Heroin-induced toxic leukoencephalopathy
Images
CASE SUMMARY
A 64-year-old normotensive female with a history of inhaled heroin use was brought to the emergency department with the chief complaint of altered mental status. Clinical examination was not significant except for confusion. Admitting urine toxicology demonstrated high level of opioids. After 5 days, patient developed seizures and was intubated. Clinical neurological examination revealed weakness of the left upper limb, with a power of 0/5. Initial and repeat CT scan of the brain without contrast and MRI scan of the brain without contrast were obtained during the patient’s hospital stay.
IMAGING FINDINGS
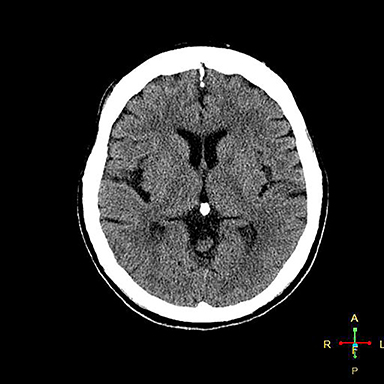
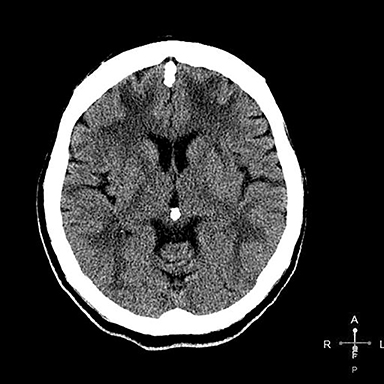
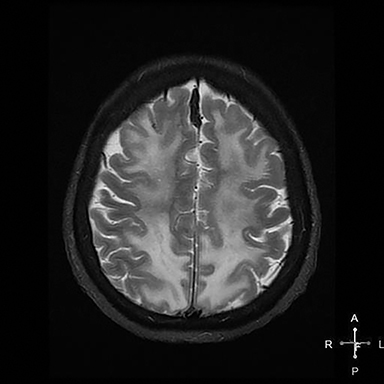
An initial CT scan of the brain (Figure 1) in the emergency department was negative. A repeat CT scan of the brain (Figure 2) on day 5 demonstrated development of extensive white matter abnormality predominantly within the frontoparietal lobes of the cerebrum bilaterally with mild white matter abnormality within the occipital lobes and left cerebellar hemisphere. There was no evidence of acute hemorrhage or mass effect and there was relative sparing of the basal ganglia, internal capsules, brain stem and the gray matter. The MRI examination of the brain (Figure 3) on day 7 demonstrated signal abnormality within the periventricular white matter, deep white matter, and subcortical white matter of the predominately frontoparietal lobes bilaterally, mild signal abnormality occipital lobes bilaterally and subtle signal abnormality within the white matter of the left cerebellar hemisphere.
DIAGNOSIS
Heroin-induced toxic leukoencephalopathy.
Differential diagnoses: Global hypoxic/ischemic insult, cerebral vasculopathy, posterior reversible encephalopathy syndrome (PRES), hypoglycemic encephalopathy, progressive multifocal leukoencephalopathy (PML) and acute disseminated encephalomyelitis (ADEM).
DISCUSSION
Toxic leukoencephalopathy refers to progressive damage of the white matter of the brain, particularly myelin. There are many causes, such as drugs of abuse, environmental toxins and chemotherapeutic drugs. The signs and symptoms of disease range from inattention, forgetfulness and changes in personality to dysarthria, ataxia, dementia, coma and even death.1 Drugs of abuse like toluene, ethanol, cocaine, methylenedioxymethamphetamine (MDMA or “ecstasy”) and heroin have been associated with toxic leukoencephalopathies.1 Toxic exposure from heroin-induced leukoencephalopathy often involves bilateral symmetric damage to cerebellar white matter, posterior cerebral white matter; typically occipital lobe, posterior limb of internal capsule and cerebellar peduncles.2
Drug abuse and addiction has become a main public health problem that affects all societies.3 Heroin, which remains the top drug of concern, rapidly penetrates the blood-brain barrier of the central nervous system and can cause a rare condition called toxic leukoencephalopathy or toxic spongiform leukoencephalopathy. Some investigators have hypothesized that the neurotoxicity of heroin may be due to contamination by or addition of another substance.4,5 In our patient, it is not clear whether heroin was contaminated. Nevertheless, a study5 failed to clearly identify a neurotoxic contaminant or additive in the heroin users responsible for the inflicted white matter damage.
Most of the available literature regarding imaging of neurotoxic changes induced by inhalation of heroin involved predominately the cerebellum, occipital lobes, posterior limb internal capsule and brainstem; however, our patient presented with the lesser known imaging finding of predominate involvement of the frontoparietal lobes.4,6-13
CONCLUSION
The MR imaging findings of heroin-induced toxic leukoencephalopathy in our patient are lesser known, with predominant involvement of the frontoparietal lobes rather than the posterior limb internal capsules, occipital lobes, cerebellum or brainstem. Recent studies have described an imaging presentation similar to our patient and it is important to consider the diagnosis of toxic leukoencephalopathy even when the more common areas of involvement are spared.
REFERENCES
- Filley CM, Kleinschmidt-DeMasters BK. Toxic leukoencephalopathy. N Engl J Med. 2001; 345:425-432.
- Hagel J, Andrews G, Vertinsky T, Heran MK, Keogh C. “Chasing the dragon” - Imaging of heroin inhalation leukoencephalopathy. Can Assoc of Radiol J. 2005;56(4):199-203. Review.
- Jordan MT, Bryant SM, Aks SE, et al. A five-year review of the medical outcome of heroin body stuffers. J Emerg Med. 2009; 36(3):250–256.
- Keogh CF, Andrews GT, Spacey SD, et al. Neuroimaging features of heroin inhalation toxicity: “chasing the dragon.” AJR Am J Roentgenol. 2003; 180:847–850.
- Wolters EC, van Wijngaarden GK, Stam FC, et al. Leucoencephalopathy after inhaling “heroin” pyrolysate. Lancet. 1982; 2:1233–1237.
- Chen CY, Lee KW, Lee CC, et al. Heroin-induced spongiform leukoencephalopathy: value of diffusion MR imaging. J Comput Assist Tomogr. 2000; 24:735–737.
- Gacouin A, Lavoue S, Signouret T, et al. Reversible spongiform leucoencephalopathy after inhalation of heated heroin. Intensive Care Med. 2003; 29:1012–1015. Epub 2003 Mar 14.
- Kriegstein AR, Shungu DC, Millar WS, et al. Leukoencephalopathy and raised brain lactate from heroin vapor inhalation (“chasing the dragon”). Neurology. 1999; 53:1765–1773.
- Offiah C, Hall E. Heroin-induced leukoenceph-alopathy: characterization using MRI, diffusion-weighted imaging, and MR spectroscopy. Clin Radiol. 2008; 63:146–152.
- Chang WC, Lo CP, Kao HW, et al. MRI features of spongiform leukoencephalopathy following heroin inhalation. Neurology. 2006; 67:504.
- Vella S, Kreis R, Lovblad KO, Steinlin M. Acute leukoencephalopathy after inhalation of a single dose of heroin. Neuropediatrics. 2003; 34(2):100-104.
- Havé L, Drouet A, Lamboley JL, Cotton F, St-Pierre G, Quesnel L, Guilloton L, Felten D. [Toxic leucoencephalopathy after use of sniffed heroin, an unrecognized form of beneficial evolution]. Rev Neurol (Paris). 2012; 168(1):57-64.
- Blasel S, Hattingen E, Adelmann M, Nichtweiß M, Zanella F, Weidauer S. Toxic leukoencephalopathy after heroin abuse without heroin vapor inhalation: MR imaging and clinical features in three patients. Clin Neuroradiol. 2010 Mar;20(1):48-53.
Citation
KD L, M Y, TR J. Heroin-induced toxic leukoencephalopathy. Appl Radiol. 2016;(3):36-37.
March 2, 2016