemorrhage or calcification. Although small and asymptomatic lesions may be managed expectantly, surgical resection is advocated for lesions that are greater than 7 cm, elicit symptoms, or are hormonally active.
REFERENCES
- Rao P, Kenney PJ, Wagner BJ, Davidson Imaging and pathologic features of myelolipoma. Radiographics. 1997;17:1373-1385.
- Lam KY, Lo Adrenal lipomatous tumours: A 30 year clinicopathological experience at a single institution. J Clin Pathol. 2001;54:707-712.
- Daneshmand S, Quek Adrenal myelolipoma: Diagnosis and management. Urol J. 2009; 2:71-74.
- Civrilli K, Damry N, Steppé R, et Bilateral adrenal myelolipomas. Journal Belge de Radiologie. 2008;91:90.
- Umpierrez MB, Fackler S, Umpierrez GE, Rubin Adrenal myelolipoma associated with endocrine dysfunction: Review of the literature. Am J Med Sci. 1997;314:338-341.
- Elsayes KM, Mukundan G, Narra VR, et Adrenal masses: MR imaging features with pathologic correlation. Radiographics. 2004;24:S73-S86.
- Wadih GE, Nance KV, Silverman Fine-needle aspiration cytology of the adrenal gland. Fifty biopsies in 48 patients. Arch Pathol Lab Med. 1992;116:841-846.
Citation
R LSAB. Giant bilateral hemorrhagic adrenal myelolipomas. Appl Radiol. 2016;(4):32-34.
April 4, 2016