MR imaging of femoroacetabular impingement









Dr. Filigenzi is a Fellow in Musculoskeletal Imaging and Dr. Bredella is an Assistant Radiologist, Department of Radiology, Massachusetts General Hospital, Boston, MA. Dr. Bredella is also an Assistant Professor of Radiology, Harvard Medical School, Boston, MA.
Osteoarthritis (OA) of the hip is a very common problem. While there are many different etiologies for OA of the hip, often a specific cause cannot be determined. Recently, femoroacetabular impingement (FAI) has been found to cause progressive degenerative changes leading to early OA of the hip in younger patients.1,2 In FAI, morphologic abnormalities of the proximal femur, acetabulum, or both cause abnormal contact between the femur and acetabulum during motion of the hip joint, especially during flexion and internal rotation. This contact causes abnormal stress on the acetabular labrum and articular cartilage. The resulting degeneration, tearing of the labrum, and damage to the adjacent acetabular cartilage can lead to the development of OA.1-6
Recognition of FAI and its relationship to early OA of the hip requires early diagnosis and treatment to prevent or delay hip degeneration. Magnetic resonance imaging (MRI) and MR arthrography are excellent imaging modalities for showing the morphologic abnormalities of the proximal femur and acetabulum as well as the various changes seen in the hip secondary to FAI. In this article, the authors describe the 2 different proposed mechanisms for FAI, imaging of the morphologic abnormalities, and secondary changes seen around the hip as a result of FAI.
Pathomechanisms of femoroacetabular impingement
The normal anatomy of the hip allows for a wide range of motion. The morphologic abnormalities that predispose a patient to the development of FAI result in decreased joint clearance between the femoral neck and acetabulum. This results in the abnormal contact, or impingement, between the femoral neck and acetabulum, leading to the degenerative changes in the acetabular labrum and/or adjacent articular cartilage.2,7-9
Two types of FAI can be distinguished: those secondary to abnormalities of the proximal femur (cam impingement) and those secondary to acetabular causes (pincer impingement). Cam impingement is a result of a morphologically abnormal femoral head impinging against a normal acetabulum during hip motion.1,3-6,8 Pincer impingement is caused by contact between the acetabular rim and the femoral neck as a result of acetabular abnormalities, such as acetabular retroversion leading to anterior overcoverage of the femoral head.1,8,10-12 While the 2 types of FAI will be described as 2 separate, distinct entities, often a combination of factors can lead to the development of FAI.1
Cam impingement
Cam impingement results from an abnormality of the femoral head. These abnormalities include a variety of different processes, including insufficient femoral head-neck offset, subtle displacement of the femoral epiphysis, slipped capital femoral epiphyses (SCFE), or postsurgical or posttraumatic deformities.6,9,13-18
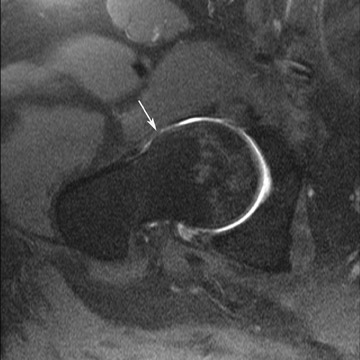
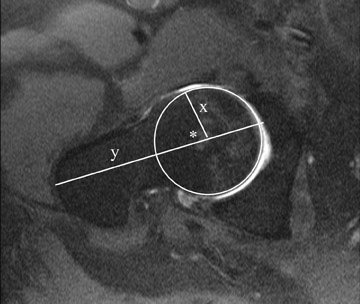
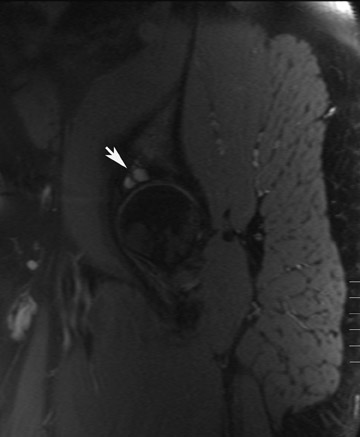
Many of these changes can be readily identified on radiographs and MRI. A decreased offset of the femoral head-neck junction, which is the difference between the widest diameter of the femoral head and the most prominent part of the femoral neck, will appear as a lack of the normal waisting of the femoral head-neck junction. On MRI or radiography, a prominent lateral extension of the femoral head at the expected step-off to the adjacent femoral neck can be seen (Figure 1).5,13 This femoral “bump” is typically located lateral to the physeal scar. The abnormal flattening or convexity of the usually concave lateral head-neck junction has been described as a “pistol grip” deformity.19
A reduced femoral head-neck junction can be best assessed on MRI using dedicated oblique axial images that are obtained parallel to the long axis of the femoral neck. Methods of quantitatively evaluating the femoral head-neck offset have been described with the “alpha” angle.20 The alpha angle is calculated on the above-mentioned oblique axial MR images of the hip. The angle is measured between a line drawn from the center of the femoral head through the central axis of the femoral neck and a second line drawn from the center of the femoral head to the point anteriorly where the distance from the center of the head exceeds the radius of the subchondral femoral head (Figure 1). It has been proposed that an alpha angle >55° predisposes a patient to cam FAI.20
Pincer impingement
In pincer FAI, the acetabulum, rather than the proximal femur, has a morphologic abnormality that results in abnormal contact between the femur and acetabulum. As with cam FAI, several abnormalities can lead to pincer FAI, the common problem being an increased relative depth of the acetabulum that results in overcoverage of the femoral head. Abnormalities that can be associated with pincer FAI include acetabular retroversion, coxa profunda, and protrusio acetabuli. All of these abnormalities can be identified on radiographs and MRI.
Radiographic findings of acetabular retroversion include the crossover or “figure-8” sign and the posterior wall sign.21,22 The crossover sign is caused by the anterior wall of the superior aspect of the acetabulum projecting lateral to the posterior wall of the superior aspect of the acetabulum (Figure 2).21,22 The line that demarcates the posterior wall passes medial to the center point of the femoral head, rather than following the normal passage at or lateral to the center of the femoral head.21,22
Protrusio acetabuli and acetabular retroversion (a posteriorly oriented acetabulum) can be seen on oblique axial MRI of the hip. The acetabular retroversion will result in an increase in coverage of the anterior aspect of the femoral head.22 Acetabular depth can be quantified on the same oblique axial images that are used to calculate the alpha angle. The depth is calculated by drawing a line connecting the anterior and posterior acetabular rims and a parallel line that passes through the center of the femoral head. The distance between these 2 lines is the acetabular depth, with the value being positive if the center of the femoral head is lateral to the acetabular rim.23 As would be expected, the acetabulum is significantly deeper in patients with pincer FAI than in patients in cam FAI, in which the depth is normal.23 Future research may recognize a specific value for the acetabular depth that puts a patient at increased risk for the development of pincer FAI.
Imaging findings of femoroacetabular impingement
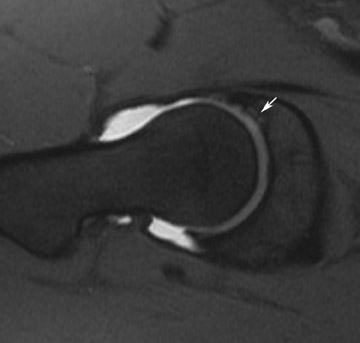
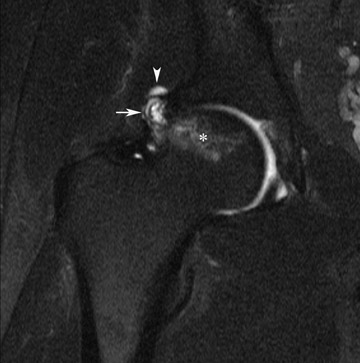
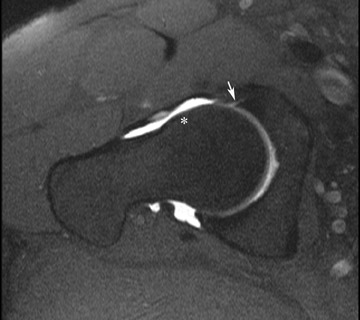
MRI findings of changes secondary to FAI within the acetabulum can be seen involving the acetabular bone, labrum, and articular cartilage. Recent research by James et al24 suggests that a majority of the abnormalities are located peripherally at the labral-chondral transition zone. The articular cartilage can show a variety of changes. Early damage is manifested by areas of signal hyperintensity that represent areas of chondral softening. Eventually, this softening progresses from articular cartilage fissures to chondral fragmentation and resultant full-thickness chondral defects (Figures 3 and 4). These changes are classically described as appearing in the antero-superior aspect of the acetabulum. However, recent research suggests that patients with cam FAI tend to have articular cartilage lesions in the antero-superior portion of the acetabulum, while patients with pincer FAI tend to have cartilage lesions in the posteroinferior aspect of the acetabulum.23
Once chondral abnormalities are present, subsequent changes can also be seen in the adjacent subchondral bone. This includes the development of subchondral edema, sclerosis, and cysts (Figures 3 through 5). Fragmentation of the anterior acetabular margin is frequently seen (Figure 4). In fact, an os acetabuli is often identified in patients with FAI.25
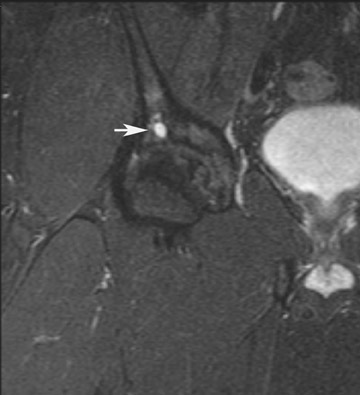
Changes in the acetabular labrum include degenerative signal manifested as increased signal in the normally dark labrum on fluid-sensitive sequences as well as labral tears and complete labral detachments. Associated paralabral cysts can also be seen (Figures 6 and 7).7,26,27
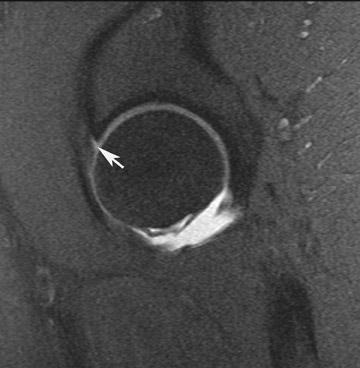
Changes secondary to FAI are not just limited to the acetabulum but can also be seen in the proximal femur. Such abnormalities include the development of subchondral edema and juxta-articular fibrocystic changes within the proximal femur, usually at the site of the dysplastic femoral bump (Figure 8). The femoral-sided fibrocystic changes, including the “Pitt’s Pit,” likely represent the point of impingement on the femur and do not represent a normal variation of synovial herniation, given their relatively high prevalence in patients with FAI and their location at the anatomic site of impingement.6,26,28
Additional findings as a result of FAI can also be seen in the soft tissues around the femur and acetabulum, usually as a result of secondary inflammation related to the FAI. There may be thickening of the joint capsule, often with an associated synovitis, and thickening of the iliofemoral ligament laterally.
Conclusion
Femoroacetabular impingement is a relatively common disorder that can result in the development of OA in the younger patient population. This article addressed the various morphologic abnormalities that predispose a patient to the development of FAI and detailed the changes that can be seen around the hip as a result of FAI. MRI and MR arthrography are accurate, noninvasive methods for the evaluation of both the structural abnormalities and the pathologic changes associated with FAI. Correct diagnosis of this disease process is essential to prevent or delay the progression of OA.
REFERENCES
- Ganz R, Parvizi J, Beck M, et al. Femoroacetabular impingement: A cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112-120.
- Tanzer M, Noiseux N. Osseous abnormalities and early osteoarthritis: The role of hip impingement. Clin Orthop Relat Res. 2004;429:170-177.
- Beck M, Leunig M, Parvizi J, et al. Anterior femoroacetabular impingement: Part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004; 418:67-73.
- Ito K, Leunig M, Ganz R. Histopathologic features of the acetabular labrum in femoroacetabular impingement. Clin Orthop Relat Res. 2004;429:262-271.
- Ito K, Minka MA 2nd, Leunig M, et al. Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br. 2001;83:171-176.
- Jäger M, Wild A, Westhoff B, Krauspe R. Femoroacetabular impingement caused by a femoral osseous head-neck bump deformity: Clinical, radiological, and experimental results. J Orthop Sci. 2004;9:256-263.
- Leunig M, Podeszwa D, Beck M, et al. Magnetic resonance arthrography of labral disorders in hips with dysplasia and impingement. Clin Orthop Relat Res. 2004;418:74-80.
- Lavigne M, Parvizi J, Beck M, et al. Anterior femoroacetabular impingement: Part I. Techniques of joint preserving surgery. Clin Orthop Relat Res. 2004;418:61-66.
- Beck M, Leunig M, Clarke E, Ganz R. Femoroacetabular impingement as a factor in the development of nonunion of the femoral neck: A report of three cases. J Orthop Trauma. 2004;18:425-430.
- Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br. 1999;81:281-288.
- Ferguson SJ, Bryant JT, Ganz R, Ito K. The acetabular labrum seal: A poroelastic finite element model. Clin Biomech (Bristol, Avon). 2000;15:463-468.
- Ferguson SJ, Bryant JT, Ganz R, Ito K. An in vitro investigation of the acetabular labral seal in hip joint mechanics. J Biomech. 2003;36:171-178.
- Leunig M, Beck M, Woo A, et al. Acetabular rim degeneration: A constant finding in the aged hip. Clin OrthopRelat Res. 2003;413:201-207.
- Eijer H, Myers SR, Ganz R. Anterior femoro-acetabular impingement after femoral neck fractures. J Orthop Trauma. 2001;15:475-481.
- Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991;73:423-429.
- Leunig M, Casillas MM, Hamlet M, et al. Slipped capital femoral epiphysis: Early mechanical damage to the acetabular cartilage by a prominent femoral metaphysis. Acta Orthop Scand. 2000;71: 370-375.
- Myers SR, Eijer H, Ganz R. Anterior femoro-acetabular impingement after periacetabular osteotomy. Clin OrthopRelat Res. 1999;363:93-99.
- Pitto RP, Klaue K, Ganz R, Ceppatelli S. Acetabular rim pathology secondary to congenital hip dysplasia in the adult. A radiographic study. Chir Organi Mov. 1995;80:361-368.
- Stulberg SD, Cordell, LD, Harris WH, et al. Unrecognized childhood hip disease: A major cause of idiopathic osteoarthritis of the hip. Proceedings of the Third Open Scientific Meeting of the Hip society. The Hip. St Louis, MO: CV Mosby; 1975, 2112–2228.
- Nötzli HP, Wyss TF, Stoecklin CH, et al. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556-560.
- Siebenrock KA, Schoeniger R, Ganz R. Anterior femoroacetabular impingement due to acetabular retroversion. Treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85-A(2): 278-286.
- Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br. 1999;81:281-288. Comment in: J Bone Joint Surg Br. 1999;81:743-744.
- Pfirrmann CW, Mengiardi B, Dora C, et al. Cam and pincer femoroacetabular impingement: Characteristic MR arthrographic findings in 50 patients. Radiology. 2006;240:778-785.
- Erratum in: Radiology. 2007;244:626. Comment in Radiology. 2007;244:625-626; author reply 626.
- James SL, Ali K, Malara F, et al. MRI findings of femoroacetabular impingement. AJR Am J Roentgenol. 2006;187:1412-1419.
- Kassarjian A, Yoon LS, Belzile E, et al. Triad of MR arthrographic findings in patients with cam-type femoroacetabular impingement. Radiology. 2005; 236:588-592.
- Stoller DW, Tirman PFJ, Bredella MA. Femoroacetabular impingement. In: Diagnostic Imaging: Orthopaedics. Salt Lake City, UT: Amirsys; 2004.
- Sadro C. Current concepts in magnetic resonance imaging of the adult hip and pelvis. Semin Roentgenol. 2000;35:231-248.
- Leunig M, Beck M, Kalhor M, et al. Fibrocystic changes at anterosuperior femoral neck: Prevalence in hips with femoroacetabular impingement. Radiology. 2005;236:237-246.
