Gorham-Stout Syndrome
Images
CASE SUMMARY
A 53-year-old was evaluated for right proximal upper extremity pain and progressive limitation of shoulder joint movement over a period of six years. The patient had type 2 diabetes mellitus. There was no fever, history of trauma, or any other disease. All blood testing was normal, including alkaline phosphatase. Clinical examination and other imaging methods identified no neurological or vascular etiology.
IMAGING FINDINGS
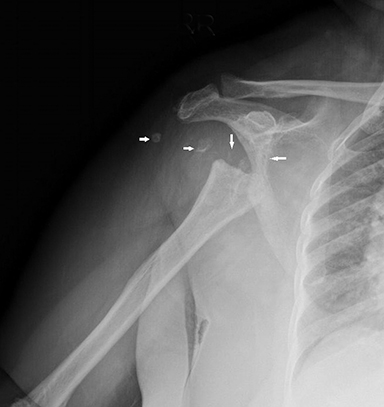
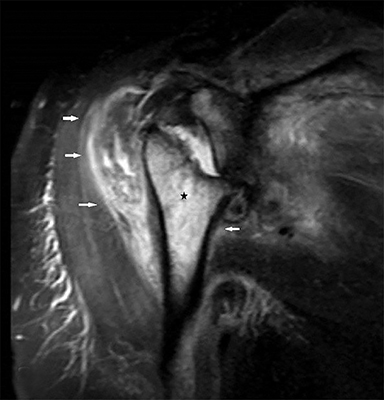
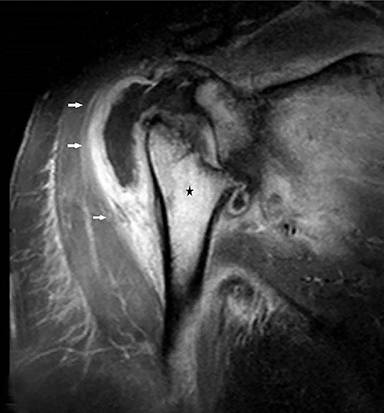
Anteroposterior radiography of the right shoulder demonstrated absence of the humeral head with tapering of the remaining bone tissue. There were accompanying millimeter-sized bone fragments in the adjacent soft tissue (Figure 1). Coronal T2 fat-saturated magnetic resonance imaging (MRI) revealed humeral head loss with prominent medullary bone edema in the metaphysodiaphyseal portion of the humerus and glenoid (Figure 2). These bone segments and the surrounding soft tissue enhanced markedly following intravenous contrast administration. MRI also showed increased joint fluid and signs of synovitis. Histopathological evaluation was reported as nonspecific proliferative, inflammatory disease.
DIAGNOSIS
Gorham-Stout syndrome (GSS)
DISCUSSION
Gorham-Stout syndrome, which is also referred to as “vanishing bone disease,” is a rare disorder characterized by the disappearance of one or more bones. Etiopathology of this disease is unclear. Research suggests the condition arises from nonmalignant proliferation of hemangiomatous or lymphangiomatous tissue, resulting in progressive destruction and absorption of the affected bone.1,2 One or more bones, most commonly the skull, upper and lower extremities, spine, and pelvic bones, may be affected.2 Gorham-Stout syndrome has been reported in the literature as occurring most commonly in males up to 40 years of age; however, our patient did not fit these demographics.2,3
Clinical findings include pain, swelling, loss or restriction of motion, osseous deformity or, most frequently, bone fracture; rarely, GSS may be asymptomatic until late stages. Some related complications are respiratory dysfunction secondary to pleural effusion, chylothorax, osteomyelitis, and spinal cord lesions associated with vertebral bone involvement.1,2
Laboratory findings are almost always within normal limits, although alkaline phosphatase levels may be elevated. Imaging is usually the main diagnostic tool. Radiography initially reveals osteoporosis, followed by progressive fragmentation leading eventually to the entire loss of cortical bone in the late period. Computed tomography (CT) and MRI also demonstrate these findings in addition to diffuse atrophy of adjacent muscles owing to bone resorption.2,3
Histopathological findings of GSS are nonmalignant hyperproliferation of small vascular structures and progressive bone resorption.4 The differential diagnosis includes hereditary multicentric osteolysis, osteolysis due to other diseases such as malignancy, hyperparathyroidism, syringomyelia, and tabes dorsalis.2
Treatment options include radiotherapy, alpha 2b interferon, supportive nutrition and bisphosphonates.1,2 Surgery, consisting of resection of the affected area and bone graft placement is another therapeutic approach.4
CONCLUSION
Gorham-Stout syndrome is a rare entity whose diagnosis is usually overlooked, leading to delays in therapy. It should be considered, especially in the evaluation of osteolytic lesions in typical locations. Although imaging plays an important role in GSS diagnosis, definitive diagnosis may be achieved by excluding other osteolytic causes in suspected cases.
REFERENCES
- Deveci M., Inan N, Corapçıoğlu F, et al. Gorham-Stout syndrome with chylothorax in a six-year-old boy. Indian J Pediatr. 2011;78(6):737-739.
- Nikolaou VS, Chytas D, Korres D, et al. Vanishing bone disease (Gorham-Stout syndrome): A review of a rare entity. World J Orthop. 2014;18;(5):694-698.
- Jindal M, Garg K. Vanishing bone tumor (Gorham-Stout syndrome): A case report. Translational Science of Rare Diseases. 2017;2(1-2):73-76.
- Radhakrishnan K, Rockson SG. Gorham’s disease. Annals of the New York Academy of Sciences. 2008;1131(1):203-205.
Citation
P TAÇ, M O, A H, H C. Gorham-Stout Syndrome. Appl Radiol. 2021;(2):36-37.
March 11, 2021