Hot Topics in Imaging Informatics: As Discussed by a Roundtable of Experts
Images





In May 2008 I served as the moderator of a roundtable discussion on imaging informatics-one of the hottest topics in diagnostic imaging. The roundtable, which brought together a distinguished panel of experts, was held in conjunction with the annual meeting of the Society for Imaging Informatics in Medicine in Seattle, WA. The information from this roundtable has been published as this special supplement to Applied Radiology.
Imaging informatics is having a major impact on all of our practices and, in my opinion, is a driving force in the future of diagnostic imaging. In planning for the roundtable, we chose topics that were important, practical, and, at times, controversial.
In an article about re-engineering radiology for an electronic world, Dr. Paul Chang from the University of Chicago focuses on how we can avoid having radiology services become a commodity and the importance of using imaging technology to provide added value to our customers.
Dr. Paul Nagy from the University of Maryland delves into the use of informatics to improve the quality of radiology. He points out that if we're not careful, quality can fall by the wayside as we transition from film-based to digital imaging.
Dr. Khan Siddiqui recently left the University of Maryland to begin work on healthcare informatics with Microsoft. In his article, he discusses advanced visualization-what it is, how its role is changing, and why it has become such an integral and important part of image interpretation. He also offers advice on how to choose the best possible system for your practice.
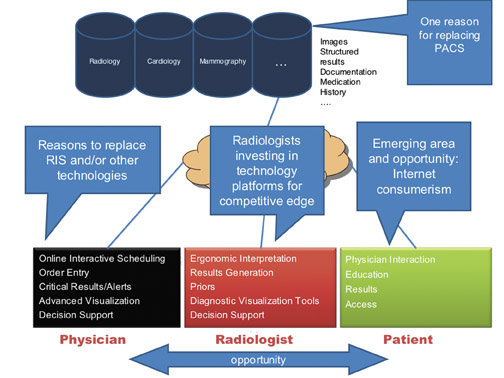
Although some radiologists have only recently purchased their first picture archiving and communications systems (PACS), many have been through several different PACS over the last 15 years. Dr. Steven Horii from the University of Pennsylvania describes how difficult and painful the addition of a PACS or the transition from one PACS to another can be, and offers frank "prenuptial" and "postnuptial" advice on how to minimize the disruption to patient care.
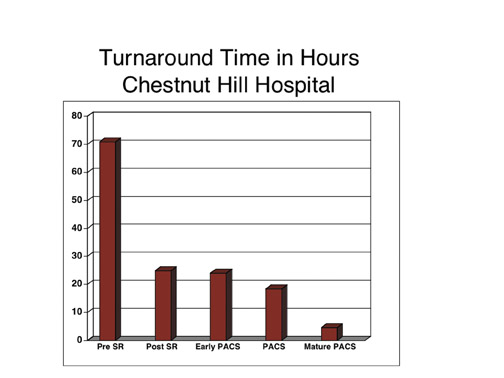
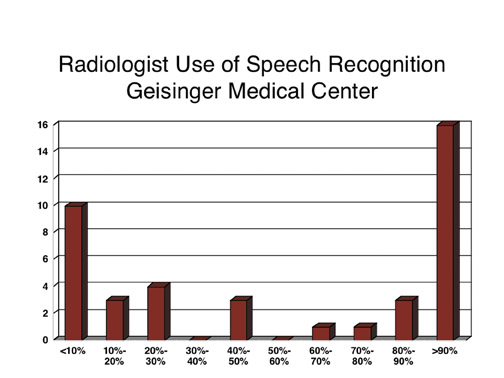
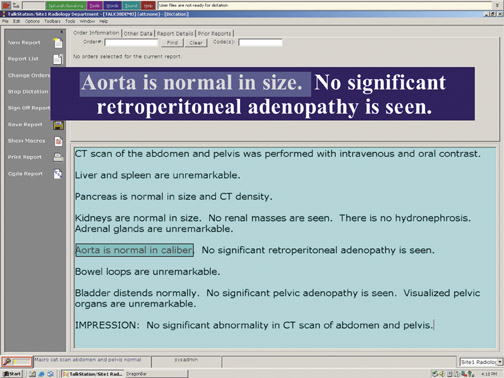
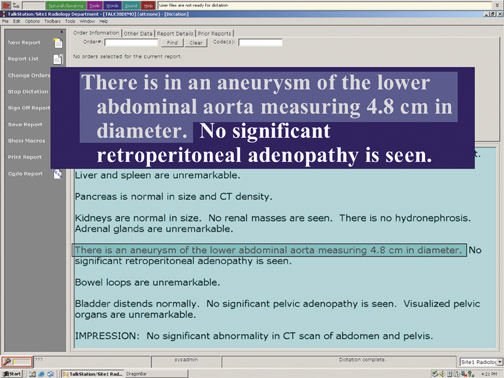
Dr. David Weiss from the Geisinger Health System weighs in on the pros and cons of speech recognition systems. Currently more than half of academic radiology departments across the country use speech recognition technology. However, its adoption has been controversial and the results mixed. Dr. Weiss describes how to get the most out of speech recognition systems.
Finally, Chris Hafey of Vital Images offers a vendor's perspective on the key steps to enterprise-wide advanced visualization, while Robert Cooke of FUJIFILM Medical Systems USA explores how the Internet is revolutionizing radiology.
It has been my distinct pleasure to work with such a distinguished panel of experts. I would like to thank Vital Images and FUJIFILM for sponsoring the roundtable, Anderson Publishing for producing this special supplement, and all of the roundtable participants for providing thoughtful advice and practical tips on how to use imaging informatics to improve the quality and efficiency of radiology services.
Dr. Chang is a Professor and Vice-Chairman, Radiology Informatics, and Medical Director, Pathology Informatics, University of Chicago Pritzker School of Medicine, and the Medical Director, Enterprise Imaging, for the University of Chicago Hospitals, Chicago, IL.
In radiology informatics and information technology (IT), we are constantly challenged to provide a sustainable infrastructure that supports the needs of the radiology department and enables imaging throughout the healthcare enterprise. In the early days, many of us thought that radiology informatics was defined merely by digital image management and its promise to eliminate X-ray film. Once we accomplished that goal, we realized that optimization of workflow was even more important.
Too often, electronic practice tools are viewed as turnkey solutions. In reality, installation of a picture archiving and communication system (PACS) or a speech recognition system will not fix a "broken" radiology practice. The improper application of electronic-based systems can make deficiencies in workflow even more glaring. Unless we are willing to dramatically re-engineer the radiology department and our own attitudes and practices, we will not only fail to successfully leverage and exploit these advanced imaging tools, we may threaten the perceived value of radiology and participate in its marginalization or commoditization.
From a strategic perspective, our true goal is to build a technology infrastructure that ensures the relevance and value of radiologists in taking care of patients. Those of us in informatics and IT need to incorporate into our strategic planning a view of radiologists asvalue innovators.
Value innovation
The concept of value innovation was first introduced by Michael Porter in his 1985 book, Competitive Advantage: Creating and Sustaining Superior Performance . 1 Value innovation is the never-ending task of re-examining what we provide that is of value to our customers. We must always ask ourselves: Are we relevant? Do we add value? And we must continuously re-engineer our workflow and our attitudes to add that value.
In a modern economy, there are 2 ways to compete. If your product or service is perceived as a commodity-that is, undifferentiated from competing products or services-the only legitimate basis on which to compete is price. Toilet paper, for example, is a commodity.
Another way to compete is to provide a product or service that is perceived as having additional value that can be differentiated when compared with other products and services. An iPod (Apple Inc., Cupertino, CA), for example, is perceived to have more value than other MP3 players.
The question is, as radiologists, are we providing a commodity that can be out-sourced anywhere or are we providing true value? The answer depends on how we see ourselves and what kinds of service we provide. In arriving at that answer, it is important to ask customers what is important to them and how well we're succeeding in meeting those needs.
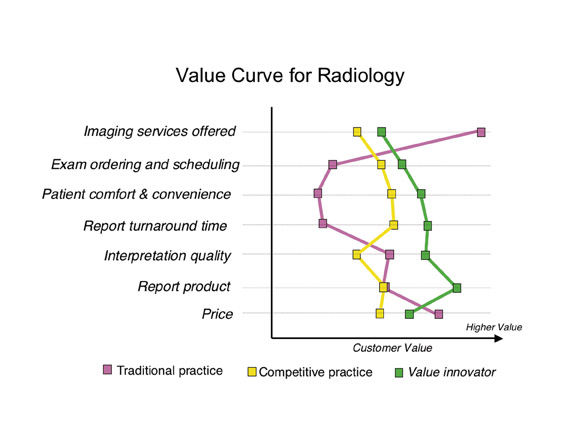
Once we have defined those axes of value, it is possible to plot a value curve. Figure 1 shows value curves for 3 different types of radiology practices. 2 The value curve for a typical academic radiology practice shows very high value in the number of imaging services provided. However, academic practices tend to fall short when it comes to other components that are valued by customers, such as examination ordering and patient comfort.
The services provided by a competitive, successful community-based practice are quite different from those provided by an academic practice, and they result in a characteristic value curve that is also different. The "competitive" practice may not deliver as many imaging services, but it excels in services that are perceived as being of value to the customer, including examination ordering and scheduling, patient comfort and convenience, and report turnaround time.
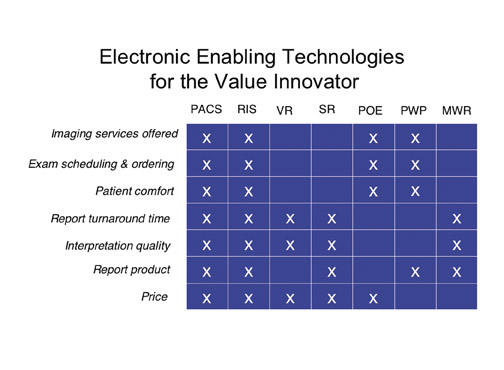
True value innovators go even further, identifying where they are on the value curve, where they want to be, and the gaps in between. Then, and only then, do they acquire technology that best suits and addresses those gaps, whether it be PACS, teleradiology, a radiology information system (RIS), voice recognition, structured reporting, Web-based physician order entry, multimedia Web reports, or patient Web portals(Figure 2).
The iPod effect
Before identifying gaps in value, it is important to understand who the customer is. In the context of radiology, our customers are our referring physicians and, ultimately, our patients. Today, patients are active health consumers, and, like other consumers, their characteristics have changed over the last 10 to 15 years. Let's call it the iPod effect.
From functional point of view, the iPod could be considered an inferior product. For example, it doesn't come equipped with FM radio, and it locks users into a particular application, iTunes. Yet the totality of the experience is viewed as seamless, attractive, and very positive. The reason the iPod is successful is that it addresses 3 major drivers of the modern-day consumer-characteristics that drive our modern-day healthcare consumer as well.
The first driver of the iPod effect is real-time delivery, or "I want it now." In the past, if customers ordered a music CD and received it in the mail a few days later, they were happy. Then it became possible to place an online order before midnight and receive the CD by express delivery the next day. Now, we can go to iTunes and download music onto the iPod immediately. Real-time delivery of service and product is a critical driver and one of the reasons the iPod has been so successful.
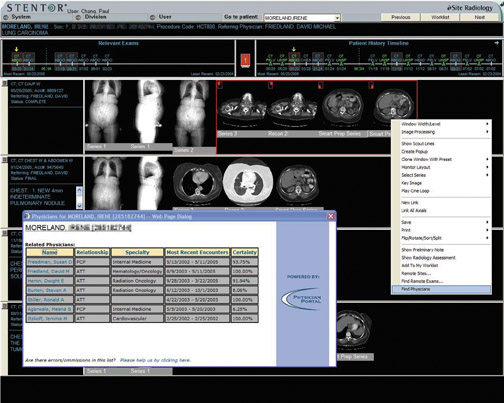
When it comes to medical care, that same expectation is valid. Many of us in hospital-based radiology practices have confronted the increasing demand to provide same-day service. A patient comes in in the morning for a magnetic resonance imaging (MRI) study or a positron emission tomography/computed tomography (PET/CT) scan, and the patient wants the interpretation in his or her oncologist's hands that afternoon, so therapy can begin immediately (Figure 3). Clearly, the drive for real-time delivery of service is going to continue and is one of the reasons certain technologies such as speech recognition have become so important.
The second iPod characteristic is no-compromise service. From the elegant interface to the seamless integration with an industry-leading, comprehensive iTunes library, the iPod offers users a listening experience that is without peer.
In healthcare, patients have developed similar expectations. In the past, there was an asymmetrical distribution of healthcare information-that is, the doctor always knew more than the patient. This is no longer the case. Who is more motivated to know everything about a disease than the person who has the disease? With the resources available on the Web, many patients are extremely knowledgeable. After all that research, they want optimized, no-compromise service. As a result, we can no longer differentiate ourselves as physicians who add value by simply knowing more than our patients. Instead, we must take on the role of consultant and manager, becoming the person who helps shepherd the patient through a complex process. Patients will no longer settle for second-best.
The last driver is personalized service. With the iPod, we can select our own music. We no longer have to listen to someone else's selection on the radio. With amazing advances in genetics and proteomics, physicians will be able to provide customized therapy for patients. That same driver is going to be relevant in radiology. For example, optimized image protocols that are tailored to the specific patient will require much more capable integration of information systems.
Information throughput
Another major driver in radiology is the concept of pay for performance, or "no outcome-no income." Can radiologists successfully play this game? I believe we can. However, critical requirements for success will include massive improvements in efficiency, productivity, and cost-effectiveness-in other words, optimized information throughput.
Electronic-based technology and informatics can be important enablers of value innovation, if we're willing to re-engineer our processes. When it comes to improving efficiency in information throughput, we must go beyond such simple measures as enhancing patient throughput or reducing report turnaround time.
The turnaround time that really matters encompasses the entire service chain. It spans from the time a physician decides to order a study to the time at which information is available from that study to help the clinician create a patient management plan. To truly improve turnaround time, we must re-evaluate examination ordering and scheduling, patient registration, examination acquisition, examination interpretation, report authoring, and report delivery.
Collaboration
It is clear that we must do away with film and paper. Instead, we must embrace electronic-based informatics systems. To do this, we need much better integration of electronic information systems and modalities within those systems. To date, a lack of integration is one ofvendors' biggest failures.
Time-motion studies repeatedly show that technologists waste too much time typing information from one electronic system to another. We also need greater integration in communicating context. It makes no sense for technologists to have to tell a RIS that they have completed a study. "Performed procedure" steps and other kinds of technology can do that automatically.
In addition, we will need to make major improvements in how we communicate. Simply sending out reports in a timely fashion willno longer be adequate. We must be much more engaged and collaborative.
In considering the difference between communication and collaboration in radiology, it is useful to think about the evolution of the Web. Radiologists typically use a PACS the way people used an old-fashioned Web 1.0 application. We sit in a dark room, and information orimages come to us. Our clinicians are not interacting with us, and we're not collaborating with them. This is one reason radiology can be easily commoditized and marginalized.
Today, kids don't use the Web to passively receive information in isolation from one another. They use such applications as Skype (SkypeTechnologies, Luxembourg), instant messaging, MySpace (MySpace, Inc., Los Angeles, CA), and YouTube (YouTube, LLC, San Bruno, CA) to foster virtual collaboration and active participation.
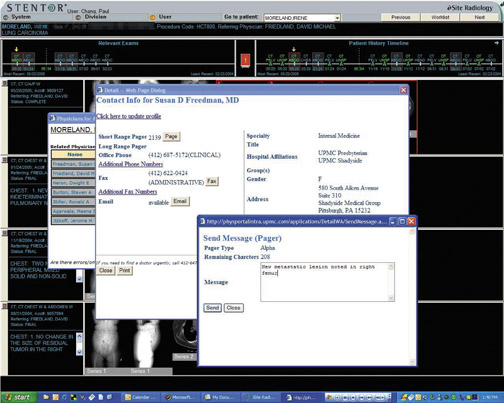
Radiologists and vendors must re-evaluate applications from this Web 2.0 perspective, re-engineering them in a way that fosters collaboration with clinicians (Figure 4). The goal is to match the appropriate communication method to a specific clinical context. Messaging, Web conferencing, multimedia reports, and other electronic communication models can all be very helpful.
Conclusion
Radiology must be willing to continuously re-engineer and reinvent itself to fully exploit electronic technology. Information systems canplay a significant role in helping radiologists to evolve from being simple providers of information to true collaborators. If we choose to make this transition, we will avoid being marginalized and commoditized. Instead, we will be able to show that we add true value to patient care.
REFERENCES
- Porter ME. Competitive Advantage: Creating and Sustaining Superior Performance . New York, NY: Free Press; 1985.
- Schomer DF, Schomer BG, Chang PJ. Value innovation in the radiology practice. RadioGraphics . 2001;21:1019-1024.
Roundtable Discussion following the presentation:
Re-engineering radiology in an electronic world: The radiologist as value innovator
Paul J. Chang, MD
ELIOT L. SIEGEL, MD: Paul, that was a wonderful kick-off to our roundtable discussion, and you raised some really interesting points. It reminded me that prior to going digital, in a film-based environment, we provided a lot of services that we don't really provide now. Radiology was the epicenter of the hospital for discussion of interesting patients and their imaging studies. As a radiologist, I felt very much more my role as educator than I do today, and I felt more directly involved with patient care than I do today. As time goes on, there's a tendency, while trying to maximize productivity, to try to sit in front of a workstation and just bang out the cases without adding that additional value that you mentioned. So I'm really excited about the potential for us to use our digital and electronic tools for more than just diagnosis and reporting and to be able to use them to significantly improve our ability to provide that added value.
You talked about commoditizatio and used the example of the superstore Wal-Mart as a metaphor for commoditization of products in general that has a negative connotation. In many ways, however, Wal-Mart has served as a groundbreaking innovator. Wal-Mart was one of the first companies to use bar coding and electronic check-out and to provide a very wide variety of different services such as optometry, its $4 generic drug pricing, groceries, and pharmacies, all in a single venue. When I walk into Wal-Mart, a greeter says hello and asks me how I'm feelingt oday, something we don't do in our imaging department. Isn't it true that commoditization isn't necessarily antithetical to innovation and personalized services?
I wonder as we move toward providing all of these sophisticated and wonderful additional services that you describe, whether or not we will have to consolidate our practices in order to support a more sophisticated and complex IT infrastructure. As time has gone on, the trend has, indeed, been toward larger and more sophisticated radiology practices with more sophisticated IT capabilities. While I think it is absolutely essential, as you point out, to the future success of radiology, do you think that this effort to add value will decrease the number of "boutique" smaller radiology practices and move us in the direction of larger, more"commoditized" practices?
PAUL J. CHANG, MD: Eliot, your aise a very good point, and you're absolutely right: Wal-Mart adds a lot of innovation. An important reality we in radiology attempt to deny is that in any economic system, any market, any economy, there are winners and there have to be losers. Wal-Mart is definitely a winner in today's economy. However, you can't have winners without losers. We try to say that if we all provide "adequate" service, if we all isolate ourselves, and if we all create antimarket barriers, then we can all do our thing and "survive." However, now that medical images can be delivered at the speed of light, the 3 drivers I mentioned are in play; our customers are now health consumers that can do their due diligence. If we are not providing timely service, not providing world-class advanced visualization, and not providing added value, then we're not providing the kind of service the customer can get across the street, if not across the world. In that situation, we will have an environment in which there will be winners and losers.
If we follow the Wal-Mart model, radiology becomes a commodity. In that case,it doesn't matter whether or not your advanced visualization is done in India, Australia, Israel, or across the world. If Icould look into my crystal ball, I think we'd see some consolidation through which a lot of services will be provided that way, because people will determine that the value provided by such services is sufficient. But I believe you will have an alternative and potentially more attractive opportunity if you offer high value boutique or niche practices with or without consolidation. These practices will provide value-added services with respect to advanced visualization or advanced expertise and evaluation.
I am absolutely convinced that with technology such as the Internet, as we move from analog to digital, the artificial barriers that sustained mediocrity are going away. So there will be losers. I would rather be a winner than a loser. Whether that winning strategy is to consolidate and provide a Wal-Mart-typec ommoditization is a question. That's a valid approach; some people are very successful at it, and some customers are content with the service provided.
From a very selfish perspective as a radiologist, I like it when docs come to the reading room for a consultation: Ir eally feel part of the patient care team. I think it's the most satisfying part of our day. I believe there will be a role for a more optimized boutique of approaches to service in radiology that avoids the Wal-Mart model as a more value-driven proposition.
PAUL G. NAGY, PhD: I really like the concept of an educated and motivated patient. I think that provides us with enormous opportunities in radiology, but also presents us with a challenge. We need t ofigure out what our role will be in terms of direct contact with the patient. The University of Pennsylvania has created a unique initiative through which they're beginning to send the reports directly to the patients. As that speeds up in realtime, how is that going to present us with challenges with referring physicians?
CHANG: It is a challenge. One of the people in our field, Dr. Leonard Berlin,has really thought and written a lot about our role as radiologists. As you mentioned, Paul, our traditional role was as the "physician's physician" in the sense that the interpretation of our studies should be exclusively presented to the referring physician and that this physician would present the results, good and bad, to their patients. Dr. Berlin has raised some issues about that in that quality is important, timeliness is important, and, oh by the way, we're physicians too.Should we not start being more proactive and more directly interactive with our patients? I can see it both ways. In myo wn practice, I like to talk to the patients. I feel that it's the best way to be engaged and to remind ourselves that we're not just sitting around in a dark reading room looking at cases. We need to rememberthat what we do impacts patient care.
The challenge, as you mentioned, is that we also don't want to create a problem with our collaborative spirit with our ordering physicians. There is a mechanism for that and that's always been communication. I believe radiologists should communicate often-not just with reports, but in the tumor board and in daily conferences, which necessarily don't have to be synchronous. One of the big opportunities of electronic systems is that they allow us to have reliable and rich asynchronous collaborations. Eliot, I know you've been on wikis and blogs, and these are mechanisms by which asynchronously one can create a community of interaction. It is crucial for radiologists to improve our communication so that we are viewed as true collaborators with our clinicians, and are seen working together to determine the best mechanism to deliver information jointly to patients.
The great model for this is to look at what our colleagues do in breast imaging. They have come up with a balance in that they communicate directly with the patient, they examine the patient, and they work very closely with the surgeons and oncologists. Now the challenge of informatics is they do that at the expense of efficiency because they typically use manual processes, and a lot of people are involved.
One of the challenges to the informatics community is to try to take the spirit of what they've accomplished with true collaboration, not only with their patient sbut also the referring physicians, and make it so it's more efficient and sustainable by embracing electronic based potentially asynchronous mechanisms.
DAVID L. WEISS, MD: Expandingo n that, Paul, you mentioned there's a need for multidirectional, real-time collaborative communication. I think everyone agrees with that. It's my feeling that many RIS products have failed in providing information services that radiologists need. A number of PACS have failed in providing the "C" for communication,and we're left with disparate software. We have one vendor for our reporting, another company for critical results communication, another couple of vendors for decision support, and another for teaching file software. It would be nice to have all of these integrated under one umbrella. What umbrella do you see best for encompassing all of these into one system?
CHANG: Well, I'm very biased about this. I think it is unrealistic to expect a RIS or PACS to be all things to all people. In fact, the analogy I like to use is audio components: you don't buy everything from one vendor because no one vendor can make the best speakers, the best amplifier, and the best blue-ray player. You buy the best component and take advantage of the fact that these components will interoperate.
I don't actually know what a RIS is anymore. Vendors, attempting to respond to our demands for improved functionality, have added increased functions that go well beyond the traditional definition of a RIS. The RIS has "become anything you want it to be." So the definition of RIS has become something that is very difficult for me to understand or grasp.
It's the same thing with the PACS. That's why you hear things about "RISdriven" workflow or "PACS-driven"workflow. I get a bit confused by these terms. Instead, we should say that in order to support complex workflow, we have a lot of services that we need. The key is interoperability. There's nothing wrong with having a separate vendor that does speech recognition, communicatio nof services, or alerts; we don't necessarily need a RIS or PACS to provide these services. What's wrong today is that these services don't talk to each other. Idon't think the solution is to expect our PACS vendor or RIS vendors to suddenly expand their portfolio of services, because the more they go away from their core competency, the less likely they are to be able to accomplish these critical services correctly.
What we really need is improved interoperability. There are a lot of strategies, and Paul is an expert in what we can do toa ccomplish this kind of interoperability. There are initiatives: Integrating theH ealth Care Enterprise (IHE), service-oriented architecture (SOA). There are a lot of different mechanisms or strategies one might use to address the issue of interoperability. But, Dave, to answer your question, I think the real issue is not that the RIS or the PACS aren't doing enough. The issue is that the pieces are there, they're just not talking together.
The real push is to get our vendors to embrace interoperability, either through approaches such as IHE or SOA or to have another vendor entity that offers expertise in how to integrate. If you look at industries outside of medicine, that'swhat they've done. I believe interoperability will be the key driving requirement for the next decade in our field.
SIEGEL: Thanks, Paul.
Dr. Nagy is an Associate Professor, Director of Quality and Informatics Research, Department of Radiology, University of Maryland School of Medicine, Baltimore, MD.
One of the roles of an informatics architect is to provide an infrastructure that enables radiologists to read images immediately whereverthey are. Such rapid access to digital imaging reduces delays in interpretation, speeds report turnaround time, and hastens clinical decision-making, all of which clearly improve efficiency.
Over the years, however, it has become equally clear that an accelerated work pace, a focus on productivity, and the use of distance medicine can sterilize work relationships. When a technologist no longer comes into the reading room to hang films, something gets lost in the relationship between radiologist and technologist. When referring physicians no longer engage the radiologist in consultations, something gets lost in that relationship too. These changes threaten to compromise quality.
In our desire to leverage information technology (IT) to be as productive as possible, we have threatened our work relationships. This does-n't need to be so. Essentially, IT was born to communicate, whether by voicemail, e-mail, text messaging, instant messaging, or paging. We can do a better job of using some of these communication vehicles to create a culture of quality within radiology-to make it easier to do the right thing while being as productive as possible. This article will discuss 3 tools we have developed at the University of Maryland to enhance quality through informatics.
Quality-control reporting
The first challenge many radiology practices face when they "go digital" is incorporating the quality-control practices that were used in the film environment. In the past, radiologists could note on the film if the images were poorly collimated or were substandard in some otherway. In an electronic environment, there is little feedback between radiologists and technologists.
The result can be a downward spiral in quality. Often, radiologists submit quality-control reports using the same paper-based forms they were using years ago. The reports go to modality supervisors, who discuss them with the technologists. But the radiologists typically don't receive any feedback on actions taken and don't observe any improvement. As a result, it is difficult for radiologists to see the value in submitting future quality-control reports.
Once radiologists become apathetic about reporting quality issues, many things can go awry. If technologists don't get feedback on the quality of their work, they are likely to either think they're doing a great job or that radiologists in their institution don't care about image quality. Radiology supervisors may know that radiologists are unhappy, but they have no data to use in taking action. The result is a disappointing stalemate.
Information technology systems must be able to handle communications feedback to ensure quality processes. The key ingredients for change at the University of Maryland were a picture archiving and communications system (PACS) and a simple Web-based issue tracking tool that enables radiologists to submit quality-control issues, assigns issues to owners, and notifies users when the issue has been resolved. We also supplied our technologists and modality supervisors with digital pagers. When a radiologist reports a quality issue, the system pages the technologist and modality supervisor immediately.
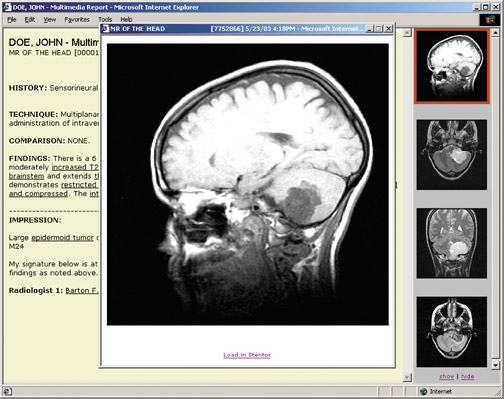
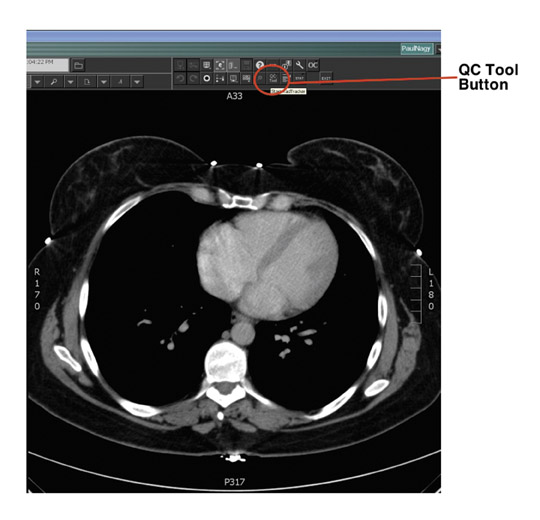
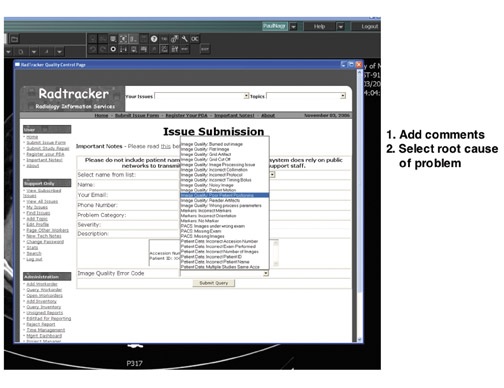
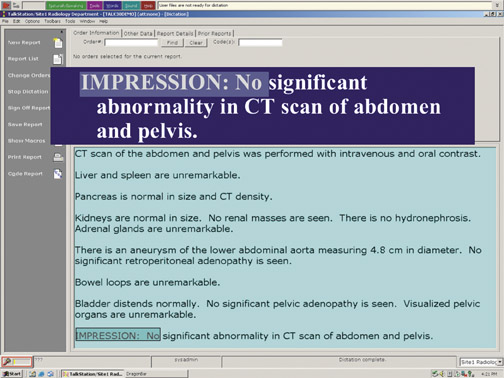
To encourage radiologists to report quality issues, it is important to remove as many barriers as possible and to make reporting simple. With this in mind, we synchronized quality control with our clinical workflow by adding a button to our PACS that launches a Web-based quality-control tool called Radtracker 1 (Figure 1).
The issue-submission Web page provides the user name, the study session number, the patient medical record number, and the modality. Within a single pull-down menu, the radiologist can select what is wrong with the images-poor patient positioning, for example-and can add comments. When the radiologist clicks on "submit," the modality supervisor and technologist receive a text message about the issue and how to correct it. The technologist then resolves the issue, and the radiologist receives an e-mail about actions taken.
Using this system, we have gone from approximately 5 to 10 paper-based quality-control reports per month in 2006 to 300 per month today. This does not reflect deterioration in quality; in fact, only roughly 1% of our annual volume of studies has a quality-control issue. Instead, better quality-control reporting has enabled us to focus on the root cause of quality-control issues and to track how quickly we respond to these issues. In approximately 40% of cases, we resolve the issue within an hour.
We have also uncovered new types of quality issues, beyond those related to image acquisition. Data quality issues can affect the radiologist's workflow. For example, if the technologist doesn't sign off and complete a study in time, the radiologist might not be able to finalize it. Using this process, we're better able to understand problem areas in the department.
We have used the quality-control data to create knowledge bases that we can click through and explore. When we do in-service training,we use the knowledge bases to find various types of cases. Using URL-based integration, we can even launch the PACS system simply byclicking on a case file.
Every few months, a radiologist, technologist, modality supervisor, and physicist meet for an hour to work through all of the quality-control issues in a given imaging section. This offers radiologists an ideal opportunity to lead a discussion on how quality-control issues arise. In the past, our modality supervisors were very good at fixing problems on a day-to-day basis but didn't necessarily understand the magnitude of the issue. Now, when they see that a problem is occurring many times a year, they realize it's worth the effort to determine why the problem is happening and how to remove the root causes.
We also use this system for generating report cards (Figure 2). These report cards enable our technologists to see how well they're doing, how many quality reports they're getting from radiologists over a period of time, and how they compare with other technologists. We have found that most technologists are very responsive. Once they see the data, they try to understand how they can do a better job. This is a very powerful tool for creating a culture of quality.
For radiologists, this system provides a mechanism to report quality issues and removes any reason for being apathetic. We now have data-driven discussions with the radiologists to try to understand the root causes of quality issues. The radiologists feel that the technologists are working with them, that we are a team, and that we have a good feedback mechanism and good communication.
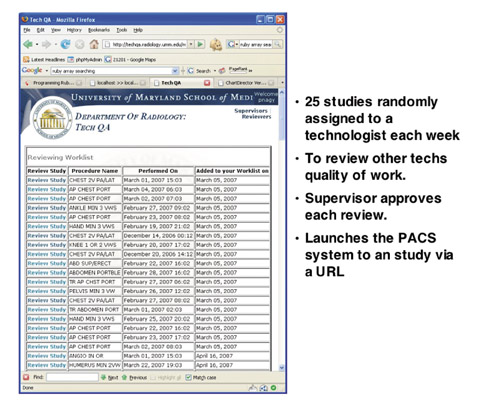
Technologist peer review
The second quality-control tool that we have implemented, technologist peer review, also harkens back to the days of film. Acquiring images has always been an art that requires training and feedback to perfect. In the past, as senior film technologists processed films, they would review images and take junior technologists to task for quality problems. Through peer pressure, junior technologists would be motivated to improve their performance.
Peer pressure is an enormous motivator that we don't use well enough in healthcare to improve performance. At our institution, we use informatics as a tool for applying peer pressure. We no longer have the luxury of doing in-line quality control while processing film. Radiologists need to read images right away and report them immediately. However, we can do retrospective quality control.
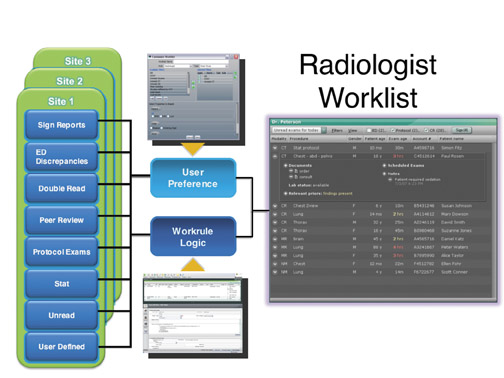
To achieve this goal, we have built a fully automated Web-based Tech Quality Assurance (QA) tool that captures all the studies done by a section, then randomly assigns approximately 5% of them to a volunteer to review (Figure 3). Reviewing technologists are given a worklist with the procedure names and dates. Because of synchronization between information systems, they can launch the study in the PACS system simply by clicking on the integrated URL.
Once the study has been launched, the technologist reviewer rates it on a scale of 1 to 5, with 1 being poor and 5 being excellent. The ratings cover patient positioning, image clarity/artifacts, contrast, annotations, markers, and radiation safety. The reviews are then approved or disapproved by a modality supervisor. This step enables us to train our volunteers to become better reviewers.
We have used this technique to review >5000 studies so far. We have found that we're doing well on contrast, data quality, and annotations, but have room for improvement in markers, positioning, and radiation safety (mostly collimation).
We can also use the Tech QA tool in preparing individual technologist report cards. This is a way of giving very tailored feedback on how to improve their processes. We can also use this tool as a knowledge base to identify the best and worst studies in each section, so thattechnologists can learn by both doing and seeing.
Communication
Communication between radiologists and referring physicians plays another important role in quality. Take the case of a critical finding that warrants rapid communication. The Joint Commission on the Accreditation of Healthcare Organizations (JCAHO) requires that radiologists document not only that a critical finding has been delivered but also how long it took to deliver the finding.
Delivery of critical findings can be especially challenging in a large in-patient medical center. At the University of Maryland, we have roughly 1100 attending physicians and another 900 residents. Often the physician who orders a study is not the right person to take delivery of the critical finding. This is a source of frustration for radiologists.
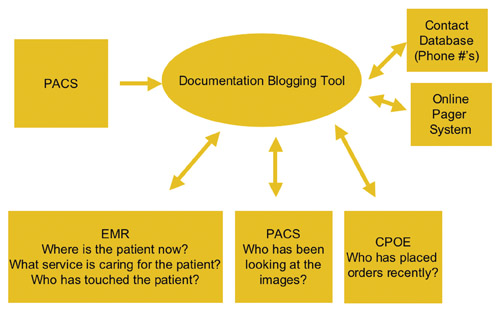
To help in identifying the right person to receive information to critical situations, we have developed data mining tools that identify who is involved in patient care (Figure 4). This tool can perform a real-time query of the electronic medical record to determine where the patient is located and which service team is caring for the patient. Often, it is more important to identify the appropriate service team than to identify the individual physician.
We can also use the critical alert tool to determine who has been in contact with the patient in the last 24 hours. Knowing which physicians and nurses are giving care to the patient offers an important clue in determining to whom to deliver critical information. We can also look atthe PACS to see who has been looking at the images and the computer-based order entry system to see who has been placing physician orders for the patient.
When the radiologists launch the critical alert tool from our PACS, they are presented with all of the patient information and names of clinicians who have been involved in patient care, along with information on how old the contact data are. Once we have all this information, we mine a centralized physician contact database with phone numbers and an integrated online paging system. The radiologist simply clicks on the "contact" button next to each name.
In addition, we have built a blogging tool that can be launched from the PACS and documents all the radiologist's efforts to communicate critical findings, as well as to document that it was successfully delivered, to whom, and when.
Healthcare IT systems are a gold mine of information. If we can provide some of that information in a relevant format to radiologists, it can help them to make decisions and to communicate information quickly in a critical environment.
Conclusion
Communication plays a vital role in how we deliver radiology services and in the quality of those services. Information technology is immensely qualified to deliver tools that improve quality and communications. The time has come for radiologists to insist that vendors provide these tools. PACS stands for picture archiving and communication system. It's time to put the communication back in PACS.
REFERENCE
- Nagy PG, Pierce B, Otto M, Safdar NM. Quality control management and communication between radiologists and technologists. J Am Coll Radiol . 2008;5:759-765.
Dr. Chang is a Professor and Vice-Chairman, Radiology Informatics, and Medical Director, Pathology Informatics, University of Chicago Pritzker School of Medicine, and the Medical Director, Enterprise Imaging, for the University of Chicago Hospitals, Chicago, IL.
In radiology informatics and information technology (IT), we are constantly challenged to provide a sustainable infrastructure that supports the needs of the radiology department and enables imaging throughout the healthcare enterprise. In the early days, many of us thought that radiology informatics was defined merely by digital image management and its promise to eliminate X-ray film. Once we accomplished that goal, we realized that optimization of workflow was even more important.
Too often, electronic practice tools are viewed as turnkey solutions. In reality, installation of a picture archiving and communication system (PACS) or a speech recognition system will not fix a "broken" radiology practice. The improper application of electronic-based systems can make deficiencies in workflow even more glaring. Unless we are willing to dramatically re-engineer the radiology department and our own attitudes and practices, we will not only fail to successfully leverage and exploit these advanced imaging tools, we may threaten the perceived value of radiology and participate in its marginalization or commoditization.
From a strategic perspective, our true goal is to build a technology infrastructure that ensures the relevance and value of radiologists in taking care of patients. Those of us in informatics and IT need to incorporate into our strategic planning a view of radiologists asvalue innovators.
Value innovation
The concept of value innovation was first introduced by Michael Porter in his 1985 book, Competitive Advantage: Creating and Sustaining Superior Performance . 1 Value innovation is the never-ending task of re-examining what we provide that is of value to our customers. We must always ask ourselves: Are we relevant? Do we add value? And we must continuously re-engineer our workflow and our attitudes to add that value.
In a modern economy, there are 2 ways to compete. If your product or service is perceived as a commodity-that is, undifferentiated from competing products or services-the only legitimate basis on which to compete is price. Toilet paper, for example, is a commodity.
Another way to compete is to provide a product or service that is perceived as having additional value that can be differentiated when compared with other products and services. An iPod (Apple Inc., Cupertino, CA), for example, is perceived to have more value than other MP3 players.
The question is, as radiologists, are we providing a commodity that can be out-sourced anywhere or are we providing true value? The answer depends on how we see ourselves and what kinds of service we provide. In arriving at that answer, it is important to ask customers what is important to them and how well we're succeeding in meeting those needs.
Once we have defined those axes of value, it is possible to plot a value curve. Figure 1 shows value curves for 3 different types of radiology practices. 2 The value curve for a typical academic radiology practice shows very high value in the number of imaging services provided. However, academic practices tend to fall short when it comes to other components that are valued by customers, such as examination ordering and patient comfort.
The services provided by a competitive, successful community-based practice are quite different from those provided by an academic practice, and they result in a characteristic value curve that is also different. The "competitive" practice may not deliver as many imaging services, but it excels in services that are perceived as being of value to the customer, including examination ordering and scheduling, patient comfort and convenience, and report turnaround time.
True value innovators go even further, identifying where they are on the value curve, where they want to be, and the gaps in between. Then, and only then, do they acquire technology that best suits and addresses those gaps, whether it be PACS, teleradiology, a radiology information system (RIS), voice recognition, structured reporting, Web-based physician order entry, multimedia Web reports, or patient Web portals(Figure 2).
The iPod effect
Before identifying gaps in value, it is important to understand who the customer is. In the context of radiology, our customers are our referring physicians and, ultimately, our patients. Today, patients are active health consumers, and, like other consumers, their characteristics have changed over the last 10 to 15 years. Let's call it the iPod effect.
From functional point of view, the iPod could be considered an inferior product. For example, it doesn't come equipped with FM radio, and it locks users into a particular application, iTunes. Yet the totality of the experience is viewed as seamless, attractive, and very positive. The reason the iPod is successful is that it addresses 3 major drivers of the modern-day consumer-characteristics that drive our modern-day healthcare consumer as well.
The first driver of the iPod effect is real-time delivery, or "I want it now." In the past, if customers ordered a music CD and received it in the mail a few days later, they were happy. Then it became possible to place an online order before midnight and receive the CD by express delivery the next day. Now, we can go to iTunes and download music onto the iPod immediately. Real-time delivery of service and product is a critical driver and one of the reasons the iPod has been so successful.
When it comes to medical care, that same expectation is valid. Many of us in hospital-based radiology practices have confronted the increasing demand to provide same-day service. A patient comes in in the morning for a magnetic resonance imaging (MRI) study or a positron emission tomography/computed tomography (PET/CT) scan, and the patient wants the interpretation in his or her oncologist's hands that afternoon, so therapy can begin immediately (Figure 3). Clearly, the drive for real-time delivery of service is going to continue and is one of the reasons certain technologies such as speech recognition have become so important.
The second iPod characteristic is no-compromise service. From the elegant interface to the seamless integration with an industry-leading, comprehensive iTunes library, the iPod offers users a listening experience that is without peer.
In healthcare, patients have developed similar expectations. In the past, there was an asymmetrical distribution of healthcare information-that is, the doctor always knew more than the patient. This is no longer the case. Who is more motivated to know everything about a disease than the person who has the disease? With the resources available on the Web, many patients are extremely knowledgeable. After all that research, they want optimized, no-compromise service. As a result, we can no longer differentiate ourselves as physicians who add value by simply knowing more than our patients. Instead, we must take on the role of consultant and manager, becoming the person who helps shepherd the patient through a complex process. Patients will no longer settle for second-best.
The last driver is personalized service. With the iPod, we can select our own music. We no longer have to listen to someone else's selection on the radio. With amazing advances in genetics and proteomics, physicians will be able to provide customized therapy for patients. That same driver is going to be relevant in radiology. For example, optimized image protocols that are tailored to the specific patient will require much more capable integration of information systems.
Information throughput
Another major driver in radiology is the concept of pay for performance, or "no outcome-no income." Can radiologists successfully play this game? I believe we can. However, critical requirements for success will include massive improvements in efficiency, productivity, and cost-effectiveness-in other words, optimized information throughput.
Electronic-based technology and informatics can be important enablers of value innovation, if we're willing to re-engineer our processes. When it comes to improving efficiency in information throughput, we must go beyond such simple measures as enhancing patient throughput or reducing report turnaround time.
The turnaround time that really matters encompasses the entire service chain. It spans from the time a physician decides to order a study to the time at which information is available from that study to help the clinician create a patient management plan. To truly improve turnaround time, we must re-evaluate examination ordering and scheduling, patient registration, examination acquisition, examination interpretation, report authoring, and report delivery.
Collaboration
It is clear that we must do away with film and paper. Instead, we must embrace electronic-based informatics systems. To do this, we need much better integration of electronic information systems and modalities within those systems. To date, a lack of integration is one ofvendors' biggest failures.
Time-motion studies repeatedly show that technologists waste too much time typing information from one electronic system to another. We also need greater integration in communicating context. It makes no sense for technologists to have to tell a RIS that they have completed a study. "Performed procedure" steps and other kinds of technology can do that automatically.
In addition, we will need to make major improvements in how we communicate. Simply sending out reports in a timely fashion willno longer be adequate. We must be much more engaged and collaborative.
In considering the difference between communication and collaboration in radiology, it is useful to think about the evolution of the Web. Radiologists typically use a PACS the way people used an old-fashioned Web 1.0 application. We sit in a dark room, and information orimages come to us. Our clinicians are not interacting with us, and we're not collaborating with them. This is one reason radiology can be easily commoditized and marginalized.
Today, kids don't use the Web to passively receive information in isolation from one another. They use such applications as Skype (SkypeTechnologies, Luxembourg), instant messaging, MySpace (MySpace, Inc., Los Angeles, CA), and YouTube (YouTube, LLC, San Bruno, CA) to foster virtual collaboration and active participation.
Radiologists and vendors must re-evaluate applications from this Web 2.0 perspective, re-engineering them in a way that fosters collaboration with clinicians (Figure 4). The goal is to match the appropriate communication method to a specific clinical context. Messaging, Web conferencing, multimedia reports, and other electronic communication models can all be very helpful.
Conclusion
Radiology must be willing to continuously re-engineer and reinvent itself to fully exploit electronic technology. Information systems canplay a significant role in helping radiologists to evolve from being simple providers of information to true collaborators. If we choose to make this transition, we will avoid being marginalized and commoditized. Instead, we will be able to show that we add true value to patient care.
REFERENCES
- Porter ME. Competitive Advantage: Creating and Sustaining Superior Performance . New York, NY: Free Press; 1985.
- Schomer DF, Schomer BG, Chang PJ. Value innovation in the radiology practice. RadioGraphics . 2001;21:1019-1024.
Roundtable Discussion following the presentation:
Using informatics to improve the quality of radiology
Paul G. Nagy, PhD
ELIOT L. SIEGEL, MD: Thanks, Paul. That was really an excellent presentation. You have a talented and sophisticated information technology operation in the department of radiology at the University of Maryland and consequently have the good fortune to have access to all of these. But many of the people who will be reading this may not have that same level of expertise in thei rpractices. So if others wanted to create a level of functionality that in some ways paralleled what you've described, how would they get that? Should they talk to their PACS vendor or RIS vendor? Or find a third party? Or should they hire the best and brightest IT folks for their own department? How would you recommend that someone proceed who wants to take advantage of all the wonderful potential that you talked about?
PAUL G. NAGY, PhD: Well, I think it's the responsibility of academic institutions to explore new technologies and to evaluate their effectiveness for radiology practices. So it's our responsibility to be able use these types of tools and determine whether they make sense andif they're actually valuable to clinical practice. A lot of times it's a failure of imagination; it's very hard to know what to ask for if you haven't seen it before. Intrying to demonstrate these tools, prototype them, and evaluate them, I hope we are shaping the conversation of what users and customers can ask for. You should be asking your existing vendors for these tools. Their job is to help you use informatics to enable your job. Ithink that conversation is how most of our economy works, in that it creates an environment in which enough people ask the vendors for these tools. Then marketing people get all excited because they're losing a competitive advantage or they see this as a differentiator, which several vendors do now. As the PACS marketplace fills up, they're going to be looking for these advantages and that will drive their engineering. The problem is that it takes a long time; it might take a year or more in many circumstances. Customers need to ask vendors how they can help them measure and improve the quality of their operations.
I do think it is very important to adapt these tools for your local environment. So it's very expensive and inefficient to make your vendor do all this work because it's very hard for them to provide all these solutions for you. It is very valuable to have some talented, local ITs upport people who understand the radiologist's environment and can help you provide tools.
My recommendation is to hire a high school student. It's amazing what they can do to integrate solutions and to use some of these social and IT tools for Web development. They can help improve your communication within your department. That's a very low-risksolution, investment-wise, for how much they can accomplish with a little glue in your current systems.
STEVEN C. HORII, MD: I do ultrasound as a clinical specialty. So I interact with the sonographers that I work with directly. Things like quality issues come up very quickly and are corrected almost on the spot. That's the way we practic eultrasound. But an important aspect of what you talked about gets back to what Dr. Chang mentioned, and that is making this asynchronous. Right? Right now, my feedback to my sonographers is synchronous. I sit with them and say,"Could you get me a picture next time ofthe hepatic veins?" I think the advantage of the tool you have is that you are able to make this an asynchronous process. Do you see it that way?
NAGY: If you have the data recorded somewhere, you can do all kinds of reporting, which can help you really understand some nuance of how your department operates and what's frustrating your radiologists. Tagging images in a PACS is a lightweight structure that can be harvested to provide quality feedback. The customers I care about are ther adiologists, and I want to know what their frustration level is working in the environment they have. It is very important to make sure that their voices are heard in a quality-control chain. You certainly don't want to neglect some of the synchronous relationships. We try to have as many opportunities as possible to bring the radiologist and the technologist together to learn to understand this process. The reality is that technologists and radiologists are being driven apart by a variety of forces that really require these asynchronous feedback tools. Once you have this data, data drives behavior, and data drives culture. If you can use this data in the right way, it really helps you create a culture of quality in the environment. So not only is it important to have it asynchronous because of people's productivity roles, but also being able to have this data helps you move forward as a department so you can know what you're doing.
KHAN M. SIDDIQUI, MD: I have a comment and a question. What Paul has shown-the ability to integrate and mine data for different purposes-opens up a whole idea of other clinical information that is needed at the time of interpretation. We just get a small historical feel in our PACS order system, which may not reflect what is going on with the patient. To be able to access the latest clinical notes, bring in the latest lab values, and bring in the latest surgical notes will actually give the radiologist much more insight into what is happening in the case.
SIEGEL: That is part of the imageinterpretation workflow.
SIDDIQUI: Exactly. What Paul is doing in bringing these in is showing the PACS vendors and others to go to the Web 2.0 frontier. You need to be able to do much more integration, and enable us to deal with the integration of systems.
Paul, have you done any analysis interms of value proposition? A lot of departments will say, "Yeah, that's great, but how much money do I save?" Have you examined productivity or costanalysis from these tools?
NAGY: We did, and it is very hard to determine return on investment for a lot of the quality tools. The Joint Commission Critical values is a good example,it's very hard to do a cost calculation, unless you look at the fact that the average lawsuit is $2 million for a miscommunication. But that's usually more of a stick than a carrot. The other factor is satisfaction in terms of physicians and radiologists. It's hard to look at the productivity goals for some of the types of quality tools that I showed today. We have improved performance and quality, which have indirect effects on productivity.
You did mention the need, and I want to stress that more for interoperability integration. One of the reasons we're embracing the Integrating the Healthcare Enterprise (IHE) initiative is that we need to reduce the cost of integration by an order of magnitude, because we need an order-of-magnitude-greater level ofintegration to make our processes transparent. We need 10 times as many interfaces than you're currently doing. If each one of them costs $20,000 today and it takes you 6 months with 2 vendors, you'll never get to the point at which you can interoperate enough to truly have an environment in which you have a holistic view of the patient experience. IHE accelerates the adoption of IT standards, which lowers the cost greatly.
PAUL J. CHANG, MD: When most of us around this table do budgets and we're trying to pitch things, we rarely have to give a return on investment (ROI) argument when patient safety is the issue; one cannot compromise quality or safety. So it's usually not an ROIa rgument. It usually is a total cost of ownership (TCO) analysis. Usually, it is "easier" to play the TCO game than the ROI one.
One of the perspectives I have when you look at the whole quality chain is that it's not just the technologist. Ramin Khorasani has really educated me on this. We have a similar tool that Paul describes at our institution, and a lot of the errors we have found, especially with cross-sectional imaging, happen because of miscommunication of the protocol, not matching the right protocol that was done by resident or a radiologist and the technologist. Have you found a similar kind of issue where there is a disconnect between the protocol and the actual implementation?
NAGY: Absolutely. I think protocoling is a very important. I have seen encouraging things from our RIS vendors in terms of their ability to understand the protocols of preacquisition workflow step that the radiologist could and should get involved with. Certainly residents in our department view a lot of that, as well. I think that one of the greatest ways to improve quality is to reduce variation. The more standardization you do, the more it improves your quality by having repeatable processes. Protocoling is an area in which a lot of the variation is unnecessary. So trying to reduce the protocol or trying to tailor them specifically to the patients is certainly animprovement in the diagnostic accuracy of the information you acquire.
CHANG: I really like your technologist peer review. Have you incorporated the radiologist RADPEER process within this? As you keep saying, the idea is that we need interoperability, which gives us the ability to do it within the context of our workflow. When I'm looking at my PACS, I press a QC button and that's the time that I'm going to do it. Have you incorporated and extended this model to radiology peer review as well?
NAGY: We've done it for 2 different levels. One is for RADPEER, and one is for resident review. We have residents who do Emergency Department call overnight and radiologists come in the morning. Sometimes residents will have left by the time the radiologist has reviewed their work. But the radiologist wants to ensure that the resident reviews the finding and make sure there's a handoff in that process. So we built the tool for resident sign-off.
We also use RADPEER. I haven'tf ound it as successful as that. We do use it for our monthly quality reviews. It hasn't been as useful for information for continuous quality improvement because the rates are incredibly low even though we review >1400 studies a month. It helps us to identify gaps in some ways, because there's a lot more variability when you've got RADPEER and you only have 0.05% of your studies with a 3 or a 4, which is the ACR criteria for significance of missed findings. It's very hard to use that as enough justification to understand what's missing in you reducational process. I found it's been good behavioral information and good personal information, but that it is not as useful for departmental-wide continuous quality improvement initiatives.
SIEGEL: Paul, some radiologist sconsider the referring physician to be the "customer." So it occurred to me as you were talking about getting feedback from technologists and also from radiologists that it might be interesting to provide a mechanism to solicit feedback from the clinicians as well. This could be on the perceived quality of images or whether the study and report provided the answers to their questions successfully. I find it interesting that most departments don't get feedback from their clinicians in a more formal or semiformal fashion, or at least informal but solicited feedbackfrom the clinicians about their perception of quality in the imaging department and whether or not we're actually meeting their expectations.
NAGY: I think customer relations management is a whole new frontier for radiology. I am a big fan of peer reviews.I think the technologists know what good work is; they're trained in the art of it. I would want our peers to review our work, because that's a little bit more informal way of quality improvement than from our customers. Customers are a little bit harder in terms of providing feedback, in terms of understandin gwhat their needs are. Do the results answer their questions? Do they help them make management decisions? There's a lot of work that we can bedoing to improve customer relations management. We need to really tailor our services to our customers more tightly, understand exactly what they're looking for, and answer their questions better. I think there are some feedback tools. We do try to use "return receipt" to see when they've looked at the results of the images.
In the ED, we look to see whether the emergency physician looks at the images. They look at it very synchronously to when the radiologists look at it, so knowing who's been looking at images is an important part of our communication process. What's interesting is that IT is sitting on a gold mine, and radiology is not using any of this information. I think it's going to be a great differentiator for practices that can use this IT knowledge in terms of business intelligence. This knowledge can be used to help tailor their services to be more competitive and to understand how to use their resources wisely to get the biggest bang for their buck.
SIEGEL: We provide feedback in different dashboards in the department. It might be interesting to actually have ac linician dashboard. While they are our customers, it's actually part of our responsibility for optimal patient care to understand how they are receiving and utilizing the imaging studies and results. Do those who request the study actually look at the results of the study? Do they look at the images? If we make a recommendation for follow-up, do they actually follow our recommendation?
NAGY: That's a good quality indicator. Follow-up is very interesting as well. That's going to be an interesting area forinformatics to be engaging, to understand how much of a value is the radiology and the practice of the patient?
SIEGEL: Paul was talking about pay-for-performance for radiologists, but it may be that part of pay-for-performance for clinicians might have to dow ith how they utilize our radiology services. Mining that vast amount of IT information you were talking about to provide feedback for and to those clinicians might be interesting.
NAGY: Absolutely.
HORII: We do use feedback from our referring physician colleagues, but it's part of our incentive process. But you can look at as a quality improvement issue in that we seek feedback from the referring physicians. That feedback goes directly into our incentive parameters.
When this article was written, Dr. Siddiqui was Chief of Imaging Informatics and Cardiac CT/MRI at the Veterans Affairs Mary land Health Care System, and Co-Director of the Imaging Informatics and MRI Fellowships at the University of Maryland School of Medicine, Baltimore, MD. He is now Principal Program Manager, Health Solutions Group, Microsoft Corp., Redmond, WA. He currently chairs the IT and Informatics Committee for the American College of Radiology and also chairs the Advanced PACS-based Imaging Informatics and Therapeutic Applications Conference of SPIE Medical Imaging 2009.
In the early 1970s, computed tomography (CT) studies generated just a few images that radiologists could spend time examining in detail. Today, a typical trauma CT study at the University of Maryland Shock Trauma Center consists of 2000 slices. A typical cardiac CT study may generate ≥6000 images. The difficulty of evaluating so many images has spurred the movement toward volumetric or 3-dimensional (3D) interpretation of imaging data. More and more radiologists are taking advantage of a multitude of tools that enable advanced visualization, advanced functional analysis, and quantification of pathology.
Vendors have developed a variety of workstations to support 3D imaging. The traditional workstation is a "thick client" to which images are delivered for image rendering and display. There is, however, a growing trend toward use of a "thin-" or "smart-client" configuration, in which image rendering takes place on the server or "back end" at the data center. Images are streamed to the workstation for display. Another option is to display all images on the picture archiving and communications system (PACS).
Image visualization
There are two basic forms of image visualization solutions: 1) client-side rendering, and 2) server-side rendering.
Client-side rendering
How image rendering takes place can have an important impact on workflow. Client-side rendering creates a big disadvantage of limiting one user at a time to use a costly workstation. There are multiple workflows for client-side rendering depending on who actually interacts with the workstation. In one version of client-side rendering, a technologist does all the processing. The scan is performed on the CT scanner, and data are sent to the advanced workstation and to the PACS. Processed images are then created by the technologist and pushed to the PACS again, where the radiologist interprets them. In this workflow, the radiologist is at the mercy of the technologist, who decides the format and orientation of images the radiologist will see.
Another form of client-side rendering involves the radiologist directly performing image processing. In this case, images acquired on the CT scanner are sent to the PACS. Either the radiologist reads the images on a 3D workstation situated adjacent to the PACS, or the images are pulled from the PACS to a separate 3D workstation for processing. Client-side rendering forces clinicians and radiologists to physically go and find the workstation, which could be anywhere in the hospital and is sometimes difficult to find. This creates a hindrance to the use of advanced image processing.
When the PACS and 3D workstation are not tightly integrated, workflow can suffer. Typically the radiologist views 2-dimensional (2D) images on the PACS. However, in order to do multiplanar processing or 3D visualization, measure stenoses, or use other advanced tools, the radiologist must go to the 3D workstation, which may or may not be located nearby.
A semi-integrated PACS and 3D workstation is more convenient because it makes possible simultaneous examination of the data sets on both the PACS and advanced workstation without having to physically move from one place to another. However, the workstation must be very robust for client-side rendering. In addition, unless there is integration of contextual data between the systems, it will be necessary to duplicate the input of patient and study information from the PACS into the 3D application.
There are certain advantages to using client-side rendering. First, most 3D workstations available today are designed for this use. Technologists and 3D lab personnel can preprocess image data before the radiologist looks at them. Once the data have loaded, all functionality is performed locally on the 3D workstation. And many 3D workstations are sold at a discount when purchased at the same time as a scanner.
There are also disadvantages to client-side rendering on a traditional 3D workstation. First, it is necessary to buy multiple workstations for multipurpose or multidepartmental use. Still, workstation locations are often limited and may be inconvenient. Typically, an institution buys just one or two 3D workstations, and all users must share them.
To handle all of the image data, a powerful computer with multi-gigabytes of random access memory and, usually, multiple processors is needed. The distributed architecture can create problems, as not everyone may be reading from the same dataset. For example, if data are sent to a 3D workstation for rendering, and the patient is later re-imaged or an abnormality is identified and annotated at the PACS workstation that information may not be available to the radiologist working at the 3D workstation. Lastly, a robust network is required, given the amount of data that must be transferred to the 3D workstation for processing.
Server-side rendering
The biggest advantage of server-side rendering is that data are available wherever they are needed, anytime they are needed. In addition, everyone who is accessing the data is interacting with the same data from the same server. Information can be saved on that server-a defining pathology or measurements of ejection fraction or perfusion, for example-and all users have access to it.
Server-side rendering is less network-dependent because only a small amount of data is transmitted at a time, and the streaming technologies that most vendors use don't require a robust network. In addition, workstations do not need robust computing power, as most of the processing work is done at the server. The biggest advantage for server-side rendering solutions is that advance image processing applications are available to the entire healthcare enterprise and can significantly enhance patient care by making advance image data available to every physician. Image processing can even be done from home while securely connected to the server at the host institution.
One disadvantage of server-side processing is the limited number of applications currently available. This is rapidly changing, however, and at the time of the publication of this article, all applications available on stand-alone workstations may be available on server-side rendering clients. Many vendors are putting advanced cardiac analysis applications and virtual colonoscopy applications on server-side rendering clients, for example. Another disadvantage is that there may be a reduction in performance when more than the optimal number of users are accessing the same data and on the server configured for a lower number of concurrent users. In a high-volume practice, such delays may reduce radiologist productivity.
Survey: Integration
To better understand the need for tighter integration between 2D and 3D interpretation, we deployed a survey on the Internet in 2006 jointly with the Departments of Radiology at VA Maryland Healthcare System, Baltimore, MD, and Stanford University School of Medicine, Stanford, CA. 1 We wanted to know whether radiologists and cardiologists perceived a need for a seamlessly integrated 2D/3D application or a 3D advanced visualization application from a single PACS vendor.
We received 503 responses to the survey, approximately two thirds from radiologists and one third from cardiologists. We were surprised to find that 96.2% of radiologists and 92.3% of cardiologists reported reviewing CT or magnetic resonance (MR) images using 3D and multiplanar reformatting. We also asked who usually creates multiplanar, 3D, or volume-rendered images for interpretation. Both radiologists and cardiologists reported doing image processing themselves during the interpretation in the majority of cases, rather than relying on technologists (79.2% and 69.2%, respectively). We found no significant difference between academic radiologists and private-practice radiologists in the likelihood of processing images during interpretation (78.1% and 81.0%, respectively).
These responses suggest that both radiologists and clinicians want integrated 2D/3D workflow that makes use of the same application. In addition, they want to be able to interact with those images rather than use precanned screen captures from a workstation.
In 2006, we conducted a study that asked the question: If a PACS with a seamlessly integrated 2D/3D capability were available, what would the ideal display layout look like? In designing the study, we made the assumption that radiologists would use 2 monochrome high-resolution displays and 1 color display. In hindsight, we should have assumed the use of 3 color monitors. As a result, there is some discrepancy between our study data and what we would expect to find today. 2
The study involved 8 radiologists from 3 different medical institutions using 6 different PACS systems and 4 different 3D systems. The selection of a breadth of users with multiple systems provided us with better information on workflow.
As expected, in a survey of 8 radiologists and 18 protocols, there was a large amount of variance in the initial "blank slate" evaluation, primarily in the layout and positioning of particular image series. However, there were similarities in windowing/leveling, orientation, and 3D presentation states.
When the initial results were compiled and the participants were presented with a consensus layout, there was a high level of agreement. We were surprised to find that all 8 radiologists wanted the images to be laid out in a 4-on-1 display on both monochrome monitors, with volume-rendered image on the color monitor.
Second, all radiologists wanted images presented in axial, coronal, and sagittal planes for every case. Third, all users requested multiple preset windows and levels. However, not all window/level settings were requested for every orientation; instead study participants wanted them to be tailored to the task at hand. For example, they requested bone window/level settings on sagittal images of a CT of the chest, as this is the best orientation for evaluating compression fractures of the spine. When evaluating for lung nodules, they requested lung and soft tissue windows.
Finally, they requested that 3D series also be tailored for specific tasks-for example, axial maximum intensity projections (MIPs) to evaluate for lung nodules and coronal MIPs for vascular interpretation.
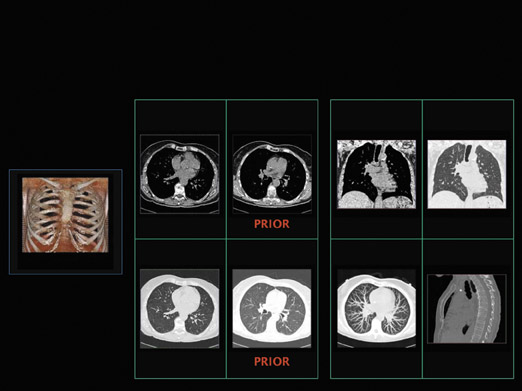
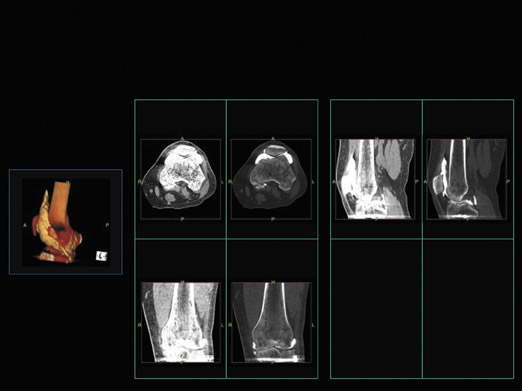
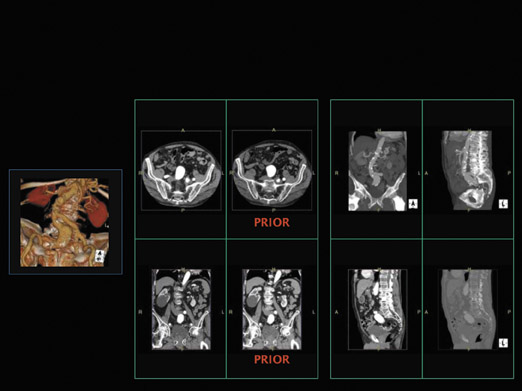
We then brought all 8 radiologists together and asked them to agree on a consistent layout. Some of protocols they decided on are shown in Figures 1 through 3. Figure 1 illustrates the presentation of a chest CT with prior studies. The radiologists said they would want to see current and prior images simultaneously on the same monitor. They would also want to see a multiplanar interpretation along with a MIP on the other monitor, and a volume-rendered image on the color monitor. Figure 2 shows an extremity CT without any prior studies, while Figure 3 shows an abdominal CT with prior studies.
Study participants also indicated that all 3 monitors should have color displays, so that advanced visualizations could be put on any portal available, not just a single monitor. These studies clearly identify a need for a 2D/3D integrated solution and radiologists' preferred layouts and types of displays. The next step was to determine whether radiologists actually worked in this way. To answer that question, we looked at the interpretation process in real time at our institution.
In the past, workflow studies involved human observers with stopwatches. That approach not only takes a great deal of time and personnel, it interferes with daily workflow and is full of errors and bias. In fact, this approach creates a "fish bowl" phenomenon in which radiologists actually change the way they interpret studies in response to being observed.
To avoid this problem, we created a new method that uses automated data extraction and data mining from the PACS and the 3D application to assess the interpretation process in real time. It documents the actual interpretation process and assesses the variability of interpretation throughout the day, without the need for personnel observing a radiologist. In addition, radiologists are not aware of being observed by anyone, even though they know they are being tracked by the application.
We identified lists of desired auditing functions, including use of workstation tools, navigation strategies, time-stamped functions, and percentage of time spent looking at advanced visualizations versus multiple imaging planes. We used the audit logs from the PACS and 3D systems that were originally developed for "debugging" purposes. In their raw form they are essentially unreadable, but we converted them to a much more useful format from which we can extract information to understand how the radiologists interact with images based on slice information, navigation time, etc.
The initial phase of the study was conducted in 2003, 1 year after implementation of server-side rendering and thin-client enterprise advanced visualization application. We found that 36% of all CTs done in the department were being examined in a nonaxial mode by radiologists, as were 1% of studies reviewed by nonradiologists.
We repeated the study in 2005 and found that 90% of all CT studies done in the department were being examined in a nonaxial mode by radiologists. Among nonradiologists, 21% of all CTs were being examined in a nonaxial mode.
To determine whether these results were unique to our department, we looked at audit logs from 3 different institutions. At site A (our institution), 90% of all studies were being looked at by clinicians or radiologists in nonaxial mode. At site B, an academic institution, nearly 25% studies were being looked at in advanced visualization mode. At site C, a community hospital, only 6% of studies were being looked at in advanced visualization mode. When utilization of 3D visualizations was tracked over time, we saw increasing utilization of advanced visualization at site A, whereas utilization at the other two sites was nearly flat.
In the middle of the study period, site B integrated its clinical applications with the PACS and changed its procedures so that all studies done on the scanners were automatically sent to the server-side rendering application. It also added a 3D button on the PACS that the radiologists could use to launch cases on the 3D applications. After site B implemented the new policy and made it easier for radiologists to do 3D interpretation, we found that the utilization trend became similar to that of site A, where all studies automatically went to the thin-client application.
At site C, the advanced visualization server was in an on-demand mode. All studies were reconstructed on the scanner; therefore, many MIPs, multiplanar reconstructions, and other nonaxial images were sent to the PACS directly rather than to the thin-client application. When radiologists needed to view studies on the thin-client applications, they would ask the technologist to push them from the PACS. At site C, 3D utilization remained low throughout the study.
These results showed that if an institution enables technology, makes it available, and incorporates it into the work-flow, radiologists will use it. Studies by Dr. Siegel 3 have shown that use of an advanced multiplanar interpretation process actually saves time, for example, cutting the time spent reading a chest CT from an average of 7 minutes to an average of 5 minutes after implementation of a thin-client solution.
Current and future trends
It has become obvious to vendors and the academic community that making image data available anytime, anywhere is key. True thin-client workstations with server-side rendering and enterprise-wide distribution are the current trend.
As time goes on, and more and more studies involve dual-source scanners and multispectral imaging, there will be too much data for workflow to focus on the examination of axial, coronal, and sagittal images. Instead, workflow will need to become anatomy-driven and pathology-driven.
To do that, it will be necessary to automatically identify where the desired anatomy is. Some vendors are developing tools that preidentify anatomy before radiologists open the study, so that workflow can be based on anatomy. It will also be important to prespecify how radiologists want to see certain anatomy or pathology, rather than simply viewing traditional planes.
Another trend spurred by increasingly robust Internet technology is truly browser-based advanced visualization with "zero footprint," without the need for a client installation or even a "plug-in" for image viewing. This truly enables enterprise-wide and Web-based deployment of imaging solutions, and even opens the possibility of sharing images with patients.
REFERENCES
- Lau D, Siddiqui KM, Herfkens R, et al. Survey of 3-D visualization usage. Presented at the 92nd Scientific Assembly and Annual Meeting of the Radiological Society of NorthAmeria. Chicago, IL; November 26, 2006.
- Boonn WW, Siddiqui KM, Vandermeer P, et al. Defining and evaluating custom 2D, 3D, and advanced imaging digital display protocols. Presented at the SPIE MedicalImaging 2006: PACS and Imaging Informatics conference. San Diego, CA; February 14, 2006.
- Musk A, Siegel E, Siddiqui KM, et al. The use of workstation auditing tools to determine how 3D/multiplanar workstations are used in the routine interpretation of CT of the thorax. Presented at the 90th Scientific Assembly and Annual Meeting of the Radiological Society of North Ameria. Chicago, IL. November 28, 2004.
Roundtable Discussion following the presentation:
Advanced visualization: Making the right choice
Khan M. Siddiqui, MD
ELIOT L. SIEGEL, MD: That was a great talk, Khan. It brought up a lot of really interesting questions. My personal computer has an operating system that allows me to specify which application I want it to use, whether it's an MP3 file for music, a .jpeg file for an image, or a movie file. That's really great because I get to pick and choose the application that I want for certain types of media. Do you see a time coming any time soon where I'll be able to sit down-and whether it's PACS that's driving my image interpretation list or my radiology information system or reporting system-that the best of breed application for visualizing those types of images-whether they are nuclear medicine, MRI, ultrasound etc.-will be invoked automatically? Do you see a PACS being used to call up the best application for the specific images or should it be a separate software portal? Should PACS vendors be moving in a direction that expands our options beyond their own company's applications?
KHAN M. SIDDIQUI, MD: I think that's a great point, Eliot. I do believe thatit's a function of the PACS vendor to provide that functionality so the appropriate application is launched based on what the need is. But this comes to the whole point that Paul talked about, the Web 2.0 concept of application, for which you need to have additional data to understand what application is required for this study. So you need to understand why the study was ordered, not just based on "rule-out pneumonia," for example-you need to understand more about the study.
Is it known how this study was acquired? Are the technologist's comments available and do they note the clinician's ordering process? When was it ordered? Was it in the acute setting or the chronic setting? A lot of information will be needed to understand what application needs to be launched to do that. For that, we need the integration that we talked about. You need the sophistication of data-mining capabilities, and then it needs to be determined if the PACS or third-party application will actually launch. The PACS advanced viewer is where I think it needs to be.
A lot of the things that I talked about, even though we were calling it advanced visualization, have actually become basic visualization. Roughly 90% of radiologists are doing this on every single case. So it is no longer advanced visualization. If it's a basic need, then do you look at everything the same way? No. When clinicians examine patients, they examine based on the context of why the patient is here. When we look at chest CT as chest CT, that's not in the context of why the study was ordered. Currently, workflow is difficult to implement because of a lack of innovative technologies available to understand what needs to happen. As customers, we need to push the boundaries and get the PACS vendors to think out of the box, to deploy more workflow-enhancing solutions so we can personalize the interpretation, as Paul mentioned. Personalized medicine is working on personalized treatment of patients. What about interpretation? Personalized interpretation of patients is based on why the study is done, what the genomic or proteomic information of the patient is, and what information the clinician needs based on his or her personal customized treatment? So I think that's where the trend needs to go.
DAVID L. WEISS, MD: I have a comment to reinforce what Khan said. Ifeel that our main impediment to using more volume rendering and advanced visualization is the fact that we have togo through several steps and the delay in bringing those images up. My question is in two parts. First, I noticed that you were trying to get consensus from your groupas to how these images should be displayed. If these could be incorporated into hanging protocols, then that display could be individualized. What is the status of that with PACS vendors?
Second, in the earlier part of your talk, you were using 2 monochrome or 2 diagnostic and 2 color monitors, and then went to 3 monitors. The 2-monitor system is really from Eliot's work in showing that that's a good balance of cost and efficiency, but that was in a simpler time using portable chest interpretation as a model. Now with so much complex information, my radiologists are asking for 4 and even 5 monitors. How do you feelabout that?
SIDDIQUI: Hanging protocols are an extremely complex question and a lot of our work is done on understanding that. I realize that the simpler it is, the easier it is. The question needs to be how easy is it for you to change your displays to your need? Rather than predefining canned protocols and then, once it fails, then it takes you half an hour just to get the images to work. Instead of spending too much time in understanding where information is, we found in our study that everybody wanted it differently hung. But there were certain commonalities. We tried to come to a consensus agreement with that. It was a challenging task and people didn't want to give up how they are used to looking at images.
So we came up with the idea that there may be a basic layout that could gain consensus in how the images are hung. For example, in our study, everybody wanted a 2-by-2 layout, so that layout could be made standard. But how the images are displayed should be easily changeable by the clinicians or the radiologists when they are looking at images. I think some vendors have done a very good job at making it very easy to implement hanging protocols and display layouts. Adding the multiplanar and 3D capabilities is not there yet. Unless somehow it's defined in the description of the series and the sophisticated PACS system has the capability to understand that, it becomes more challenging. But the majority of the vendors don't even cater to advanced visualization as part of the hanging protocol. It's considered a separate application, and they launch it wherever we set up that application.
WEISS: So you don't see that incorporation happening any time soon?
SIDDIQUI: I think we need to push and ask for it; that's what will drive it. But, yes, it needs to go into that direction. With regard to your second question about multiple monitors, this wasn't a talk on monitors, but we've done a lot of work to determine, from a human visual-perception point of view, if it makes sense to look at 4 monitors or 3 monitors. We found that your short-term memory only is about an average of 100 milliseconds for human beings. So if it takes you 100 milliseconds to look from one image to the next image, you've already lost the ability to compare. We've done some studies to show that actually you do not remember what the previous image was if that was the case. So if you are trying to compare something from monitor 1 to monitor 4, there is enough lag that-from a human visual perception point ofview-you actually don't even remember what the first image looked like. Four or more monitors make you do multiple tasks and long motions, and you are straining your neck by doing a lot of repeated motions. We have a radiologist who prefers full-monitor workstations who now has neck problems. Now he's moved down to a 2-monitor workstation because he's physically hindered by that.
But I think the display layout and, as Eliot talked about, customized and personalized layout of images can happen in 2 monitors. So 2 or 3 monitors for work-flow-type of applications is probably the best way to do it. But I think the jury is still out on what the monitor configuration needs to be. We haven't had enough experience in understanding workflow and multiple monitors with these advanced applications to really know.
Most of our advanced applications don't work on more than 2 monitors. They're hard-coded to launch on only 1or 2 monitors. So they don't even have the flexibility to expand to a full-monitor layout to look at all of this information.
SIEGEL: Interestingly, the radiologist who still uses the 4-monitor workstation configuration and has had the problems with neck strain was one of the radiologists in our study that helped to document the fact that a 2-monitor configuration is just as fast and effective and productive for a radiologist as a 4-monitor configuration. But there is that psychological need because many of us grew up reading film using alternators and other systems that displayed numerous films simultaneously. So a lot of people still want to work with multiple monitors. However, I believe that we're really able to look at only a single monitor at a time, and a very intelligent combination of software and eye-tracking technology could provide everything those radiologists would need for evaluation and comparison of multiple current and previous images using a single monitor.
WEISS: I always believed that with ideal PACS software, 1 monitor would be sufficient. Perhaps we should be looking to move toward that. If the software could interpret what you wanted to see next, you wouldn't have to go back and forth.
SIEGEL: With some sort of rapid blink mode, for example.
SIDDIQUI: Eliot always gives a standard challenge to PACS vendors that they need to be able to display all relevant clinical and historical and current pertinent information in 6 seconds in a single, easy-to-digest display.
SIEGEL: So it's not only the image but also the presentation of the information. What do you need to optimize the efficiency of that presentation? Vendors should not be limited to only visual display of information but could also supplement that with sounds, vibration, andother types of parallel output to multiple senses.
STEVEN C. HORII, MD: I have a question about the cardiologist data and what they were using the 3D reconstruction for. Were they interpreting the studies or reviewing them?
SIDDIQUI: They actually interpret the studies also. It all depends on how the departmental workflow is and how the technology is deployed in the institution. If is applied and only radiologists are using this technology to interpret images and to provide these reports, once you enable clinicians to be able to look at images themselves, they want to read them themselves. Our vascular surgeons do the same thing. No matter what we say, they want to look at the images themselves and understand what the anatomy is and see the vascular disease that we're talking about. It is the same thing with cardiologists; they want to see for themselves. Even though we interpret in conjunction with echo and coronary angiodata, they still have the clinical knowledge and understanding of what is happening with the patient. Interpretation really requires that deep understanding of what is happening to the patient now.
PAUL G. NAGY, PhD: I agree with you that we've gotten a lot of improvements moving from a workstation to a server-side rendering environment. We no longer have radiologists tethered to a workstation. We no longer have lines of radiologists waiting behind a workstation, or other ludicrous things. We do still have challenges, though, with interoperability with server-side environments. I have 3 issues I'd like you to address to the radiologists about what they should be asking for. One of the challenges we have is the issue of auto-routing our images. We're still finding that we're autorouting like we did in theearly 1990s.
The second challenge we have iswe're not really saving our work product. Radiologists spend 20 minutes in 3D space carving and slicing a model, andt hen they might save a screen capture to a PACS. If they relaunch that study on a different workstation, they will have to rebuild all that work that they did. The third challenge we've had has to do with measurement methodology even within the same vendor. If you did a study for which you measured stenosis on a vendor's system, then over time their version 2.0 might make a different measurement methodology. So there are still interoperability challenges with 3D vendors that I was hoping you could address.
SIDDIQUI: Oh absolutely. Auto routing is a big issue. I think you're keeping 2 data sets: 1 data set for your advanced visualization and 1 data set for your PACS visualization. As Paul said, there are issues with synchronicity. Do we need to establish the same images available on 2 systems? I think they need to move toward a single-storage model in which both applications are accessing the same data. But then the issues become the robustness of the storage system, the network performance, how you access th edata from the PACS, and is it robust enough and fast enough to render 4000images simultaneously and show them?
So there are some technological challenges, but I think the solutions are out there. We need to push the vendors to explore these things. Paul, I know you've pushed a lot on the vendors to think about single-storage models and access information. I think this is so much influx. The complexity of the data and the analysis is increasing, and the need for data is increasing. We have just not kept up with the infrastructure needs for that kind of data.
SIEGEL: Paul, to address your second question, what you're implying is that there should be a mechanism to save a presentation state. So rather than just storing the resulting image itself, you should be able to store something that would allow a clinician or other radiologist or other viewer to be able to take over from that saved state and perform additional manipulation or processing of the image. Khan or Paul, or anybody else, do you see any possibility in the near future of creating a standard for saving an advanced visualization presentation state?
NAGY: Well, my biggest concern is that there's such wonderful innovation going on in advanced visualization butit's becoming a bigger and bigger island. I think this is going to be a real challenge in a Web 2.0 world, when we need to collaborate and share. I think that is the challenge: how do you match standardization, which typically runs counter to innovation? Standardization is slow and is the lowest common denominator for what we can share. Innovation runs ahead of everybody else. There needs to be a bit of a mechanism to harmonize those two efforts.
PAUL J. CHANG, MD: Paul's absolutely right. One of the biggest frustrations I see is that the so-called advances in advanced visualization are actually enhancing its isolation from the workflow. Also, the problem is not just rendering. The problem we're having is actually the transfer syntax, the transmission of these large datasets from one place to another; it's not where the rendering is done.
The other comment I would make is that people tend to assume that advanced visualization equals static volumetric or morphologic visualization. In reality, it's more than just that. In fact, 40% of our work is PET/CT and MR spectroscopy. In fact, I actually believe our differentiation as value providers in radiology will be more in line with what we do to combine and integrate all the information, not just morphologic but also functionaland physiologic.
Which brings me to my question. Many years ago, when I was building PACS, it was a basic, simple thing: getting a Web client to look at X-rays and simple CTs on the Web. When we first developed our first prototype that ultimately become Stentor, I got an e-mail from the ED doc saying, "Thank you forinventing this. Now we don't need you damn radiologists anymore." That actually prompted us to realize that we need to think about our value. Is it deliveringimages? Or is it providing communication and actual collaboration?
When we put in our server-client 3D web service, a different doc at the University of Chicago said, "Thank you for doing this. Now we don't need you damn radiologists anymore." You mentioned the importance and the inevitability that we're going to go to server-side, the inevitability that we're going to have enterprise-wide distribution of the ability to look at volumetric rendering. As these advances in automatic "one button" segmentation and visualization continue, what is my value added as a radiologist? I'm going to tell you something, as an oncologic imager and a body imager, Idon't enjoy reading 3D vascular run-offs. This is because I feel I add relatively little value as a radiologist beyond what the 3D image provides.
The argument could be made that, in some ways, how do we differentiate ourselves with advanced visualization? How do we add value? How do we prevent losing our differentiation as our vendors integrate these systems? As Ramin Khorasani says, if you get better computerized physician order entry and understand the protocol and you understand what the question is you want to answer, segmentation and preprocessing can get increasingly automatic. If we actually do achieve "one button rendering," how do you address the argument that this potentially could actually add to our commoditization? At least from a morphologic context of imaging, if it's all there in the automatically rendered 3D image, and my value is just in what the arrow shows, what is my value to patient care? What is the role of a radiologist as a value provider when all of this is automated and actually provides exactly what the clinicians want? Do we need these damn radiologists anymore?
SIDDIQUI: As long as all we're doing is pointing to that stenosis arrow,and here is the stenosis, you're going to do that. But if we have more understanding of what is happening to the patient, and our interpretation is personalized to the patient, we're providing more value and we are becoming, as you talked about, physicians' physicians. Then we are making them understand what is happening and we have the understanding and expertise. If a vascular surgeon calls you and looks at a stenosis, if you don't have any understanding of what is happening to the patient and there are 10 stenoses seen so that which one is the critical one is based on a patient's clinical information, then hedoesn't need you, because he already has that information. But if you are providing that added data, added information in the context of the patient, then he can do his other tasks of treating patients and doing surgical procedures, and not spend time looking at images, because he now believes what you are saying.
The issue clinicians mention to me is that if we say that there are 10 stenoses,and that's it, then the patient comes in with some mild weak symptoms and cardiac imaging, the clinician needs to know what needs to be fixed. So that's why I have to go back in and look at all the images and figure out what's going on. That's why my value is not there anymore. But if I understand what the other imaging modalities have previously shown, what the patient context is, and what the patient's historical information is, then I can do my interpretation then based on that context. Then the clinicians do not need to go through that process to do it, and they can do other things. So we need to develop our own value. Are we just interpreting images? Or are we actually providing information that clinicians either would take extra time to find or would need more information to get their job done?
As you said, it's a really challenging task. When we go and give talks at cardiac CT meetings, if we ask the audience how many people are cardiologists and how many radiologists, 80% of the people in the audience are cardiologists.
SIEGEL: Do you think making advanced visualization ubiquitous throughout the hospital and giving full access to the cardiologist increases or decreases your value as a radiologist providing those services?
SIDDIQUI: We've deployed this since 2002, so we have 6 years experience. I now have more people asking me questions and relying on my interpretations. Even when I'm traveling giving talks, I get questions all the time. It's not uncommon to see me sitting at a conference in the audience with my laptop open and actually reading a case because some clinician wants me to give my opinion on a study. So, I've seen people asking me and interacting with me more now, even with more utilization of the advanced visualization. This point was raised on the closing session at the SIIM meeting 2 years ago in Orlando questioning if a radiologist will be a radiologist in 15 or 20 years or will he be an imager? We see the same thing in virtual colonoscopy with gastroenterologists. They want to be able to read it themselves. So, what is a radiologist going to be called 10 or 15 years from now? We've already seen special training programs started in neuroradiology and interventional radiology in which folks don't do basic general radiology but rather combine specialized radiology training with clinical specialty. So, what is a radiologist in 20 years fromn ow when all this becomes ubiquitous? Are you going to be just an oncologic imager and that's all you do, but you have the understanding of the patient and also maybe taking care of the patient the same time? Or will there still be what is traditionally known as a radiologist?
SIEGEL: Your opinion is that making advanced visualization available to our clinical colleagues will not in any way decrease radiologists' added value?
SIDDIQUI: It depends. The function may change for radiologists and what they do 15 or 20 years from now, but they will never be just imagers. That's what I think. I do not think by giving ubiquitous access for advance visualization to clinicians we will decrease radiologists' added value.
CHANG: We have to be more engaged in taking care of patients. A radiologist who is just an imager, who simply recapitulates morphologic findings as an interpretation will be of very little utility in the future, or even today. The radiologist who is going to have value is engaged as a true collaborator, someone in the tumor boards who understands therapy, who understands about the outcome and the correlation between therapy and diagnosis. There are going to be a lot of losers in radiology if they feel that they're just imagers. Then they will be commoditized because the advances in advance visualization, volumetric rendering, automated segmentation, and visualization will render those people obsolete. Imaging sevices will be a commodity because it's easier to get a cardiologist or a vascular surgeon if these tools are there for them to see all the stenoses. The radiologist who is more tuned in to the therapy and to the management of the patient as a whole is the one who's going to survive and thrive. These other imagers are not going to be around.
Dr. Horii is a Professor of Radiology and the Clinical Director of Medical Informatics, the University of Pennsylvania Medical Center, Philadelphia, PA.
Increasingly, radiology practices are deciding to add to an existing picture archiving and communications system (PACS) or to change PACS vendors entirely. These are among the most challenging transitions a radiology practice will ever face. This article will discuss why it maybe desirable to upgrade a PACS, how to manage the project, and some pitfalls to watch out for.
Adding to a PACS
The decision to add to a PACS is often driven by imaging subspecialties. Existing PACS often fail to meet the needs of radiologists who interpret ultrasound or nuclear medicine studies, for example. An ultrasound system must be able to handle not just color imaging but multiple cine loops, Doppler wave forms, and other complex tasks that PACS supplied by the major vendors often don't handle. Nuclear medicine studies involve similar challenges, particularly in the mathematical analysis of images. Cardiology is also placing new demands on PACS, as cardiologists have different requirements from radiologists when interpreting images. At the same time, new capabilities for advanced visualization may drive the need to add to or change a PACS.
Upgrading is difficult because the PACS interacts with so many other systems and devices. There are a tremendous number of interfaces involved, and that complexity affects information flow. Network loads may change, for example, and a larger amount of storage may be needed. Studies may begin to incorporate new images, as advanced imaging techniques enable radiologists to create 3-dimensional (3D) series from data that was already part of the image acquisition.
Similarly, new imaging equipment raises new issues. If cardiology is being integrated into the PACS, images should flow to the archive directly from the angiography systems. To do that, it is necessary to interface with equipment in the catheterization laboratory. Table 1 summarizes some tips for adding to a PACS.
Avoiding pitfalls
PACS and radiology information systems (RIS) do not exist as stand-alone systems. They interface with a number of other systems, including hospital information systems, pharmacy systems, admission-discharge-transfer systems, billing systems, and others. Software and hardware changes have the potential to affect the way those interfaces operate.
It is critical to consider how information will move among several PACS. Should we go back to the old store-and-forward days of routing images to where they're needed? How do we do that with different kinds of PACS? How do we get the information where it's needed, when it's needed?
At a minimum, interfaces usually require the setting of parameters by both vendors involved. The software on both sides of the interface is expecting certain behavior and data across that interface, and is sensitive to very small changes.
When managing interface changes, keep in mind that vendors generally accept responsibility only for their hardware and software and for managing their side of any interface. They will not be responsible for what is on the other side of the interface, unless an agreement to that effect has been negotiated or the same vendor manufactures both pieces of equipment.
The process of installing a new system, new software release, or new hardware usually results in downtime. Management of this process is important because it affects all users. Be aware that a system that worked perfectly during testing can still develop problems during installation. It is unlikely that any vendor can exactly reproduce your system configuration for testing.
There are many stories of major problems that developed after the addition of a new system or a change in software on an existing system. Usually, the systems themselves work, but the interface fails. For example, when we installed a new CT scanner at the University of Pennsylvania, the PACS stopped acquiring images. Both devices were DICOM conformant, but the network interface had been set for a particular scanner. When we changed that scanner, we had to change the parameters on the network interface to suit the performance of the new machine.
To avoid such problems, it is essential to completely understand the projected work flow and movement of information across the interfaces between systems, especially between a new PACS and the existing one. There must be a strict policy in place covering any changes and upgrades. Vendors should understand the policy and sign off on it. Such an agreement can avoid the common problem of a vendor who performs preventive maintenance on a scanner and, without the explicit consent of the radiologist, also installs some new software. Often it is only when the scanner stops sending images to the PACS that the radiologist becomes aware of the software upgrade.
Consider having a test system that enables the testing of changes before they're actually implemented in operational systems. As mentioned earlier, this will not catch all of the little, irritating problems that might occur, but it will catch the big ones that prevent the system from operating.
Understand that knowledge is power. A radiologist who is knowledgeable about the interfaces between systems, what those interfaces do, and what information flows across them is in a much better position to determine whether a new system is likely to impact an existing system.
It is also important to understand that interfaces have both upstream and downstream dependencies. A change on one side may affect the way devices operate on the other side.
Changing to a new PACS
If adding to an existing PACS is challenging, changing to a new PACS vendor is daunting. Many radiology departments are doing just that, however. There are several reasons why. A vendor may go out of business or be purchased by another company, for example. In addition, an existing PACS may no longer support the department's current work, or it may not expand to meet new needs. If the PACS cannot handle the advanced visualization needed for cardiac imaging, a new PACS may be needed.
A corporate decision may drive the change to a new PACS. If the hospital is purchased by a larger entity, hospital administration may sign an exclusive purchase agreement with a particular vendor. One radiology practice may take over an existing one with a very large installed base. A new radiology chairman may have a preferred system and initiate the change in the PACS vendor.
The University of Pennsylvania has changed PACS vendors 3 times. The first time, the vendor for our ultrasound mini-PACS left the business. Our main PACS vendor could not handle ultrasound images in the way we needed, so we had to make a change to a new ultrasound mini-PACS. In another case, our health system established an exclusive relationship with a single imaging equipment vendor, and we were required to change vendors for our departmental PACS. We eventually changed back when the new system could not meet our needs.
Challenges
There is no question that changing to a new PACS is painful. The most intense pain does not come from the capital costs. Nor does it come from the need to dispose of old equipment or to part ways with the existing vendor.
What is really difficult is the migration of multiple terabytes of data that reside in an existing archive. This may seem puzzling. We can store and retrieve DICOM images, so why can't we easily retrieve DICOM objects? Many PACS store DICOM attributes in proprietary database tables, reassembling the DICOM objects only when they are requested. Vendors do this because it optimizes system performance. Remember, DICOM was designed for the communication of images, not as a database format.
Typical database problems include irregularities in patient names. Is Homer Simpson the same person as Homer J. Simpson? What about Homer Simson, spelled without the p, who has a different identification number but the same birth date and the same address? Are they all the same person?
What about a head CT study that actually contains images of the head, chest, abdomen, and pelvis? What about studies that were entered into the database with incorrect order or request numbers? And what about studies that were stored on read-only memory but whose attributes were updated after the initial image acquisition? When those studies are read off the disc, they will come back with the older values in the DICOM headers.
There are numerous other examples, all with some sort of information mismatch. During the migration progress, each of these will need either manual intervention or processing through additional software.
As might be expected, interfaces present special problems. All interfaces between the new PACS and other information systems and imaging equipment will, at the least, need to be tested. In addition, a new round of interface license fees may be imposed by other vendors, forexample, the RIS vendor.
The phasing out of old equipment can create another problem, particularly if the new PACS installation runs behind schedule. In our case, we had been observing archive failures resulting from mechanical problems in the existing jukebox. We didn't fix the problems because we expected the new system to be in place before the existing system failed completely. Unfortunately, we missed the target date for installation of the new PACS. Archive failures began to occur with increasing frequency and began to affect clinical operation.
At that point, it was unclear who would handle problems with the existing system during changeover. The old system vendor was no longer under service contract, and the new system vendor was not enthusiastic about paying to repair a system it was going to replace. It took several months of negotiation with both vendors to get the situation resolved. In the end, we had support of both systems.
Recommendations
Based on our experience, it is wise to get a "prenuptial agreement" from the PACS vendor (Table 2). This agreement should provide for guaranteed access to the database and the data. If a vendor is going out of business, it is important to get the database schema from them before they shut down. Details of all intersystem interfaces are also needed, including all DICOM and HL7 messages and their content.
The agreement should include an option to continue service contracts on a month-to-month basis, with cost constraints. Service should be on the same terms as during the system's active life. If service had been available 24 hours a day, 7 days a week, it should continue at this level as long as the system is in clinical use.
The agreement should also provide for guaranteed engineering support during the transition, including a commitment to work with the new vendor. Such service will not be free of charge, but it is wise to negotiate a schedule of charges in advance.
No matter how information migration is managed-whether by the existing vendor, the new vendor, or a third party-provision should be made for DICOM objects that contain private groups and elements. Private DICOM groups are permitted in the DICOM standard, and many vendors use them. Ideally, a storage system will store these and return them on request. Determine how these will be migrated to the new system. Make sure the vendor does not simply discard private DICOM groups.
Establish realistic and firm change-over dates, as well as contingency plans in case those dates are missed. This should include an agreement about who will pay for service of the old system if changeover dates are not met.
Consider changing the disaster recovery backup to a DICOM media storage application profile system. Store all information as DICOM filesand DICOM objects, rather than in proprietary formats. Consider using a vendor-independent storage solution that supports different vendors'PACS. There are commercial vendors that provide such products, and some of the main PACS vendors can do so as well, upon request (and payment of the cost of such options).
Be prepared for failures of the old system before completing changeover to the new system, and know how to handle those failures. Do not ignore maintenance of the old system. Continue to check that backup systems are working.
Don't count on reusing old PACS hardware. Not only is the old hardware likely to be obsolete, it will be needed when the old system is run in parallel with the new system during testing and startup. In addition, if the original PACS was acquired through an operating lease, the equipment must be returned to the original vendor unless a purchase agreement is negotiated.
Consider beginning database conversion well in advance of changeover. Set a target for the amount of data to be converted prior to the changeover, typically 1 to 2 years' worth, with the rest converted on either an ad hoc basis or in a background process.
Determine who will perform database clean-up and how it will be paid for. If health system staff will be doing the clean-up, consider negotiating a charge-back rate to cover labor.
Considering having a database survey done ahead of time to determine how many problems exist in the database. This will provide perspective on how difficult the changeover is likely to be.
It will likely be necessary to run parallel systems for a while. Determine who will pay for the extra network infrastructure and hardware that may be needed to support a network that is twice its usual size.
If the change in PACS is a result of a decision by the health system or hospital administration, make sure they are aware of the full costs associated with making the change and are willing to support those costs.
Finally, appoint an "informatics historian" who will record the dates of all systems and hardware installations, keep track of all software version descriptions, and maintain a record of problems, as well as their follow-up and resolution. Such records are extremely valuable and have saved some institutions significant expenses on service contracts.
Conclusion
Adding a PACS to an existing enterprise is not a trivial endeavor. It requires knowledge and planning, chiefly with regard to interfaces and data flow. It is possible to minimize the negative impact of a PACS addition, but it is difficult to completely eliminate it. A change in PACS vendors is, without question, painful. The most effective way to minimize the pain is to thoroughly plan for the change and prepare for all that it will entail.
Roundtable Discussion following the presentation:
Avoiding pitfalls in adding to a PACS or changing PACS vendors
Steven C. Horii, MD
ELIOT L. SIEGEL, MD: Thanks, Steve. That was a very comprehensiv eand timely summary.It raises a numberof different questions. One thing that occurred to me right away was the question of adding to or replacing your radiology information system (RIS). Have you had any experience with that? Do you have any advice? Have you at the University of Pennsylvania had the opportunity to look at that possibility?
STEVEN C. HORII, MD: We have looked at it and rejected it almost out of hand, because if we thought changing a PACS vendor was tough, changing your RIS is even tougher because it has numerous interfaces and it affects numerous pieces of your operations. It's very difficult. We did go through upgrade of an RIS, which was a major change in the system. That was still painful, even after a year or so of advanced planning, and now probably a year-and-a-half out in operation. We're still finding little things that cause problems. It's very difficult to do. Idon't talk about it extensively because if you can avoid it, I certainly recommend avoiding it rather than taking it on. I mean, if you have to do it, you have to d it. But it's very, very difficult.
SIEGEL: Paul, we're contemplating this at the University of Maryland. Are we going to keep the legacy system up and running? Or are we going to migrate from the legacy system to the new system?
PAUL G. NAGY, PhD: We're migrating all the reports from the old system to the new system. It is an extensive process. I would say it's similar to a PACS migration, actually. The problem with the RIS is that there are so many different workflow components, including scheduling and registration. I think the bigger problem is that, with the earlier RIS, we were an island. We did all of our own scheduling and all of our own registration. We basically had our own master patient index inside the RIS. When you migrate to a new RIS now, most modern systems are really parts of an enterprise. So we're going to have to talk to enterprise scheduling and do a lot more interoperability than we had to do in previous versions. It's kind of hard to go from our own show to being a cog in a wheel. Probably the hardest piece for us to re-work is to rework our workflow to be part of an enterprise data synchronization stream.
HORII: In upgrading our RIS, we also went through a major change in the userinterface. It had been a terminal-based kind of roll-and-scroll interface to a multiple windows-based system. It was a large change for the users. As much as we tried to reduce the impact of that by doing change management, we still could have done more. I recommend educating your staff as far in advance as you can, and actually getting them to see the product and understand what it's going to do. We tried to do that. But, as you know, in the radiology department, the scheduling just to get people into training is very, very difficult. If we had to do it over again, we would probably insist on better change management and better education of our users.
DAVID L. WEISS, MD: Steve, many sites out there have purchased their PACS before this information has become codified and have not protected themselves as you have suggested. Many of those sites aren't planning on changing PACS in the nearf uture but may be facing that in 2 to 4 years. Can you expand on what can be done now to back-fill to protect yourself if you haven't done this in the past but may want to change PACS 3 or 4 years from now?
HORII: Well, there are things you can do. A lot of PACS are installed with periodic hardware refreshes, for example. So the vendor will come in after 3 years and offer to replace your workstation hardware, expand your servers, or upgrade something at a discounted cost. Often, those are opportunities at which you can say, if we're going to do this, we'd like to negotiate some new conditions. We've got to put in new workstations, and we're going to put in a new archive. We've done this and we took those opportunities to say we'd love to stay with you guys, but if you're going to do this, we want these new things included. For us, one of them was a change to a DICOM-based archive instead of a proprietary one. We managed to get that negotiated as part of a hardware change-refresh scenario. So you have some opportunities.
The other thing, of course, you can do is negotiate for service. The vendors are very interested in the service side of your business. Service contracts generally are profit-making for many of the vendors. Those things are often negotiated on a shorter-term basis than the whole lifetime of your PACS. So that's another point at which you have so much opportunity to renegotiate what you may want to do in the future.
SIEGEL: Is it a fantasy to think that leasing arrangements or pay-per-volumeo f studies arrangements make it any easier to migrate to a new PACS system? Is that something that one should consider?
HORII: The amount of labor required is similar. The advantage you have with lease agreements, though, is that you still have some leverage over the company since it's a continuing thing. If they have the hardware in ther eand you paid for it, at that point, you're at their mercy. If it's a leasing agreement, they know that you could change out of it the next time the lease is up. So it puts a little more pressure on the vendors. But when it actually comes time to change, it's still not any easier.
SIEGEL: One of the things I was wondering about is disaster recovery or a backup. It's one thing to migrate your database, but can you migrate your disaster recovery system and your backup? When you go to a new PACS system, then do you have a backup? Or do you also need to create that backup simultaneous with migrating to the new system?
HORII: That's a tough, tough problem, and it's a reason why some people have said that if you have a disaster recovery storage out there, that you should maintain enough of your presents ystem that you could pull data back from it if you need it, but don't bother to migrate it all. Your need for the backed-up studies tends to be fairly low. You're only really going to need it if things go bad very quickly.
SIEGEL: Presuming you have the software to be able to access it.
HORII: Yes, presuming you have the software to be able to access it. That's the advantage of going forward. If at all possible, look at your disaster recovery solution as a vendor-independent one so that you could pull it back from any vendor. Remember that your need for that is likely to be rare-at least you hope thatit's rare. But when you do need it, you need to be able to get it back fast enough that you can be back in business, or why have it at all? If it takes you as long to retrieve the stuff as it did to put it in there, it's not a very good backup solution. So some consideration has to be given to making that work, because it has a potential to exist for a longer time than your present PACS implementation. It's something that's vendor-independent.
NAGY: For archiving solutions, when you're archiving the files in DICOM, it's a very admirable thing to do. The challenge is that if you do a file-based migration later on without that PACS vendor, you're going to lose all the patient demographic updates. We find as many as 20% of our patients change their names or information. We're a large trauma center,so we often find out who they are after we've imaged them. If you work with an enterprise archive vendor, make sure that they're also capturing an Health Level 7(HL7) feed, and capturing ADT (patient administration messages) in the patient updates.
My question for you has to do with migration time. There's this very annoying rule of thumb coined by Fred Behlinof one third-that if you have 3 years of data on your PACS, it's going to take you 1 year to get that data off. If you've got 6 years, it's going to take you 2 years to ge tit off. Some of it is because of the slow transfer rates of earlier archiving strategy technology, such as digital linear tapes and magneto-optical drives. Some of it is the fact that it loads the performance on the old PACS to a point at which the radiologist can't use it while you're trying to transfer data off of it. Some of it has to do with the curation of the data that has to be done to get it off. It's been frustrating how it's been reinforced several times that it takes this long to get this data off. Steve, my question is how long did it take you to get the data off? And what were the limitations in trying to get it off?
HORII: One of the problems that we had was that it was taking longer, actually, than that estimate. That was becauseof the number of problems we had in the database: the number of unspecified studies, the number of studies with incorrect patient names or patient names that had changed, all those sorts of things. So it actually took us longer. The vendor didn't use Behlen's estimate, but used an estimate that was also based on having access to the old PACS server 24 hours a day. We said, "Well, we're still using that system. You can't do that." So it automatically nearly doubled the amount of time it was going to take. So, yes, that'san important consideration. I would say that the one-third rule is probably a conservative estimate. It's unfortunate, but that's apparently what we live with now. If you look at what some of the vendors are proposing now, especially the ones who proposed just storage solutions, they're now including things like a layer that manages changes in the fixed content files that would allow you to make a migration more quickly than that. It can basically just change the upper layer and change the database tables. But the problem is if you have an existing installed base of it, it's not like that, and it's tough to change it.
NAGY: I'd recommend archiving backwards in time, to go from the present backwards. That way, the most relevant information is probably the more recent. I have another question. In early 2002, the IHE came up with a couple of profiles called Consistent Presentation of Images. With this, when a radiologist is looking at 1000 images, they select the 4 that are important to them. They might do mark-up, like circles and arrows, and those annotations are then in the system. When you change PACS vendors, without IHE, how do you maintain that work product?
HORII: The problem is that it will often go away unless it's made as a DICOM presentation state. Unless you basically change the objects and include those as a DICOM overlay, they're going to be part of the proprietary database of your PACS vendor. That's the case with most systems. The key image note and presentation state storage, if it's done right, is a DICOM thing, and you should have it. But I don't know that a lot of the vendors actually support presentation state storage.
NAGY: The newer ones do. It's a surprise to me when radiologists don't own their work product in their system, and they're going to lose it when they migrate to a new PACS vendor.
SIEGEL: That's a great point. Well,thanks, Steve.
Dr. Weiss is the Clinical Section Head for Imaging Informatics at Geisinger Health System, Danville, PA. He is also a member of the editorial board of this journal.
Currently, there are a handful of ways to create a radiology report. For decades, the standard has simply been transcription, coupled in more recent years with digital dictation. Another option, structured reporting, is used by many radiologists in mammography but is not widespread in general radiology. This article will focus on speech recognition, which is being adopted by more and more radiology departments, in both academic medical centers and private practice.
One of the purported advantages of speech recognition is cost savings. In reality, a speech recognition system may, at least in part, shift costs rather than save them. This is because instead of paying a transcriptionist, a radiologist spends time editing and typing. However, without question, improved turnaround time is an advantage of speech recognition, as has been documented in a number of studies. 1,2
One of the disadvantages of speech recognition is a time penalty. A majority of radiologists report spending more time creating and finalizing reports using speech recognition as compared with conventional dictation, with a resulting decrease in overall radiologist productivity. 3,4 However, the most serious problem with speech recognition is its potential to distract the radiologist from viewing images. If the radiologist's eyes are on the dictation screen rather than on images, the risk of error increases. 5
Acceptance of speech recognition by radiologists has been complicated by a misalignment of incentives. Radiologists only indirectly benefit from the advantages of speech recognition. If cost savings help the department to stay under budget, radiologists might receive a bonus, but it will be slow in coming and will be shared by many others. Similarly, improved turnaround time will help to achieve departmental goals, but diagnostic accuracy and productivity are more important to most radiologists.
On the other hand, the disadvantages of speech recognition fall directly on radiologists, as they suffer the potential for a time penalty, productivity decrease, and distraction from image viewing. Administrators and information technology staff must pay attention to this misalignment of incentives and find a solution to it if they want radiologists to adopt speech recognition.
Case studies
The following case studies illustrate both the success and, in some ways, the failure of speech recognition.
Community hospital
The first case study involves Chestnut Hill Hospital, a small community hospital in Philadelphia, PA, with a general radiology practice of 4 to 5 radiologists reading 100,000 examinations annually. In 1998, we installed speech recognition, shortly after hardware and software advances made it practical for radiology use. The next year we installed a picture archiving and communications system (PACS) and, in early 2000, we integrated the 2 systems.
All of the radiologists agreed to implement speech recognition. We discontinued using a transcriptionist after about a week. What followed was 4 weeks of difficulty. First, we ordered the wrong microphones for data entry (ones without a barcoder). We weren't proficient in using the product as it was designed. Macro techniques were still in their infancy. The navigation controllers we use today were not available. And, initially, there was no integration between the PACS and speech recognition.
Nonetheless, report turnaround time decreased from approximately 72 hours to 20 to 24 hours immediately after implementation of speech recognition (Figure 1). There was no further significant reduction in turnaround time during the first 6 months after installation of the PACS. However, after we streamlined workflow to make the best use of the PACS, we did see a major drop in turnaround time to an average of <4 hours for all studies.
A major change in workflow involved the radiologists' work schedules. We were accustomed to leaving the hospital at 5 pm each day, when the film library stopped distributing hardcopy studies to be read. Several months after installation of PACS we realized that, since PACS produced images hour after hour, we could reconfigure our work schedule. All but one radiologist began to leave the hospital at 4 pm, while the on-call radiologist stayed until 7 pm. This new schedule consisted of the same total number of work hours, but resulted in much better turnaround time.
Large medical center
At Geisinger Medical Center, we have digital dictation and use structured reporting for mammography. We installed speech recognition in the third quarter of 2004, and radiologists were encouraged, rather than given a mandate, to use it. Therefore, at each workstation we still have both a speech recognition microphone and software, and a conventional digital dictation system.
An interesting pattern developed. After 6 months, half of our radiologists were using speech recognition 80% to 90% of the time, and the other half were using it ≤30% of the time (Figure 2). This was a bit surprising. It is more common to see a bell-shaped usage curve, with most of the radiologists accepting speech recognition, a handful really embracing it, and a handful really struggling with it.
What happened at Geisinger? We did get buy-in from the radiologists initially, but we may have had unrealistic expectations of accuracy that led to frustration with the product after implementation. A training session with a trainer who knows the software inside and out- and software that has become highly accurate in recognizing that trainer's speech-is far different from a new user's initial experience. In addition to problems with the speech engine, we also had some disruption attributable to the PACS and the radiology information system (RIS).
These were not the real reasons speech recognition was not widely used at Geisinger, however. The main problem was that we did not communicate a consistent message that the department would be adopting this technology. We also had no defined endpoint for eliminating digital dictation and have continued to support 2 separate reporting systems.
Ensuring success
Table 1 outlines some of the steps that can be taken to ensure adoption of speech recognition. First, provide meaningful incentives to users. The incentives could include bonuses, extra time off, or a reduction in productivity requirements for radiologists who use speech recognition. Don't allow use of the system to be voluntary.
Have realistic expectations and plan for a drop in productivity. Most studies show at least a 10% reduction in radiologist productivity after implementation of speech recognition. There are some exceptions, however. For example, at the community hospital profiled earlier, my colleagues and I all felt strongly that we were more efficient when using the integrated PACS-speech recognition product.
The University of Pittsburgh showed at least a time-neutral effect after installation of speech recognition using a hybrid transcriptionist-radiologist editing process and some modifications in workflow. 6 Massachusetts General Hospital (MGH) recently did a productivity study of PACS and speech recognition in collaboration with New York University. They were able to show that at MGH the use of PACS had a positive impact on radiologist productivity, while speech recognition had no statistically significant effect on productivity. 7
Plan for training and ongoing support. Even experienced users will have problems now and then. When new radiologists join the department or locum tenens radiologists arrive, they will need support on the system.
Set a deadline for the removal of conventional transcription and transition to speech recognition. Consider using a hybrid model for report editing. One way to use speech recognition is to have radiologists dictate, edit, correct, and sign their own reports. Another way is to have radiologists dictate reports, and then use "back-end" transcription for editing. In this process a transcriptionist listens to an audio file while viewing the text and making corrections. Although this approach relieves radiologists of clerical work, it reduces cost savings and results in variable turnaround times. Consider combining these 2 approaches, so that radiologists who are proficient with speech recognition can work independently and those who are struggling or in a time bind can send reports to back-end transcription.
Christiana Care Health System in Wilmington, DE, provides an example of a hybrid model for report editing. All radiologists use speech recognition but are given the choice of self-editing or back-end transcription. Approximately half of the radiologists choose to use self-editing 80% to 90% of the time, and about half of the radiologists send their reports to back-end transcription. 8
Take steps to maximize efficiency. With speech recognition, efficiency is determined by accuracy, navigation, integration, and macro use. To maximize accuracy, it is best to use a headset microphone. This will improve accuracy by standardizing the distance and the position of the microphone in relation to the mouth. With a hand-held microphone, approximately half of the errors can be attributed to not holding the microphone in the correct position.
Make corrections properly, either using the correction mode or, in the case of some speech recognition systems, the vocabulary editor. This is a way of training the system to learn each user's specific speech patterns.
Pay close attention to ambient noise. It may be helpful to have the walls of the reading room covered in acoustic paneling and to have acoustic tile or carpeting installed on the floor. If ambient noise remains a problem, consider putting in a fan or some device that generates "white noise."
Speech recognition requires not just dictation but navigation through the text and various screens of the speech recognition system, as well as simultaneous navigation through the PACS. It is important to consider how to make this process seamless through use of a mouse, a microphone with programmable buttons, or some other navigation aid.
Integration is another critical factor in efficiency. It is fairly easy to use a stand-alone speech recognition system. It is much more difficult to achieve interoperability between the speech recognition system and the PACS or RIS. The interface with the RIS needs to be bidirectional, enabling the accession number to pass from the RIS to the speech recognition system, and in the other direction, for text and any other information to pass back to the RIS.
Even simple integration algorithms can eliminate unnecessary tasks. Without them, it is necessary to first open a case in the PACS, then open dictation in speech recognition, and then add demographic information. Integration enables distillation of the workflow into simply viewing images, dictating, and signing the report. The case is closed automatically, the next case opens automatically, and the radiologist views the images, dictates, and signs the report.
Macros and templates are essentially canned reports that the radiologist can pull up anytime and modify. With speech recognition, the use of macros magnifies the time savings. Not only does it save time in dictation, it saves time in proofreading.
Figure 3 shows the modification of a macro for a CT scan of the abdomen and pelvis. The macro states: "Aorta is normal in size." To modify that text, the user verbally selects the sentence and substitutes: "There is an aneurysm of the lower abdominal aorta measuring 4.8 centimeter in diameter." The user also changes the impression from: "No significant abnormality in CT scan of abdomen and pelvis" to "Abdominal aortic aneurysm. No other significant abnormality…."
All of the radiologist's edits are done verbally, without the eyes ever leaving the images. Not only is this method much faster than dictating an entire report, the radiologist has only 2 phrases to proofread.
Conclusion
Effective use of speech recognition can yield major improvements in report turnaround time. This technology is not always well accepted by radiologists, however, in part because it can reduce productivity, at least initially.
To encourage radiologists to adopt speech recognition, it is essential to offer meaningful incentives. It is also helpful to identify departmental champions who can generate excitement about the new technology, to set a firm date for discontinuing conventional transcription, and to maximize efficiency by improving accuracy, streamlining navigation, integrating speech recognition with the PACS and RIS, and taking advantage of macro functionality.
REFERENCES
- Mehta A, Dreyer KJ, Schweitzer A, et al. Voice recognition-An emerging necessity within radiology: Experiences of the Massachusetts General Hospital. J Digit Imaging .1998;11(4 Suppl 2):20-23.
- Ramaswamy MR, Chaljub G, Esch O, et al. Continuous speech recognition in MR imaging reporting: Advantages, disadvantages, and impact. AJR Am J Roentgenol .2000;174:617-622.
- Gale B, Safriel Y, Lukban A, et al. Radiology report production times: Voice recognition vs. transcription. Radiol Manage . 2001;23:18-22. Comment in: Radiol Manage . 2001;23:23-25; discussion 26-27.
- Hayt DB, Alexander S. The pros and cons of implementing PACS and speech recognition systems. J Digit Imaging . 2001;14:149-157.
- Atkins MS, Moise A, Rohling R. An application of eyegaze tracking for designing radiologists' workstations: Insights for comparative visual search tasks. ACM Trans Appl Percep .2006;3:136-151.
- Crane K, Branstetter BF, Chang PJ. Does radiologist efficiency have to suffer with speech recognition? Presented at the 91st Scientific Assembly and Annual Meeting of the Radiological Society of North America. Chicago, IL; November 27-December 2, 2005.
- Halpern EF, Sack D, Kirpekar N, et al. Impact of medical imaging informatics on radiologist productivity. Presented at the 93rd Scientific Assembly and Annual Meeting of the Radiological Society of North America. Chicago,IL; November 25-30, 2007.
- Stillman P, Garrett RE, Cooper SA. Quality improvement project to decrease inpatient radiology turnaround time: Experience at Christiana Care Health System. Prescrip Excell Health Care . 2008; 1(2):9-11.
Roundtable Discussion following the presentation:
Speech recognition: Evaluation, implementation, and use
David L. Weiss, MD
ELIOT L. SIEGEL, MD: That was a very comprehensive summary of the topic. If I'm in the process of trying to purchase a speech recognition system, I might hear from some folks that there's really not very much difference from one system to another and they would suggest I buy the one that is most cost-effective. But I might hear from others that there are significant differences and that some of the differences might be an added value beyond the speech recognition. So my first question is whether you believe that there are substantial differences from one vendor to the other with regard to basic speech recognition accuracy rather than the other added value items that the vendors provide? As a customer who's looking to purchase speech recognition, what questions do I ask and what kind of things do I look for?
DAVID L. WEISS, MD: That's a great question. In terms of accuracy, that really is a function of the speech engine, which is the software that turns our words into text. And until recently, most if not all of the speech recognition products for radiology used the same speech engine. That said, there are some differences because they take that basic speech engine, and they modify it with a radiology vocabulary and a radiology speech model. In other words, it's looking for my text in the context of a radiology report.
For example, if I tried to take a radiology-modified speech engine and dictate "Mary had a little lamb, its fleece was white as snow"-and I've tried to do this-it would try to put it in the form of a radiology report, and it would try to use medical terms.
SIEGEL: I guess some of us have had the opposite experience where we'vetried to do a medical report and it comes out "Mary had a little lamb."
WEISS: Well, that's one of the reasons why it's not quite appropriate to buy an off-the-shelf product and use it for radiology, although it's certainly possible. You can train it yourself in terms of vocabulary and syntax to do that.
The other issue is that these speech engines, as I alluded to, learn your voice and your particular way of dictating over the course of months and years. So it's really difficult to evaluate a speech engine in a 1-hour or half-day trial. You're right. There are other workflow issues in which these products do differ.I have noticed a number of those in terms of navigation, in terms of integrating with other types of communication software, including decision support, critical report communication, and things of that sort. So you need to evaluate your own needs in your department. Don't worry about the accuracy so much, although you do want to check that, and then buy the product that suits your workflow the best.
SIEGEL: So a trial period would not necessarily be effective in selecting the best one?
WEISS: A trial period would be helpful if you could do it, but it would have to be a 6-month trial, really, to decide how good the accuracy was going to be. Even then, it's so variable and so subjective that it would be difficult.
SIEGEL: How about the learning curve for speech recognition? You mentioned that we get a little bit more accurate and our productivity goes up a little bit. Is that something I can look forward to by the end of the first day or by the end of the first week? Or is it 3 years or 5 years?
WEISS: The first time I used it, it took me about 4 weeks to get used to it. Interestingly, this correlates with other observations such as the time it takes to get used to changes like holding your fork in the opposite hand. I would say that it's variable for many people and it varies on the basis of, for example, how you dictate. The system is sort of like training a dog. Dogs like the same thing every time. You can't ask a dog do you want to go for a walk? Then ask, do you want to go for a perambulation? They want the same word all the time. They want their dish in the same spot, and they want to eat at the same time. So if you're a radiologist who dictates in the same manner, in the same format for all your chest X-rays, the system is going to love that, because it's going to learn that. If you're all over the map and you ramble here, and then the next study you're dictating something else, it's not going to like that. So the learning curve is going to be much shorter for the radiologist who is concise and consistent.
SIEGEL: Are you significantly faster now than you were 4 weeks into doing speech recognition?
WEISS: Well, marginally so. First of all, I've changed locations, I've changed PACS vendors, and I've changed integration. So that plays a big role in how efficient you are. Not just accuracy. Iwould say I'm about as accurate now as I was before, but I'm not as efficient.
STEVEN C. HORII, MD: I have a question about the way these things operate. We use speech recognition. In the days of digital- or tape-based transcription, I was looking at the images and I would dictate. With speech recognition now, I look at this little screen to see the text coming up as I'm dictating. But there are numerous systems that have a mode with which you can hide the recognition until you're done. I'mwondering, what do you see your colleagues using? Which do they prefer?
WEISS: On most of the systems now, you can either choose to see the screen as the text is coming up, or choose not to see it. The worst thing to do is to actually look at the text as it's showing up on the screen, as it's being "typed." This is partly because there's a delay of a coupleo f seconds after you speak, so it's confusing, but mainly it's not good because your eyes should really be on the images and not on anything else. Your mind should be on the images, too.
I choose to actually have the screen showing. I use a bright color of the screen and I put it off on the third monitor just to remind me that I've turned the microphone on. There's nothing worse than dictating 4 complex paragraphs, and then realizing that you forgot to push the microphone button. So I like t ohave that feedback out of the corner of my eye with color. If I see radiologists staring at the text coming up, I'll recommend that they hide the text while they're dictating.
HORII: I suspect people watch the text because it allows them to catch the errors. So you either correct them on the spot or go back later to correct it. When you go back later to correct it, you know where the errors are because you've seen them come up as you're dictating. Ithink that's why people do it.
WEISS: Probably. That's why it's so important to use macros as much as possible and to dictate as few words as possible. Then you have less to correct.
KHAN M. SIDDIQUI, MD: I have a comment about the macros, and it absolutely makes a difference. A lot of vendors make an effort to show the difference between the macro text and the dictated text. So when you're correcting it, you're looking only at the colored version or highlighted version that you basically put in. It speeds up the correction process. I agree with you 100% that without macros,it can be very challenging to do.
The question that I get asked a lot is when you're doing a speech recognition implementation, how do you integrate your workflow? Should it be based on your speech recognition product's work-list? Or based on the PACS worklist?
WEISS: Or a RIS-driven worklist. My answer to that is that you should use the worklist that is most functional for you. In other words, if you have a great PACS system and an OK RIS and a not-so-good speech recognition product, then you should use the PACS worklist. If your PACS worklist isn't functional, some of the newer speech recognition products offer really nice worklist functionality. For example, many places now are no longer reading off of oneP ACS; they have their original PACS,then they've acquired another hospital, and they're reading from an imaging center, so they have 3 or 4 or 5 different PACS worklists. The speech recognition products coming out now can unify that into more of a communication package. So you could read from the speech worklist, and it will pull different images and different demographics from multiple PACS.
SIDDIQUI: One thing I've seen is that people make decisions to purchase purely on the accuracy of the speech recognition of the system. But a lot of the products out there actually provide a lot of workflow-enhancing features. Personally, I think people should consider looking at how it impacts their productivity in terms of which tools are available in the product rather than just the speech recognition part of it.
WEISS: Exactly. It's a mistake to purchase a product because of what you perceive the accuracy will be based on a 1-hour session, a half-day session, or even a demo, if they leave you a demo copy for a day. It's going to change. It's like a violin. You buy a violin, and if it's a good one, it will sound different a year from now after you've played it than it does as a new product. It's the same with this product.
PAUL G. NAGY, PhD: You showed a large gulf between your bimodal distribution, between people who choose to use it >90% of the time and people who choose to use it <10% of the time. What would you describe as their major demographic difference? Would it be their gender, their nationality, their age, or just their technological sophistication?
WEISS: None of those. It's interesting, but there really isn't a correlation between age and use. Someone asked once whether the people who use it are less productive or more productive? When I look at that, actually the people who use it more are more productive.It's like the old adage; if you want something done, give it to the person who's the busiest. It's all over the map.
NAGY: So infrequent users have the hardest time with it?
WEISS: Well, it's a self-fulfilling prophecy. If you don't use it exclusively, you will not learn it. I think the fact that we made it voluntary means that those people who are hesitant to use the product will never get better at it. They're not going to swim if they're never thrown in the water. I have not substantiated this, but I think some radiologists are a little hesitant to dictate a report and then sign it right away and have it sent immediately to the referring provider. Then they may say 3 minutes later, oh gee, I forgot to mention the gall stones!
NAGY: So we should have a little "whoops" button?
WEISS: You could have a delay in that. We don't in our product, and I wonder whether that's the issue. The other issue is that of the 3 systems we have, the speech recognition is the only system that allows everybody to see your productivity at any given moment. I think some radiologists may be hesitant about other people seeing how many studies they've read in the last 10 minutes. Youlook at productivity by the month in the RIS, you can look at it to some extent in the PACS, but this will show you clear as day. You can go in and see what the guys next to you are doing. I think all of those things are unspoken impediments to people using the product.
SIEGEL: Thanks for a great presentation and a great discussion.
Mr. Hafey is Chief Architect, Vital Images, Minnetonka, MN.
Bringing advanced visualization to the healthcare enterprise offers an incredible opportunity to enhance patient care and improve efficiency. A goal of this magnitude is not without challenges, however. To understand the challenges facing advanced visualization, it is essential to appreciate the rapid rate of change in computed tomography (CT) scanner technology. Next-generation scanners-those with >64 slices-represent only a tiny percentage of the CT market today, but they are expected to capture an increasingly larger market segment in the next few years.
The enormous amount of data generated by advanced CT scanners creates several issues that must be accounted for. First, advanced CT enables new applications that weren't possible before. Second, such applications are driving the need for enterprise-wide access. Third, distribution of data and clinical applications to the enterprise must be managed more efficiently than in the past. Otherwise, the data boom will overwhelm healthcare networks.
As new scanners bring more data to the picture archiving and communication systems (PACS) and to radiologists, there is an increasing need for advanced visualization, so that the data can be understood and interpreted. There is also a need to change the way data are handled on the back end and presented to the end-user.
One of the most significant ways to address these challenges is to transition from a sole focus on stand-alone workstations to enterprise deployment. Advanced imaging capabilities can be made accessible throughout the enterprise through a combination of thin-client, Web-based, and remote-access technologies, in addition to traditional thick-client workstations.
Key components
There are 5 key components of an effective enterprise-wide advanced visualization system: advanced technology, volumetric data management, partnerships, professional services, and performance.
Advanced technology
Several core technologies enable distribution of advanced visualization to the enterprise. The first is graphics processing unit (GPU)-based rendering. A few years ago, GPUs were available only on high-end workstations. Now they are a standard feature in virtually every PC. Graphics processing units are getting faster and better, with advances mainly driven by the gaming market. Harnessing this power is key to bringing advanced visualization to the enterprise.
Volumetric data management
To efficiently scale up to the enterprise level and provide the performance that users expect, it is necessary to stop handling data on a slice-by-slice basis. Rather, we must focus on volumetric representation. Volumetric representation makes the system more scalable, increases its speed, and provides a more consistent user experience.
Volumetric data management also influences how data are handled inside the computer itself. A key innovation in the microprocessor industry is the use of multiple cores. Today it is fairly common to buy a PC with 2 or 4 cores. In a few years, computers may have 64 or 128 cores.Through the use of optimized multicore algorithms, advanced visualization and volumetric imaging can harness the power of multicore technology as part of a volumetric data management strategy.
Partnerships
Partnerships and relationships are another key component in bringing advanced visualization to the enterprise. It is critical for vendors to partner with the technological leaders in each industry and to tie them together in a way that creates a high-performance, powerful solution. For example, Vital Images (Minnetonka, MN) has developed a number of technology partners. NVIDIA (Santa Clara, CA), a Forbes 2007 Company of the Year, is the leader in GPU technology. Intel (Santa Clara, CA) was the first microprocessor vendor to introduce multicore technology. Microsoft (Redmond, WA) offers the latest in Web services. HP (Palo Alto, CA) is the world leader in server technology.
Business relationships are also key. Toshiba America Medical Systems (Tustin, CA), for example, is a leader in developing volumetric CT scanning. McKesson (San Francisco, CA) is a recognized industry leader in medical information technology solutions.
Professional services
Access to professional services from the vendor is also critical to the success of advanced visualization. These services should maximize system performance and should include system planning, installation, integration, workflow optimization, and education. An advanced visualization vendor must have a professional services team dedicated to solving customers' problems, whether they purchase a turnkey solution or prefer a customized solution that necessitates system modifications before deployment.
Education is a key aspect of professional services. Not all advanced visualization techniques are intuitive; therefore, understanding the technology and how it works is essential. Vendors must commit to training users to make the most of advanced visualization. Users who can use the system effectively are essential for its successful deployment in the enterprise. Vendor educational services can come in many forms, including on-site learning, classroom learning, distance learning, and online learning. Education must be optimized to meet the customer's needs.
Performance
This is the fifth component of an effective enterprise-wide advanced visualization system. Customers who want the best possible system performance must ask vendors several questions, including: How are systems installed? How are upgrades handled? Are there test systems? Is there access to engineers who can immediately resolve issues? These are all issues that must be addressed when considering taking advanced visualization to the healthcare enterprise.
Conclusion
Considering these key components when incorporating advanced visualization to the enterprise ensures a flexible solution that is supported by broad clinical applications, efficient data management, and consistent performance.
Mr. Cooke is Vice President of the Net work Business Unit at FUJIFILM Medical Systems USA, Inc., Stamford, CT.
The Internet has revolutionized the delivery of many products and services. As a service, radiology has taken part in the Internet revolution. For example, radiologists once primarily worked on-site in hospitals. Today, ambulatory care is increasingly common, often separating the radiologist from the patient. As a result, remote image interpretation is now routine, and it is common to distribute soft-copy images across the health-care enterprise. These trends create the need to image-enable thousands-if not tens of thousands-of desktops throughout an integrated health-care network-many of which are outside of the walls of a hospital.
Consumerism is another critical trend that is being fueled by the Internet. Today patients have easy access to a wide range of medical information and are able to educate themselves about radiology processes. As a result, they demand a high level of service, including rapid turnaround of imaging reports.
Finally, the Internet may also be playing a role in the shortage of radiologists, as some elect to work in the computer technology industry. An estimated 380 million radiology procedures will be performed in 2008, representing an annual growth rate of 14%. The number of radiologists is growing at an annual rate of just 1.2%. Under these challenging circumstances, it is essential that we maximize radiologist efficiency, so that the quality of care can remain high.
PACS redefined
In 1999, a picture archiving and communication system (PACS) was easy to define. It consisted of a diagnostic workstation, a list of unread studies, and digital departmental storage. It was simply a system that enabled soft-copy interpretation of images. In essence, the computer replaced the light box.
Today, defining a PACS is anything but simple. In addition to remote reading, we are faced with new imaging modalities that generate very large data sets with an increasing amount of dynamic and functional content. As multiple healthcare institutions come together to form integrated delivery networks, they create multisite workflow for the radiologist and others involved in patient care. There is an increasing amount of information available to drive workflow and guide decisionmaking, but it must be navigated in an efficient fashion.
In addition, with the push toward the electronic medical record, users are looking for portable, mineable forms of data storage. They also want enterprise access to images and information, not just in radiology but also in such clinical areas as cardiovascular medicine, pathology, mammography, and others.
All of these trends create questions about what a PACS should look like. As we consider this question, we should be thinking about workflow, visualization, and infrastructure. As an industry, we must think of a PACS not as a monolithic system, but rather as a platform and an infrastructure for storage of data from multiple clinical areas, as a separate platform for visualization, and as a tool for overcoming workflow challenges.
Integration
Radiology studies often traverse many boundaries. A large hospital may be served by a single radiology group, which, in turn, may be covering multiple different large-scale facilities as well as a small hospital that is struggling to retain radiology services. The radiology group may also be outsourcing some of its work to a nationwide reading service or so-called super group.
A typical radiologist reads on ≥6 different PACS systems. This translates into at least the same number of platforms for 3-dimensional (3D) visualization, the radiology information system (RIS), and the reporting system. The need for radiologists to switch between various user interfaces creates both a great challenge and a great opportunity for integration.
For example, the mandate to maximize radiologist efficiency creates the opportunity for a new kind of integrated worklist that takes into account all of the healthcare sites the radiologist serves and brings together a variety of tasks ranging from report signing to peer review to protocoling of examinations. By drawing from combined user preferences and workrule logic, this information can be presented in a dashboard format for navigation by the radiologist (Figure 1). Combining diverse systems into a common worklist/dashboard allows a radiologist an integrated view of the work he or she has to perform.
Once the radiologist gets to that work, it is very important to have the right kinds of tools available, including advanced visualization. These tools need to be integrated not only into the PACS for use in normal day-to-day operations, but also into other applications, given that new kinds of viewing models will be incubated outside of the PACS in many cases.
These tools also need to be distributed, because diagnosis is now distributed. Radiologists should not be constrained by the limitations of the environment in which they serve. All necessary information and tools need to be accessible in a way that facilitates efficient and ergonomic interpretation. In addition, our systems must be able to provide, at a minimum, a collaborative connection between the radiologist and the clinician.
Internet
It is interesting to visualize how all of these demands might play out in the future and what impact the Internet will have (Figure 2). Hospitals may seek a common infrastructure for radiology, cardiology, mammography, and other specialties-one that integrates images, structured reports, documentation, and medication history into a decision support system. The desire to integrate various imaging modalities into a common infrastructure may be a reason healthcare institutions are looking to replace their PACS.
They may also be looking to replace their radiology information system and other technologies as a way not only of improving workflow but also of maintaining their physician base. Referring physicians may demand online interactive scheduling, order entry, critical results alerts, advanced visualization, and decision support-and hospitals may seek to provide these services as a way of retaining their relationship with physicians.
Certainly radiologists are starting to invest in technology platforms that help them gain a competitive edge through more ergonomic and efficient interpretation, access to prior studies, results generation, diagnostic visualization tools, and decision support.
Better communication with patients is also an important emerging opportunity. Interaction with physicians, education, and results reporting can all be facilitated by the Internet.
Conclusion
A unique opportunity exists for our industry to connect all healthcare stakeholders through the use of Internet technology. We must act quickly, as technology is changing at Internet speed.
As vendors, we must define our goals and deliver value. We must open our systems and enable integration opportunities without creating technology stagnation. We must continue to collaborate with stakeholders in the healthcare industry. We must continue to adapt and exploit consumer technologies. Perhaps most important, we must "humanize" radiology by involving the patient, involving the referring physician, and putting a human face on the radiology process.
REFERENCES
- Caesy S. Keynote speech: The impact of the Web on radiologist shortages. Presented at the Digital X-Ray and PACS: An Educational Forum. Scottsdale, AZ; February 26, 2005.
- Forman HP. Radiologists' salaries: Should we worry? AJR Am J Roentgenol . 2007;189:755-756.
- Sunshine JH, Meghea C. How could the radiologist shortage have eased? AJR Am J Roentgenol. 2006;187:1160-1165.
- Meghea C, Sunshine JH. Retirement patterns and plans of radiologists. AJR Am J Roentgenol. 2006;187:1405-1411.
- Licurse A, Saket DD, Sunshine JH, et al. Update on the diagnostic radiology employment market: Findings through 2005. AJR Am J Roentgenol . 2006;187:W249-W254.
- Batchelor JS. Rad workload shows double-digit increase. September 22, 2005. Available on the Aunt Minnie Web site: http://www.auntminnie.com/index.asp?Sec=sup&Sub=imc&Pag=dis&ItemId=67815. Accessed May 2008.
Panel discussion
Moderator: Eliot L. Siegel, MD
ELIOT L. SIEGEL, MD: Thank you very much for your talks, Bob and Chris. They were really both interesting and provocative. I'd like to start out on something that Bob mentioned- ergonomics as a buzz word. If you take a look at the definition of ergonomics , it comes fromthe Greek word ergon , meaning "work,"and from nomos , which is "natural laws." Most people think about the physical and physiologic aspects of ergonomics. But it's a lot more than just office furniture. Ifyou take a look at the definition by the International Ergonomics Association, they say that there are 3 subtypes. One is organizational, which we'll set aside for just a moment. The other is physical, which is the one that most people pay attention to. Then the third one is cognitive. Cognitive ergonomics actually focuses on human perception, human attention, cognition, motor control, memory storage, and retrieval. I'd like to ask both of you, in terms of things like perception and attention and cognition, where do you see next-generation systems going? Given that definition of ergonomics from a cognitive perspective, what are you doing with your companies to try to help us radiologists? We're feeling increasing stress; we've talked about how many studies we're reading out. We've done some work in our reading room to try to make a nice environment as far as the lighting, sound, and ventilation. But what are you doing to minimize my stress from a cognitive perspective,and to help in terms of designing your systems? How are you approaching that?
BOB COOKE: If you look at the cognitive side, there are some very simpl low-hanging fruit that we're facing right now in terms of alignment of human interfaces. We all talk about integration as being very good; however, if you move from one user interface scheme to another, there are all huge opportunities for improvement in terms of the way the mouse moves, the way the icons work, the color schemes of the application. These context switches between user interfaces slow people down and I think they also add stress during your work day. So very simply, in terms of even our product design, we're seeking to align our user interfaces and focus more on color schemes that are more comfortable. We should try to take advantage of these colors, because, as Ithink one of the presentations mentioned, more and more monitors are now color. There are some great opportunities to use color to flag a critical result or to flag a critical task that might be upon you. I think this is really the first area that we have to focus on as an industry, to look at alignment of user interface design, and the color schemes that are associated with those user interfaces.
SIEGEL: Dr. Weiss mentioned tha the really strongly prefers and recommends that we spend as much of our time looking at the images rather than looking at the reports as they're being generated. I'd like to expand on that from my perspective as a radiologist. I'd like to look at the images as much as possible and spend as little time as possible looking at pull-down menus or icons. SoI would love to see that as part of the ergonomic solution also. Chris, how are you dealing with that?
CHRIS HAFEY: Vital has always been very focused on usability and what we call read flow, or the minimum number of clicks to actually deliver what the user wants. We spend an incredible amount of time on it, mainly because there are so many opportunities to actually improve the read flow and the way the system works. I think it's unique in the sense that advanced visualization has such rich data to actually automate things. By putting time into this, working with users, and developing algorithms, we're able to make it as simple as opening an exam orstudy, drawing an arrow, and being done with it.
SIEGEL: Have you been tempted to incorporate some PACS functionality into your advanced visualization solution, for example, the ability to mark a study as dictated or to integrate it with areporting workflow?
HAFEY: We do have a reporting module in our system that functions a little bit differently than traditional radiologywork flow. It has some capabilities similar to that, but it's actually a bit more patient-focused in the sense that a lot of the output result is targeted as somethingy ou can give directly to a patient, specifically in cardiology, but in radiology, too. Taking things like internal findings that we find in the system, capturing them in a way that is understandable to a user,and even reusable in the system in the future, when we load up maybe a follow-up case, for example.
DAVID L. WEISS, MD: I'd like to expand on the question Eliot asked regarding keeping the radiologist's eyes away from any pull-down menu and, even more importantly, away from glancing at the keyboard to enter data or make a request. On the 3D side, the conventional mouse now is becoming inadequate in terms of a 3-dimensional image. There has been some work with a 3-dimensional mouse. What are your companies doing to incorporate some of those mechanical devices or even new mechanical devices and concepts into the reading process?
SIEGEL: In addition to just mapping those devices out to equivalent mouseclick functions, but taking advantage of a greater level of increased freedom?
WEISS: Yes, or even more so. All of those devices were created to match software, and then software was created to match those arguably flawed devices. How about doing what the folks at Apple did, in creating new hardware and new software matched to each other? In other words, throwing everything out and starting over? What are your thoughts on that?
COOKE: I think we've got to breakdown a couple of different topics here. Let's first look at the issue associated wit hkeeping your eyes on the images. As radiology transforms itself from detection and diagnosis to also now being involved inthe follow-up, communication, and collaboration with the physicians ordering the exams, dealing with critical results and with that communication and collaboration may require you to have notifications and alerts inside of your diagnostic process that require you to be involved.
Obviously from an ergonomic perspective, you should be in control of when those things pop up and when they don't. But from time to time, it may be important that those issues pop up. They may have to interrupt your reading process much the same way that somebody comes and taps you on the shoulder toi nterrupt you during your normal reading process.
The second thing is in terms of the 3D mouse. Obviously, incorporation of basic 3D functions into the diagnostic workflow is mandatory. In general, there are some great opportunities for PACS systems and advanced visualization technologies to come together to at least enhance the diagnostic process as it relates to comparisons and synchronized ways to look through stacks of thin-sliced data. I think there are some great opportunities there.
In terms of integration with these external devices, one of the nice choices we made early on in developing our system was to take advantage of off-the-shelf operating system technologies and be able to link these kinds of mouseclicks to operations within our system. So our users are routinely using 7-button mice for short-cuts, and mammographyusers are quite routinely using that shuttle device that you mentioned.
SIEGEL: How about Vital, Chris? Are you looking at other alternative input devices to a mouse or track ball?
HAFEY: Well, being on the engineering side, we absolutely love to look at these things. They are exciting and interesting, and we think of all sorts of interesting novel applications for them. None of them have actually passed the usability test on the user side to actually drive production. The other side of that is we've been very successful with our automation algorithms to remove a lot of the manual efforts of looking at these cases. We can quickly get the user to point where they want to see exactly what they're looking for.
SIEGEL: You mentioned the importance of training and the fact that there is training available for the radiologists locally on-site. But we have thousands of users, potentially, at the University of Maryland or Department of Veterans Affairs. Do we have somebody train each of them? Or have you looked at computer-based training or online training possibilities as we move from the radiology department to the entire enterprise?
HAFEY: First of all, I would love to have our product be so usable that no training is required at all. So you could walk in and immediately start getting value out of it.
SIEGEL: Like a video game.
HAFEY: Like a video game, absolutely. I think, actually, the video game industry is a fantastic model to learn about how they take a very complex situation, like an online role-playing game. They engage the user who can have success early and then later on become much more advanced and they can pull capabilities out of it.
SIEGEL: They don't have to have a trainer come by your house to train you rkid how to use a video game or even expect him or her to read the user's manual.
HAFEY: Exactly. I think those types of paradigms are important to us. We do actively think about how can we anticipate what the user might want to do, make it very evident and clear to them, so they don't have to go to the help manual. So they can walk into it without ever having any experience and still get value out of it. That being said, that's primarily focused at a lot of what used to be advanced and is now basic visualization. There are still advanced things that require not just usability, like how do I use the application, but clinically, what does this mean? What is this procedure about? There are new procedures being invented with these new scanners that require education, because you didn't learn it when you went to school.
STEVEN C. HORII, MD: I actually have a comment about the gamers. If you think about it, in some of these games you're operating in 3D space, and you'vegot 6 degrees of freedom. You have translation in 3 dimensions and rotation. Yet, the gamers do this. They fly around,s hoot down enemies, and do all kinds of manipulation things all at the same time. They have an intuitive user interface, and it's certainly something that kids can grasp. We had an experience recently when looking at a training issue and determined that when using an advanced visualization system, a static paper manual is not good enough. You really need to see how you interact. We had an undergraduate working for us who found some available software that allows us to capture all of the interaction as a movie. Then we can save it as an AVI file or whatever. So we have built a whole set of dynamic instruction files that go along with the paper manual. You can look up a task: how do I do a colon fly-through? It will show you. How did I do? We recorded an expert doing it and we can insert a voice-over it to create a little instruction video. We've posted those on our Web site. We were looking at our training, and it all came out of work with this young undergraduate in biomedical engineering who figured this out.
SIEGEL: You're looking at undergraduates. Dr. Chang and Paul Nagy mentioned they are scouting ever earlierat the high school level!
HORII: Yes, but it's probably not a lot different in terms of what they knowa bout systems.
KHAN M. SIDDIQUI, MD: I have a comment on what Chris suggested earlier. One of the frustrations I have reading cardiac CT and cardiac MR cases is that the available reporting solutions on workstations are designed for cardiologists. Cardiologists love the idea of getting a report ina structured format. But then I also have to incorporate that report into my radiology information system (RIS). So, a lot of times, I'm doing duplicate reporting, one for cardiology based on the templates that are available in the cardiac workstation, and then again on the RIS. Is there any effort to integrate the reporting systems so we just have to report once using speech recognition? There is hardly anybody doing integration of advanced workstations with speech recognition systems to take advantage of reporting flexibility. IfI'm reading cardiac CTs all day long on the workstation, because I can't do it on PACS, how do I look at prior studies? How do I look at prior reports? Currently Isee a lag in existing technologies that can provide unified workflow. Can you comment on the future of how to integrate reporting and how to make the workflow much more feasible when you compare prior studies and prior reports from contextually relevant other studies?
HAFEY: That's a great question and there are multiple aspects to it. First of all, advanced visualization has traditionally been volume-focused, not longitudinal orcomparator review-focused. There are definitely some very exciting opportunities in advanced visualization that you'll see more of in the future. One of the challenges, though, is who does comparator review? It's the PACS system. There's a disconnect in the interface between PACS and advanced visualization. At best, what we can do is get launched by URL with a patient ID. So I think yo uneed to create a tighter integration between the two so we can get context about what priors are available for this patient. Taking the advanced position, next step, then we look for the findings in those priors and how they relate to current procedures. Then we actually try to augment even further. There are an incredible amount of opportunities there.
In the report data itself, there are a lot of opportunities to get more up to speed with current IT infrastructure in terms of HL-7 and getting reports out and interfacing them to the RIS. We have developed technologies to expose our internal data structure to Web services. These are not difficult to do. It's a matter of people wanting to do it and pushing it through. A number of customers are doing that right now.
PAUL G. NAGY, PhD: I have a question. There are large cultural differences between radiologists, physicians, and IT developers. Sometimes we see this in the products, in that some products might not make sense or upgradesmight have issues. So what efforts do you take to put the radiologists into the mind of a developer?
COOKE: As an example, forums like this are extremely valuable and critical. The good news is the human body is the same across the world, and the good news is that most radiology practices, believe it or not, around the world, ar every similar in the way exams are interpreted. On one hand, as a global developer, we have a great opportunity in terms of interaction with our users and not having to worry about designing multiple different systems to solve multiple different problems. We're really only solving one problem, which is the good news.
The second thing is that you have to think about it from a couple of different perspectives. Obviously, the radiologist needs to generate a quality result and struggles with keeping quality and efficiency. Then there's the radiologist who is a business person trying to advance his or her practice. We have to interact with each and every one of those kinds ofroles. In some cases, they're all thes ame; in many cases, they're different sets of players. For example, we recently went down to one of our large readingg roup users and we spent the weekend essentially working with their radiologists, looking at the whole "click-ology"to try to remove clicks from the process. We looked for opportunities for automation to determine how we could improve the efficiency.
We're all talking about how advanced visualization can be incorporated into the diagnostic process. That's great and will help with efficiency. But, at the end of the day, there's still a whole lot of stuff right inside your basic PACS that are also great opportunities for efficiency improvement.
SIEGEL: How does Vital handle that challenge?
HAFEY: I'd say a big part of the success there is culture. You have to hire developers and train them. You have to establish a culture that says it's important to understand the end-user and to go above and beyond to get there. We sendo ur developers on-site on a regular basisto talk to users, get feedback, see what's going wrong, and see how are they working. We also have an extensive output program, so as we develop new features, we develop agile methods to get the best result possible. In the end, I think you're taking a world that is extremely complex-the radiology informatics area-with another world that is extremely complex-technology. You just need to have the right developers on staff who will go home at night and keep up on the latest technologies, read Aunt Minnie, and understand what's going on.
SIEGEL: Thanks. I'd like to thank all of our participants for an incredibly interesting discussion, and for underscoring the tremendous importance of imaging informatics, both in the way we practice radiology today and in shaping the future of diagnostic imaging. Thank you all very much.