Jugular fossa meningocele
Images

Summary
An 18-year-old woman presented with a history of recurrent headaches, which were described as dull aching and persisting for a few hours, mainly on the right side. They were not associated with any obvious cause; there was no history of associated visual disturbances, vertigo, dizziness, earache, nausea, or recurrent upper respiratory tract infections. The general and systemic nervous examination findings were within normal limits. Other sytemic examinations did not reveal any significant abnormality. Ophthalmologic and otorhinolaryngoscopic examinations also did not reveal any abnormalities of note. Routine laboratory investigations were noncontributory.
Findings
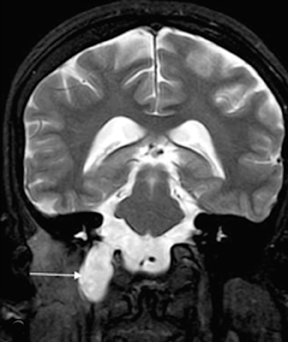
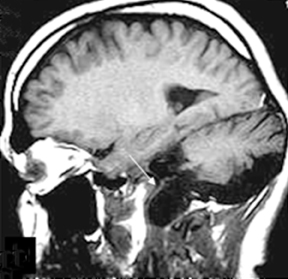
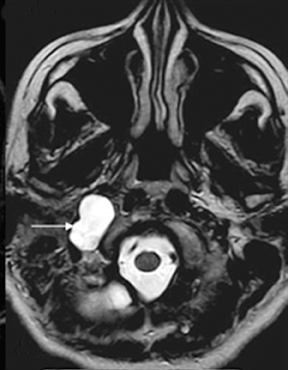
A radiograph of paranasal sinuses and a lateral view of the skull did not reveal any significant abnormality. The patient was referred for a magnetic resonance imaging (MRI) scan of the brain. The scan was performed on a 1.5T MR scanner. A bony defect was observed in the right jugular fossa. Adjacent bones were well scalloped. No obvious destruction of the cortical bone was suspected. There was continuation of the dural meningeal pouch within this defect. It was lining the CSF collection, which appeared hyper-intense on T2-weighted images, and hypo-intense on T1-weighted images. No obvious herniation of the neuroparenchyme or cranial nerve was seen within this out-pouching (Figure 1).
Imaging findings suggested meningocele in the right jugular foramen region. The contents of the right jugular foramen were displaced laterally to this meningocele. It was also extending minimally anteriorly towards the foramen lacerum. Inferiorly, it was bulging into the right parapharyngeal space. The medial margin was seen near the pharyngeal wall. The carotid vessels were also displaced laterally. The right parapharyngeal fat was reduced, compared to that of the left side. The patient was informed about this type of congenital anomaly; she decided not to undergo surgical intervention. She is being treated symptomatically with analgesics.
Diagnosis
Jugular fossa meningocele
Discussion
Cephaloceles are congenital herniations of intracranial contents into the skull’s bony defects. These may be meningocele or meningo-encephaloceles (abbreviated as encephalocele), depending on the absence or presence of brain tissue.1 When the lepto-meninges and CSF are herniated without associated herniation of brain parenchyma, it is termed meningocele. Meningoceles of the jugular foramen region are extremely uncommon and difficult to explain by current skull-base cephalocele classifications.
The jugular foramen is situated between the petrous portion of temporal and occipital bones and originates from persistence of the embryologic foramen lacerumposticus, the space between the basi-occiput and auditory canal.2 The cephaloceles are known to occur through the suture lines or junction of several bones.3 The skull base cephaloceles are classified into fronto-ethmoidal, spheno-orbital, sphenomaxillary, temporal, and nasopharyngeal types.3,4 Rare case reports of cephaloceles through the tegmen of petrous temporal bone, the greater wing of the sphenoid and the centre of the basilar occipital bones have been described.3,5,6 Our case, with its involvement of the jugular fossa, does not fit precisely within this classification. However, another case of large skull-base meningo-encephalocele in a newborn has been described with a neck mass passing through the jugular foramen.7
Basal cephaloceles are rare, with an incidence of about 1 in 35,000 births.7 Basal cephaloceles are commonly occult and without any symptoms. Therefore, they may not be identified until adulthood, especially if there is no herniation of brain contents, as in our case. The prognosis is better, especially when they are < 5 cm in diameter, do not contain dysplastic or brain tissue, and when they are not associated with hydrocephalus or other anomalies.8 Our patient, who had presented in adulthood, thus had a better prognosis. Cephaloceles are commonly associated with malformation syndromes (neurofibromatosis, Dandy Walker syndrome, septo-optic dysplasia, etc.), heterotopias, cleft palate, other midline anomalies, craniostenosis, agenesis of the corpus callosum, brainstem anomalies, etc.1,7 Their complications include CSF leak and fistula formation, local mass effect on adjacent structures near the skull base, and increased risk of CSF infection, among others.3
Conclusion
Jugular fossa meningoceles may not fit exactly into skull base cephalocele classifications. Meningoceles involving the jugular fossa can present in adulthood and can have better prognosis, especially if they are smaller and not associated with hydrocephalus or other brain/skull anomalies. Possible CSF leak and mass effect at the skull base are important complications.
References
- Matuchansky C, Colin R, et al. Cavitation of mesenteric lymph nodes, splenic atrophy, and a flat small intestinal mucosa. Gastoenterology. 1984;87:606-614.
- Howat A, McPhie J, et al. Cavitation of mesenteric lymph nodes: A rare complication of celiac disease, associated with a poor outcome. Histopathology.1995;27:349-354.
- Holmes G. Mesenteric lymph node cavitation in coeliac disease. Gut. 1986;27:728-733.
Citation
Jugular fossa meningocele. Appl Radiol.
February 1, 2013