Imaging of elbow pathology


















Dr. Bancroft is an Associate Professor of Radiology, Dr. Berquist is a Professor of Radiology, and Dr. Peterson is an Assistant Professor of Radiology, Mayo Clinic, Jacksonville, FL. Dr. Kransdorf is a Professor of Radiology, Department of Radiologic Pathology, Armed Forces Institute of Pathology, Walter Reed Army Medical Center, Washington, DC.
The opinions or assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the Department of the Army or the Department of Defense.
The evaluation of elbow pathology continues to advance, in part because of improved diagnostic imaging techniques. These improvements have assisted the radiologist in providing more accurate diagnoses and, therefore, better patient care. A variety of imaging modalities may be used for the evaluation of the elbow, depending on the indication and suspected disease process. This article will provide an overview of the imaging characteristics of some disease processes that can affect the elbow, such as trauma, arthropathy, and infection.
Imaging modalities
Most evaluations of the elbow begin with radiographs because of their screening value and relatively low cost. Lateral and anteroposterior (AP) radiographs are essential in the basic evaluation of disease. Oblique radiographs or additional views, such as the radial head view, may be utilized for further evaluation of occult trauma or early arthropathy.
Advancement in technology has allowed multiplanar imaging with multidetector computed tomography (MDCT). Mulitdetector CT is a quick means to acquire volumetric imaging data that can then be reconstructed in an infinite number of imaging planes, including 3-dimensional volume and surface renderings. It is possible to perform a single scan with thin slices that consist of near-isotropic voxel dimensions. 1 Osseous structures are best evaluated using "bone" algorithm reconstructions, whereas soft tissues and surface-rendered images are better generated in a "standard" algorithm. 1 In the presence of metal in the postoperative elbow, increased kVp and mAs will help decrease metal-induced streak artifact. 2
Magnetic resonance imaging (MRI) of the elbow can clearly define normal bone, soft tissue anatomy, and pathology. 3,4 Dedicated circumferential elbow surface coils, small field of view (10 to 12 cm), and high-field-strength magnets provide optimal image quality. Image planes and field of view for the elbow vary with study indication and include axial, sagittal, and coronal; oblique and reformatted thin-section gradient-echo images are optional. 3-6 The axial image plane is useful to assess neurovascular, tendon, and muscle anatomy. The sagittal plane is useful as a second plane for biceps and triceps tears or to define the extent of a lesion identified on axial images. The coronal plane is useful for evaluating articular surfaces, common extensor and flexor tendons, and collateral ligaments. 3,4 Methods for decreasing metallic susceptibility artifact in the postoperative patient include increasing the bandwidth, aligning the metal along the long axis of the magnet bore, utilizing fast spin-echo sequences, avoiding fat suppression, orienting the frequency- encoding direction along the main longitudinal axis of the implanted hardware, and increasing the frequency-encoding gradient strength. 7,8
Elbow arthrography-either conventional, or followed by CT or MRI-is helpful in diagnosing capsular and ligament tears, osteochondral lesions, and loose bodies when there is no joint effusion. 4,9-12 The elbow can be injected laterally (radiocapitellar joint) or posteriorly with 8 to 12 mL of solution. Using a 50% diluted iodinated contrast solution for CT arthrography should not obscure small loose bodies. A 1:250 diluted gadolinium solution that contains 50% lidocaine/bupivacaine and 50% iodinated contrast can be used for MR arthrography. Following injection, T1-weighted (T1W) fat-suppressed images are obtained in the axial, coronal, and sagittal planes. In addition, a fast spin-echo (FSE) T2-weighted (T2W) fat-suppressed (FS) sequence is obtained for the detection of marrow abnormalities, soft tissue lesions, or fluid collections.
Sonography is useful in evaluating a variety of structures, such as the common extensor and flexor origins, collateral ligaments, nerves, and bursae. 13-17 Medium- (7.5 MHz) or high-frequency (12 MHz) linear array transducers can provide high-resolution images of the periarticular soft tissues. 14,17 In experienced hands, this modality has been proven to be quite accurate.
Nuclear medicine imaging is occasionally used for imaging elbow pathology. Bone scintigraphy with technetium-99m methylene diphosphonate ( 99m Tc-MDP) is helpful to identify areas of active bony turnover and reparative processes. Combined 99m Tc-MDP and indium-111 111 In)-labeled leukocyte scans can be useful in the detection of infection, and fluorine-18-fluordeoxyglucose (FDG) positron emission tomography (PET) imaging can identify foci of hypermetabolic activity in cases of tumor, inflammation, and infection.
Osseous trauma
Elbow fractures and other injuries are common in infants, children, adolescents, and adult throwing athletes. 6,18-22 Routine radiographs and CT are generally sufficient for the detection and classification of skeletal injuries. However, it is not uncommon to detect occult skeletal injuries with MRI that were overlooked or were not identifiable with conventional techniques. 3 In children, supracondylar humeral fractures account for 50% to 60% of all fractures and have high complication rates. 22 Physeal fractures are also common in children and adolescents, with the majority of injuries occurring between 4 and 8 years of age, when epiphyses are not well ossified. 22-24 Fractures of the lateral condyle are most common, accounting for >54% of fractures. 23 "Little leaguer's elbow" typically occurs in 9- to 12-year-old baseball pitchers, and represents avulsion and fragmentation of the medial humeral epicondyle due to repeated valgus stress from the flexor and pronator muscles across the growth plate.
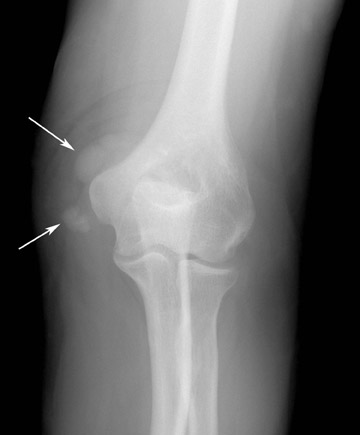
The radial head fracture is the most common elbow fracture in adults. Trauma evaluation should begin with radiographs (Figure 1) but may be supplemented with CT or MRI. Imaging features that affect patient prognosis include the degree of comminution, angulation, and depression of the radial head fracture. CT may be useful in evaluating the articular congruity of the radial head, especially after reduction (Figure 2). MRI is very sensitive for the detection of occult fractures (Figure 3), either in the marrow or physis. 23 Marrow edema or bone contusions are low in signal intensity on T1W images. Fractures are evident as hypointense lines within the marrow if there is trabecular compression and discontinuity of hypointense cortical bone.
Radial head fractures can be classified by the Mason Johnston classification system. 25 Type I include nondisplaced fractures. Type II are minimally displaced fractures with depression, angulation, and impaction. Type III fractures are fractures that are comminuted and displaced. The most severe, Type IV, are radial head fractures that are associated with dislocation of the elbow. In cases of extensive comminution of the radial head, radial head resection is usually performed, allowing for resumption of pronation and supination. Occasionally, radial head prostheses are placed in the attempt to gain function. However, these implants are prone to fracture, may dislodge, or may cause synovitis (Figure 4).
The capitellum is less commonly injured than the radial head. Fractures often occur from valgus force, with impaction of the radial head against the capitellum (Figure 5). One known imaging pitfall is the pseudodefect at the junction of the capitellum and lateral epicondyle, which is actually a normal osseous groove. 26 The pseudodefect deepens as images proceed more laterally, and occasionally 1 or more fine, low-signal lines extend from the pseudodefect into the marrow.
In adults, dislocations of the elbow are second only to those of the shoulder in frequency. In children, it is the most common dislocation. Simple posterior elbow dislocations usually result in complete disruption of all of the capsuloligamentous structures, with variable adjacent muscular injury. 27 Persistent instability after closed reduction of a simple dislocation may be secondary to soft tissue interposition or entrapment of an intra-articular chondral or osteochondral fragment. 27 MRI and MR arthrography may assist in diagnosis in these circumstances. Fracture-dislocations take various forms in the elbow and forearm. The Monteggia fracture-dislocation is composed of a fracture of the proximal ulnar and a dislocation of the radial head (Figure 6). Care must be taken not to overlook subtle subluxations or nondisplaced fractures with this injury pattern.
Tendons
Biceps tendon
Radiographs may exhibit irregularity of the radial tuberosity in chronic biceps tendon injuries, obliteration of the supinator fat stripe, or, rarely, acute avulsion fractures. 22 MR imaging is ideally suited to evaluate injuries of the biceps tendon. T2-weighted, gradient-echo, or short tau inversion recovery (STIR) images are best for showing the high signal abnormality of hemorrhage as well as the inflammation and fluid seen against the normal low signal intensity of the tendon. 27-30 The distal biceps tendon is the most commonly injured tendon in the elbow. Ruptures of the biceps tendon (Figure 7) account for only 3% of biceps injuries and are most common in men >40 years of age. 28-31 Injuries typically occur at or near its insertion into the radial tuberosity as a result of forced hyperextension with the arm flexed and supinated. 32 Tendon ruptures are characterized by complete discontinuity of the tendon, increased intratendinous signal, peritendinous fluid/hematoma, and muscle and tendon retraction. 28,29 The tendon does not retract if the bicipital aponeurosis (lacertus fibrosis) remains intact. Partial tears (Figure 8) are visible on MR as thinning, increased intratendinous signal, peritendinous fluid, and, occasionally, a proximally thickened tendon. 30
Triceps tendon
Although inflammation of the triceps is fairly common, ruptures of the triceps tendon are rare (Figure 9). 22,33 Radiography is useful in evaluating triceps injury, since up to 80% of patients will have avulsion fractures of the olecranon. 34 Inflammation in the muscle or tendon is evident as irregular areas of increased signal intensity on fluid-sensitive MR images. Complete disruption results in areas of high signal intensity separating the low-intensity tendon fragments. 29 The triceps tendon normally has striations of increased signal that insinuate between the distal tendon fibers and should not be mistaken for tears. 3
Common extensor and flexor tendons
Tendinopathy or tears of the common extensor and flexor tendons can be evaluated with MRI or sonography. 3,35 Typically, imaging studies are not performed unless the patient has failed conservative treatment. 24,35 In patients with lateral tennis elbow, the primary site of involvement is the common extensor tendon origin. MRI reveals thickening and intermediate signal within the tendon origin in cases of tendinopathy. Partial tears are depicted by thinning or partial disruption of the tendon, and increased T2W signal within and adjacent to the tendon origin (Figure 10). Complete rupture of the tendons will lead to a tendinous gap containing fluid signal, and distal retraction of the involved muscle(s). Dystrophic calcifications can arise adjacent to the lateral epicondyle and are best depicted on gradient-echo images. 36 Lateral epicondylitis is evident as a focal hypoechoic area in the deep part of the tendon or a discrete cleavage plane with sonographic evaluation. 11
Injuries to the common flexor tendon origin (golfer's elbow or medial tennis elbow) (Figure 11) are less common than injuries of the common extensor tendon origin. 22,33 Common flexor tendon injury occurs at the origins of the flexors and pronator teres. 22,31 This syndrome occurs in 1% to 3% of adults who are 35 to 55 years of age, and it is often seen in golfers, high-performance throwers, swimmers, racketball and squash players, and bowlers. 4,24 MR arthrography has been advocated for the detection of partial tears. 22 The diagnosis of partial tears is critical to throwing athletes, because these patients will likely undergo surgery. 22
Ligaments
Radial (lateral) collateral ligament complex
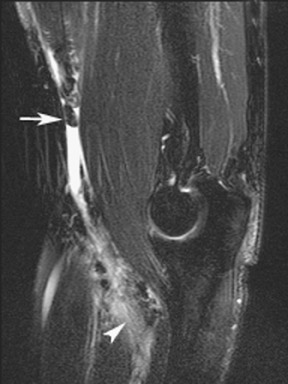
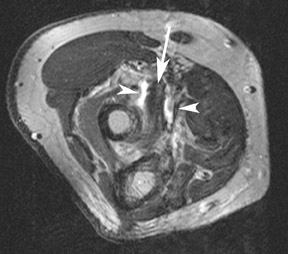
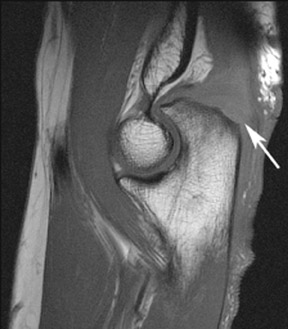
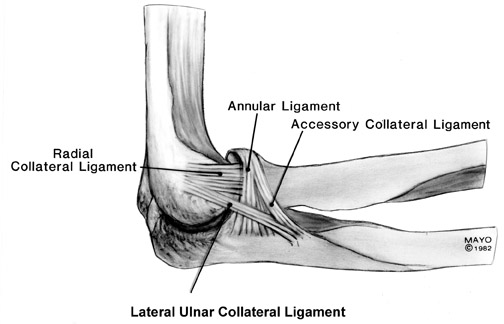
Additional support for the elbow is provided by the radial and ulnar collateral ligament complexes. 22 The radial (lateral) collateral ligament (RCL) complex is composed of the lateral ulnar collateral ligament, RCL proper, and the annular ligament (Figure 12). 37 Injury to the RCL complex (Figure 13) is less common than medial ligament injury and is usually the result of varus stress or subluxation/ dislocation. Overly aggressive surgical procedures, such as common extensor tendon release or radial head resection, can also lead to radial collateral ligament injury. 24 The lateral ulnar collateral ligament is the primary stabilizer against varus stress, and its disruption (Figure 14) can lead to posterolateral rotatory instability of the elbow. 19,38 The radial collateral ligament proper attaches to the annular ligament; therefore, both structures should be evaluated critically.
Ulnar (medial) collateral ligament complex
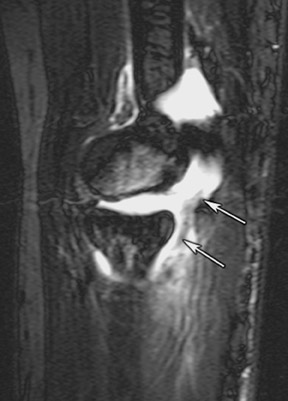
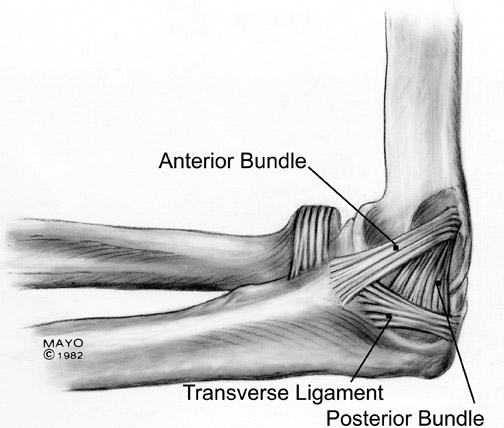
The ulnar (medial) collateral ligament consists of 3 bands and is much stronger than the RCL (Figure 15). The anterior band is the dominant structure and the primary stabilizer against valgus stress on the elbow. 39 It courses anteriorly from the anteroinferior surface of the epicondyle and attaches to the medial edge of the coronoid process. The posterior band is smaller and has a fanlike configuration. 10 It extends from behind the medial epicondyle and courses slightly posteriorly to attach onto the medial aspect of the olecranon. The transverse band is clinically less significant, is smaller or sometimes absent, and is often difficult to identify on MR. 3,4,10 Acute ruptures are not a diagnostic dilemma and are seen as discontinuity and an abnormal course of a ligament. Partial tears (Figure 16) are more difficult to diagnose with imaging; articular-surface tears are more accurately assessed with MR arthrography. 10,30
Arthropathies
MRI is not required for the diagnosis of osteoarthrosis. However, since it is such a common disorder, osteoarthrosis is often imaged in patients with other diagnostic dilemmas. The hallmark characteristics of osteoarthrosis (osteophytes, joint space narrowing, chondromalacia, loose bodies, etc.) are clearly depicted by multiplanar MR imaging (Figure 17). 4 Cartilage may be optimally imaged using gradient-echo imaging (such as double-echo steady state) or with MR arthrography. 10
Multiple other arthropathies can affect the elbow, some of which have characteristic features. Gout may also involve the elbow (Figure 18). The olecranon bursa is more commonly involved than the joint. Fluid in the bursa may be due to bursitis, but gout should always be considered. 4 When the elbow is affected by rheumatoid arthritis, the wrist and hand are invariably involved. 27 MRI provides a method for early detection of synovial inflammation and bone erosions (Figure 19). Response to therapy (active synovial inflammation and new erosions) can also be monitored with contrast-enhanced MR imaging.
Infection
Musculoskeletal infections may present with an acute, rapidly progressing course or may be insidious. Determining the extent of involvement is important in planning medical or surgical management. For example, the quantity of fluid within an infected olecranon bursa and the extent of the surrounding soft tissue involvement can be delineated with CT (Figure 20). Osseous involvement with infection is first assessed with radiographs (Figures 21 and 22), which may be diagnostic. Radioisotope studies (Figure 21) are particularly sensitive in the early stages of infection. The anatomic extent, however, may be inaccurate, especially in the articular regions, and differentiation of cellulitis or soft tissue infection from bone involvement is not always possible. 3
MR imaging may be required to make a definitive diagnosis of infection. Generally, a combination of T1W, STIR, or FSE T2W fat-sup-pressed, and enhanced T1W fat-suppressed images is the most sensitive technique for the detection of osteomyelitis. Osteomyelitis is characterized by an area of prolonged T1 and T2 relaxation times and marrow en-hancement. Changes in cortical bone (osteitis), periosteum (periostitis), and muscle are often less obvious. The presence of associated cortical destruction, sinus tracts, low-intensity sequestra, cloaca, and adjacent soft tissue inflammatory signal changes can also be evaluated with MR.
Conclusion
In this article, the imaging characteristics of a variety of disease processes involving the elbow have been presented. There are distinct advantages of each of the different imaging modalities: radiography, sonography, scintigraphy, arthrography, CT, and MRI. The choice of imaging technique will depend on the suspected disease process, the availability of advanced imaging (such as MDCT and MRI), and the personal preference of the radiologist. The ultimate goal is to provide the most accurate diagnosis for each patient, which allows for the best patient care.
