MRI of the hand and fingers
Images





















Modern magnetic resonance imaging (MRI) techniques and high-quality surface coils can provide exquisite anatomic detail of the small extremities such as the hands and feet. The fine soft tissue contrast resolution provided by MRI allows accurate identification and characterization of a variety of traumatic injuries, arthropathies, and neoplastic processes. Recent advances in gradient hardware, coil design and pulse sequences, as well as the proliferation of 3 tesla (T) MR units, allow very small field-of-view imaging at high resolution.1 3T magnets provide increased signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR) compared to 1.5T magnets. Dedicated multichannel hand and wrist coils further optimize signal to noise ratios. In addition, these coils facilitate optimal patient positioning. When coupled with appropriate imaging protocols, 3T imaging of the hand can offer improved diagnostic outcomes through superior visualization of the articular cartilage and small supporting soft tissue structures of the hand.
Limiting the field of view to the area of interest is vital to optimizing anatomic detail when imaging the small structures of the hand. Multisequence, T1-weighted and fluid-sensitive imaging is generally performed in the axial plane and in at least one orthogonal longitudinal plane, prescribed as either coronal or sagittal based on the anatomy of interest. Multiplanar, high-resolution, isotropic sequences are also helpful for evaluating the thin articular hyaline cartilage as well as the ligaments and other small intrinsic structures of the hand and fingers.
Normal hand and finger anatomy
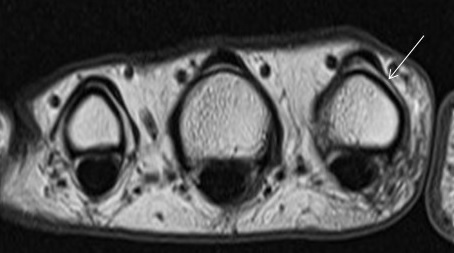
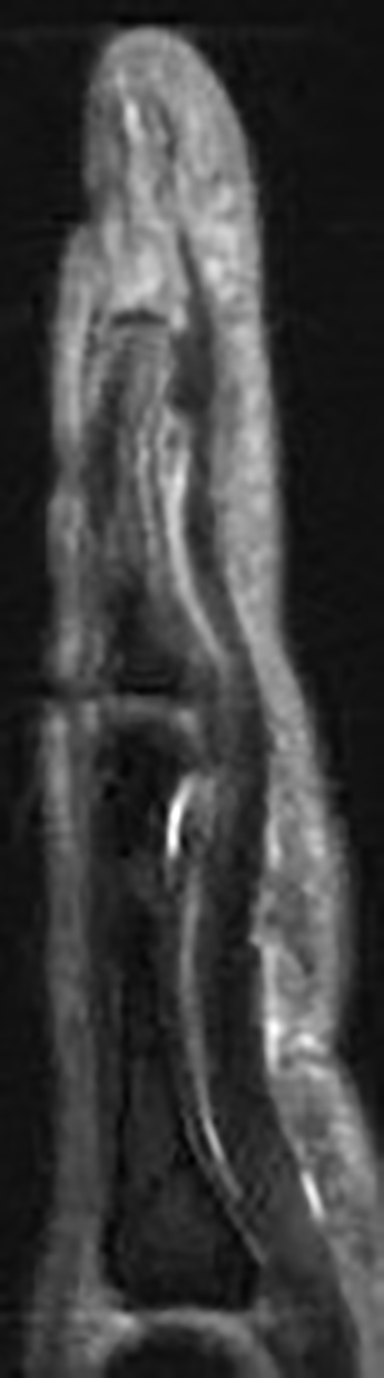
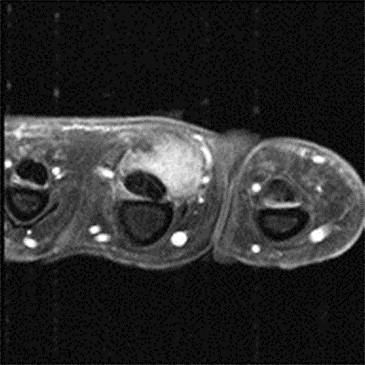
In the palmar aspect of the hand, the flexor digitorum superficialis (FDS) tendons of the lesser (second-fifth) digits insert onto the palmar aspects of the bases of the middle phalanges. Prior to their insertion, they briefly split at the level of the proximal phalanges then reunite at the level of the proximal interphalangeal (PIP) joints to create ring apertures for passage of the flexor digitorum profundus (FDP) tendons. After passing through the FDS apertures, the FDP tendons continue more distally to insert on the palmar aspects of the bases of the distal phalanges (Figure 1).2 The flexor tendon sheaths begin at the level of the metacarpal necks and are each associated with complex pulley systems comprised of 5 annular and 3 cruciate pulleys.3
In the dorsal aspect of the hand, the digital branches of the extensor digitorum (ED) tendon trifurcate distal to the metacarpophalangeal (MCP) joint. A central band from each ED branch inserts on the dorsal aspects of the bases of the lesser middle phalanges. Radial and ulnar bands continue more distally to insert on the dorsal aspects of the bases of the distal phalanges.4 In combination with the radial and ulnar bands, the extensor hoods of the lesser digits provide dorsal stability by preventing subluxation or dislocation of the ED branches.5 (Figure 2).
The MCP joint collateral ligaments of the thumb and lesser digits extend with slight obliquity from shallow depressions on the radial and ulnar aspects of the metacarpal heads to the bases of the proximal phalanges. These ligaments are considered thickened portions of the joint capsule and provide stability to varus and valgus forces and are contiguous with the volar plates at the palmar aspects of the joints.6
Traumatic injuries of the hand and fingers
The fine soft-tissue contrast resolution of MRI allows assessment of the tendons, ligaments, and intricate pulley systems of the fingers. Normal tendons and ligaments of the hands typically demonstrate low signal intensity on MR imaging. In contrast, these structures exhibit increased signal intensity or abnormal morphology when injured.
Flexor tendon injuries
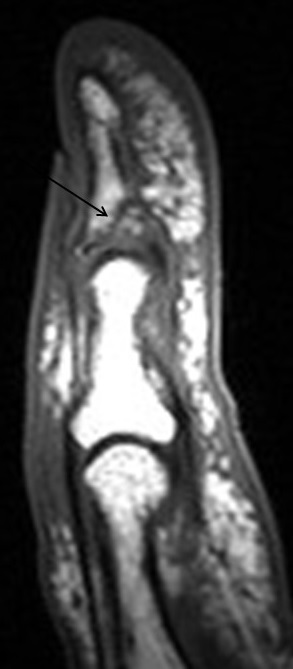
Flexor tendon injuries most commonly occur secondary to a palmar laceration or a sports-related injury. Tendon rupture or avulsion usually results from resisted forced extension or entanglement during the action of tackling (“jersey finger”). MRI can accurately differentiate a partial-thickness tear from a complete tear and can readily depict the length of tendon retraction. This injury may occur anywhere along the course of a flexor tendon and are classified by site (zone) of injury. A zone 1 injury is designated as any injury distal to the FDS insertion. The most common example is the nonosseous “jersey finger” with forced hyperextension against an actively contracting FDP with avulsion of the tendon from the palmar aspect of the distal phalanx (Figure 3). A zone 2 injury is designated as an injury incurred within the fibro-osseous tunnel from the A1 pulley to the FDS insertion. This injury can affect both the FDS and FDP tendons and can be the most difficult to surgically manage secondary to the intrasynovial location and the complexity of the anatomy, particularly the intricate pulley system (Figures 4,5).3 A zone 3 injury is designated as an injury incurred between the carpal tunnel and the A1 pulley. Zone 4 and 5 injuries represent flexor tendon injuries within or proximal to the carpal tunnel, respectively. Management generally consists of primary operative repair within 1-2 weeks of injury.7
Extensor tendon injuries
Extensor tendon injuries may occur anywhere along the course of the extensor tendons (Figure 6). A common example is a distal avulsion of the ED from the distal phalanx (“mallet finger”), with or without an avulsion fracture. This occurs with forced flexion at the DIP joint during active contraction of the ED. Management of a closed nonosseous mallet finger is generally nonoperative, but failure to treat may result in chronic swan-neck deformity with PIP joint hyperextension and flexion at the DIP joint. Avulsion of the central slip insertion on the middle phalanx will result in a boutonniere deformity with flexion at the PIP joint and a hyperextended DIP joint.4
Volar plate and flexor pulley lesions
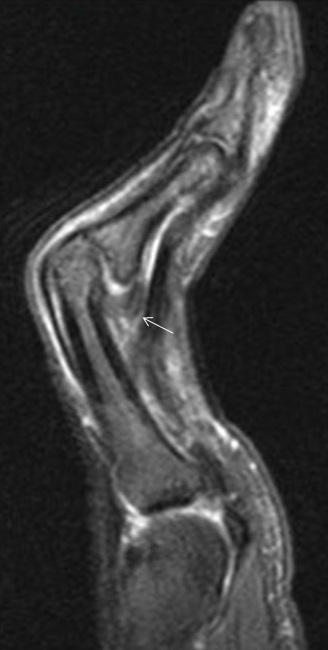
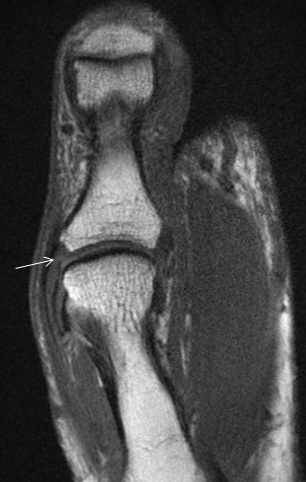
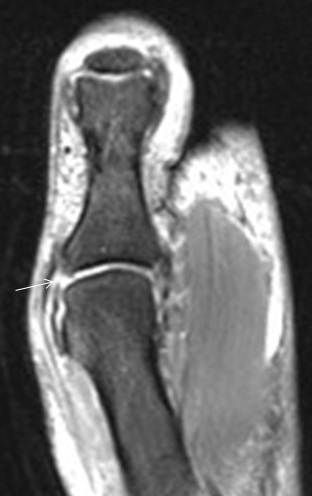
The volar plate stabilizes the PIP joint, which helps prevent hyperextension. On MRI, the volar plate is a low signal intensity structure best seen in the sagittal plane with a firm distal attachment on the middle phalanx and a pair of more elastic attachments on the proximal phalanx (Figure 7).5,8 Injury to the volar plate may result in pain and sagittal plane instability (Figure 8). Splinting and early physiotherapy will often restore function.9
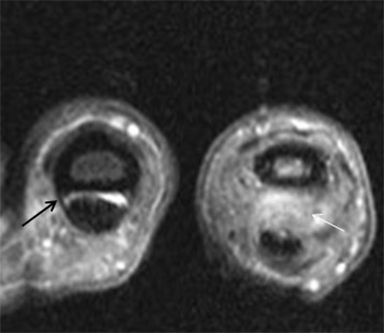
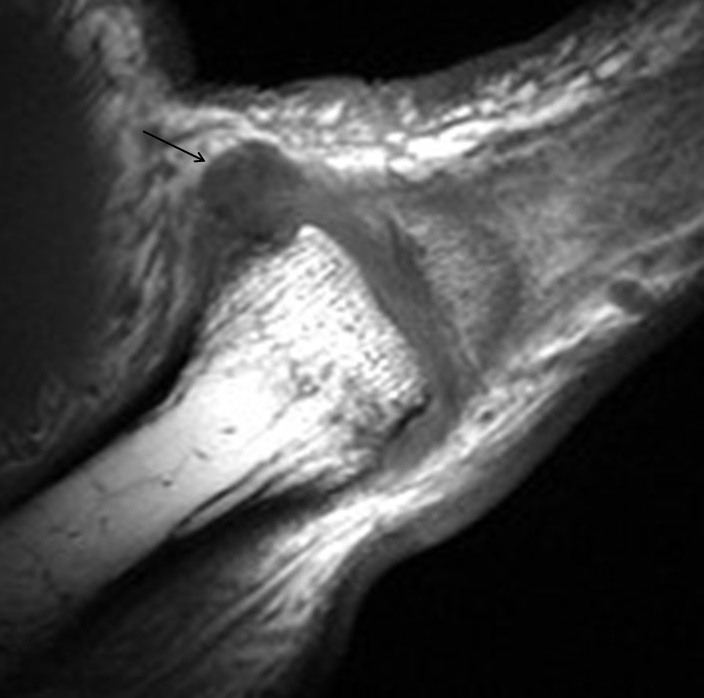
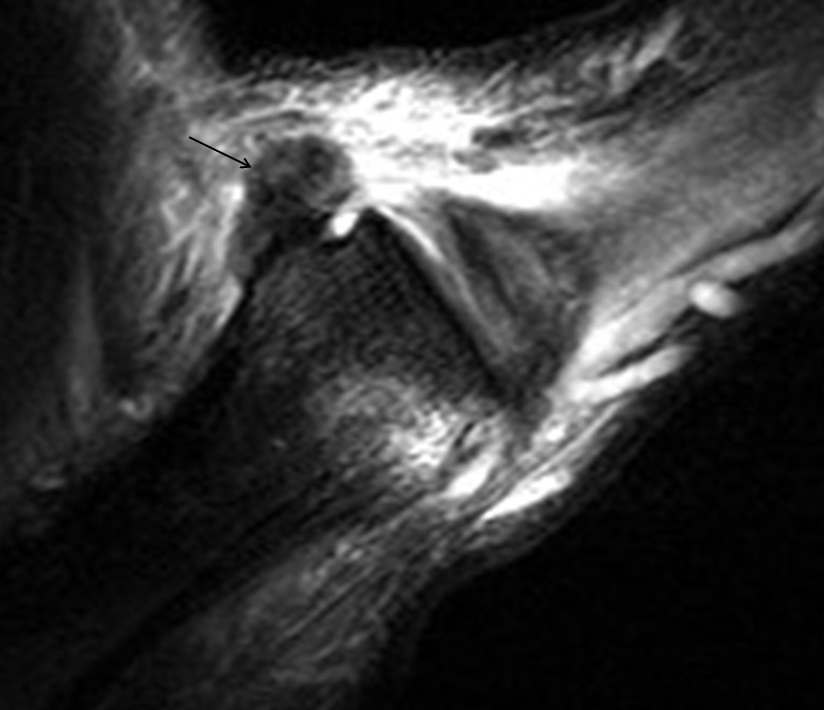
The major function of the flexor pulley system is to secure the flexor tendon along the fibro-osseous tunnel and stabilize the tendon during flexion. Injury may occur anywhere along the pulley system, resulting in abnormal “bowstringing” with development of an abnormal gap between the flexor tendon and the underlying bone with flexion of the digit (Figure 9).5 The most frequently injured component is the A2 pulley, followed sequentially by injury to the A3 and A4 pulleys. Injury to the A1 pulley is rare.
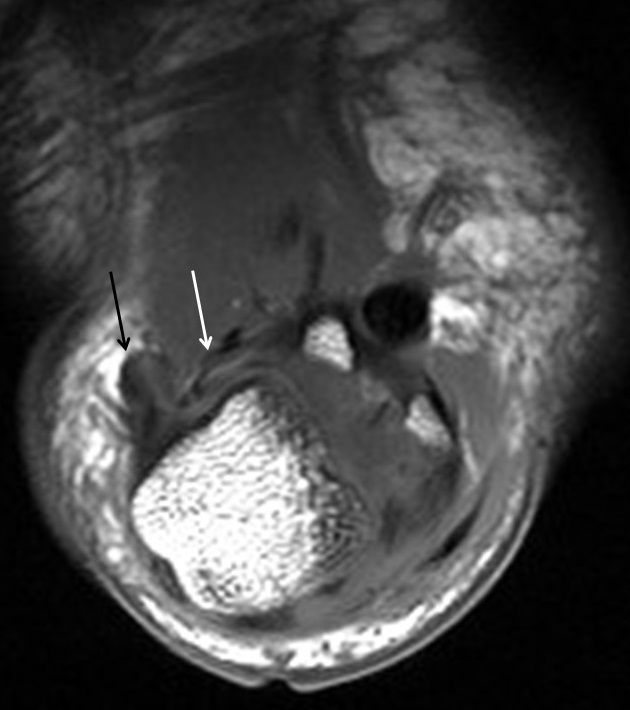
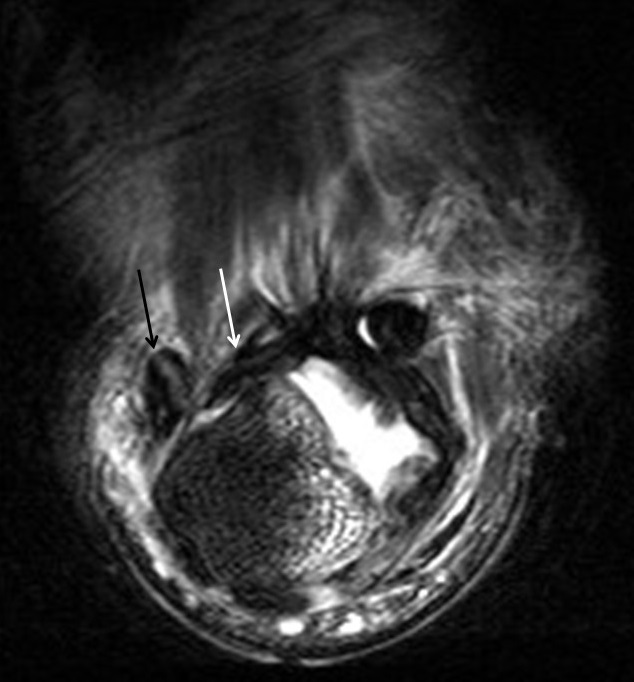
Collateral ligament injuries
MCP collateral ligament injuries range from mild sprain (grade 1) to complete tears (grade 3). Complete tears lead to instability (Figures 10-11). The most common collateral ligament injury in the hand involves the ulnar collateral ligament of the thumb, usually due to a violent hyperabduction mechanism and commonly referred to as “gamekeepers” or “skiers” thumb (Figure 12). Low grade partial or nondisplaced UCL injuries are successfully treated with conservative measures in most cases. However, if the thumb UCL ligament is torn and retracted it may become displaced superficial to the adductor aponeurosis (known as a Stener lesion), which will inhibit healing (Figure 13). Stener lesions require surgical fixation to prevent chronic instability and reduced pinch/grip strength.5, 9 Collateral ligament injuries of the lesser digit MCP joints are much less common. As with thumb UCL injuries, good outcomes are usually achieved with conservative treatment, although isolated high grade ligament tears may require surgical repair.10
Occult fracture
MRI has become a valuable tool in the assessment of radiographically occult fractures. It has demonstrated similar specificity and superior sensitivity compared to CT, making it the gold standard for fracture detection.11 However, its high cost limits routine use in the hands and fingers, particularly since the results rarely alter the original treatment plan of splinting, rest and pain control.
Arthropathies of the hand and fingers
Cartilage damage in the hand and fingers is a feature common to several disease processes commonly associated with those of a degenerative, inflammatory, or infectious nature. The resultant cartilage damage is irreversible, and disability can be significant. Currently, there is wide research interest on earlier identification of active disease in order to prevent cartilage damage and disability.
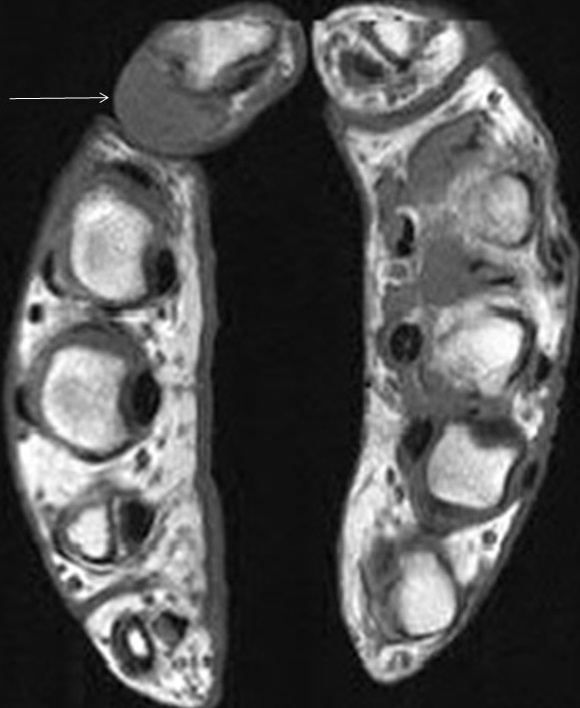
MR imaging of the hand has a few advantages over radiography in the evaluation of hand and finger arthropathies. For example, joint spaces may appear preserved on radiographs in the setting of synovitis or joint effusion, falsely implying normal cartilage, whereas MRI allows direct visualization of the articular cartilage. MRI is also able to detect small T2 hyperintense subchondral cysts and erosions before they are radiographically apparent. Erosions usually manifest on MRI as sharply marginated marrow signal abnormalities, often with enhancement after gadolinium administration and indicative of the presence of synovitis or active hypervascular pannus. Focal low T1 and high T2 marrow edema-like signal may be a precursor of an erosion. MRI findings of synovitis include abnormal T2 hyper intensity and thickening of the synovium (normally paper-thin), with or without effusion. Intravenous contrast is necessary to differentiate synovitis from synovial fluid.12 Simultaneous high-resolution imaging of both hands may be performed utilizing a “praying hands” protocol, which is helpful in the evaluation of early active systemic inflammatory arthropathies, with excellent demonstration of the symmetry or asymmetry of involvement.
Osteoarthritis
Osteoarthritis (OA) is the most common joint disease in the hand and disease prevalence increases with age. More than 50% of men and women over the age of 60 with hand radiographs have findings of OA.13 OA is generally a slowly progressive disorder characterized by nonuniform articular cartilage narrowing, periarticular sclerosis, osteophytosis and subchondral cysts. There is a predilection for the distal interphalangeal (DIP) joints and the thumb carpometacarpal joint. OA is increasingly thought to represent a continuum with what has been termed erosive or inflammatory OA. Erosive OA variably has additional features of synovitis, tenosynovitis and erosions (Figure 14) and is seen most frequently in post-menopausal females. When synovitis is seen in the presence of OA, the current theory is that the synovitis is a marker of a secondary inflammatory response to cartilage injury and free particles within the joint. Detection of synovitis in a patient with OA may predict those at risk for erosive OA, allowing early preventative treatment.14
Rheumatoid arthritis
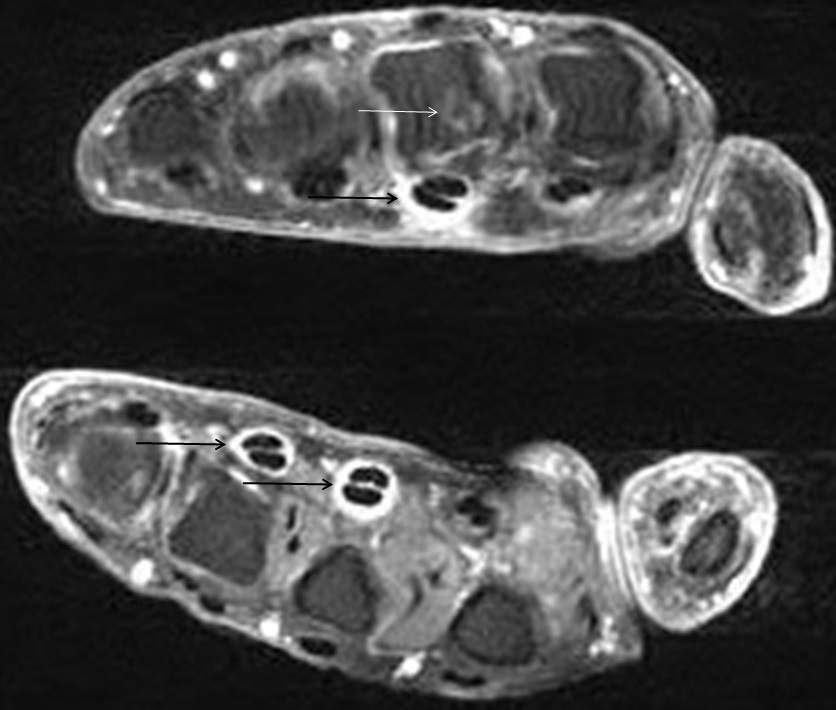
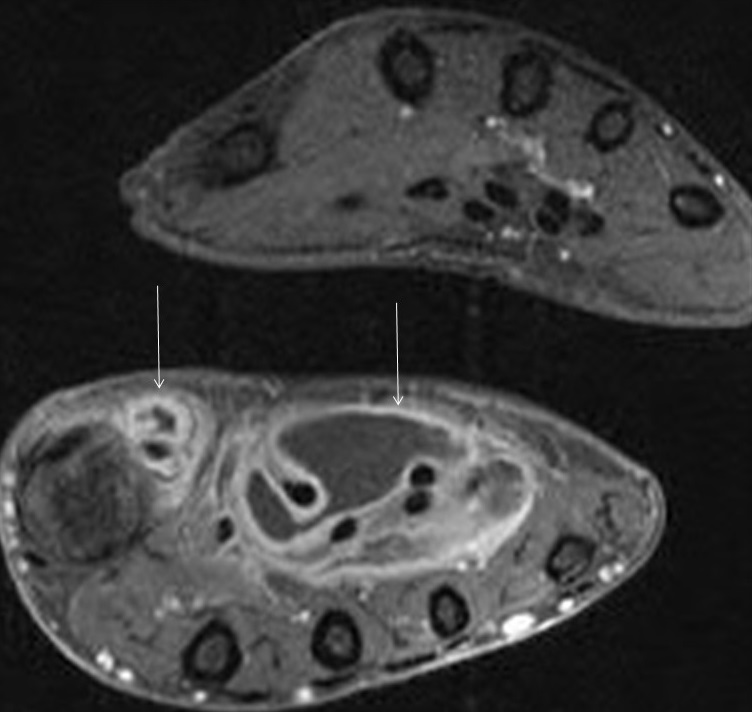
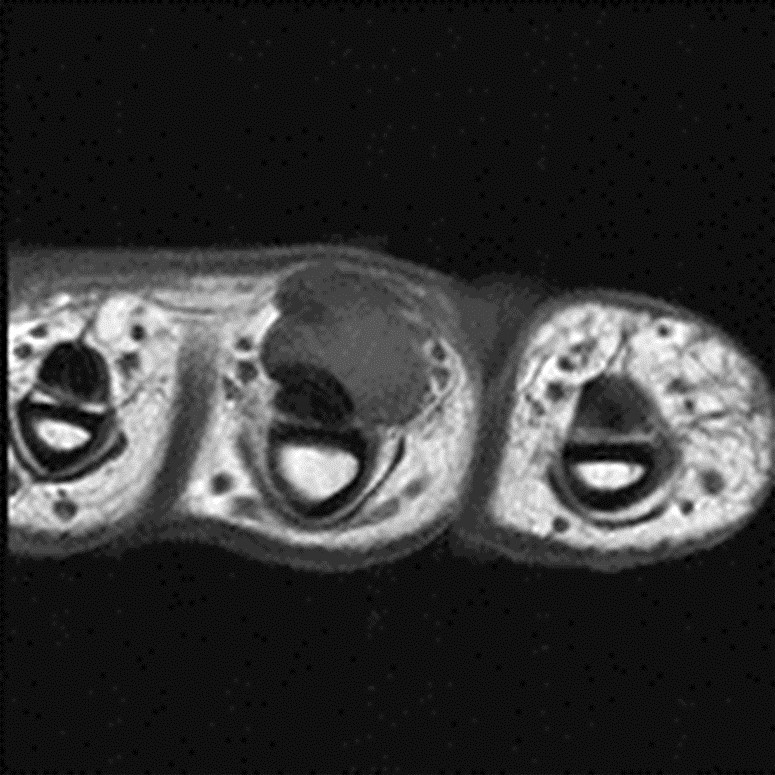
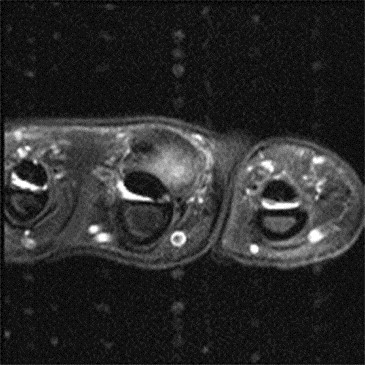
Rheumatoid arthritis (RA) is an uncommon chronic systemic inflammatory arthropathy affecting approximately 0.5-1.0% of the population, although the prevalence appears to be increasing.15 RA manifests as a proliferative, hypertrophic synovitis that leads to bone erosion and cartilage destruction. Within the upper extremity, RA preferentially involves the wrist and MCP joints. The characteristic radiographic findings of symmetric or concentric joint space narrowing and marginal erosions indicate the presence of irreversible cartilage and bone damage. Greater availability and positive outcomes associated with disease-modifying agents warrant the use of MRI to recognize RA at its earliest stage before irreversible damage occurs. MR allows more prompt and precise detection of synovitis, tenosynovitis, bursitis, early or small erosions, and osteitis (Figures 15, 16). Proliferative synovitis is the earliest recognized pathologic finding in RA, and is a predictor of future indelible damage.16 Tenosynovitis is also a common feature of RA, particularly involving the flexor digitorum, extensor digitorum, and extensor carpi ulnaris tendons (Figure 17). Erosions typically occur at the second and third metacarpal heads, carpus and ulnar styloid.
Osteitis, typically manifesting on MRI as focal marrow edema-like signal at the insertion of the synovial membrane, is increasingly recognized as an early feature of RA that predicts cartilage and bone damage.17 Subcutaneous rheumatoid nodules are present in up to 30-40% of patients, and may be encountered when imaging the hand.18 They may appear predominantly cystic with peripheral enhancement (Figure 18) or solid with uniform enhancement.19
Psoriatic arthritis and other inflammatory arthropathies
Psoriatic arthritis is an uncommon inflammatory arthropathy associated with psoriasis. Up to 30% of patients with psoriasis can be affected. Psoriatic arthritis tends to follow either a row or ray pattern. A row pattern has a predominantly distal distribution, involving the IP joints more than the MCP joints, which creates a diagnostic challenge with OA. A ray pattern usually manifests as isolated tenosynovitis, especially of the flexor tendon sheaths, with associated soft tissue edema (dactylitis or “sausage digit”), which can be readily identified on MRI. Multiple digits can be involved simultaneously (polydactylitis). Marrow edema-like signal is the earliest osseous finding on MRI, and tends to originate at the insertion of the joint capsule on the phalanx. This signal becomes more extensive with disease progression. Erosions eventually form at the bone margins leading to the “pencil-in-cup” deformity that is characteristic of psoriatic arthritis.20 Other systemic inflammatory disorders such as systemic lupus erythematosus can have findings of tenosynovitis, synovitis, and focal marrow edema-like signal as well, which may be indistinguishable from early or seronegative RA.21
Septic arthritis and oosteomyelitis
Septic arthritis is an arthropathy caused by an intra-articular infection that leads to joint destruction. Risk factors include bacteremia, immunocompromised state, rheumatoid arthritis, and prior penetrating injury. Septic arthritis should be considered in the setting of acute monoarticular arthritis, particularly with the accompanying clinical signs and symptoms of joint pain and fever. Early diagnosis and treatment is essential in the setting of septic arthritis with still intact articular cartilage to prevent the immediate risk of irreversible damage and subsequent secondary osteoarthritis. On MRI, the presence of monoarticular arthritis and synovitis with associated subchondral marrow edema-like signal is typical for septic arthritis in the appropriate clinical setting. Osteomyelitis usually occurs in the presence of a skin defect or prior penetrating injury and is characterized by confluent marrow edema-like signal and cortical destruction (Figure 19). T1-weighted images are the most reliable for confident detection of osteomyelitis, as fluid-sensitive sequences can demonstrate similar signal alterations in both non-infectious reactive changes and in osteomyelitis.
Tumor imaging
A wide variety of neoplasms can be found in the hand and fingers, although they are less common than elsewhere within the body. Lesions involving the bones of the hand and fingers account for 6% of all benign and 0.5% of all malignant osseous lesions.1,22 Lesions involving the soft tissues of the hand and fingers account for 15% of all benign and 4% of all malignant soft tissue neoplasms.1,23,24 >MRI can be a useful adjunct for radiographs in the hand and fingers given its ability to accurately delineate and differentiate tissue characteristics. MRI also provides multiplanar capability allowing precise localization of lesions in all planes. Soft tissue lesions are ideally suited for MRI evaluation as this modality is able to precisely localize lesions and delineate their association with surrounding structures. Tissue characterization with MRI is often sufficient to allow specific diagnoses of lesions of the hand and fingers.1
Imaging should include T1-weighted and fluid sensitive imaging in at least two planes, tailored to anatomic location to optimize visualization of the tumor and surrounding tissues. Contrast enhancement with gadolinium is often useful for further delineation and characterization. Magnetic resonance angiography (MRA) may occasionally be of benefit to depict vascular involvement.
Osseous lesions
Benign osseous lesions in the hand and fingers far outnumber malignant lesions, with enchondroma being the most common. Enchondromas are composed of hyaline cartilage arranged in lobules within the central medullary canal.25,26 The diagnosis can be made confidently on radiographs, although occasionally advanced imaging may be useful to evaluate for breach of the cortex and soft tissue extension or to evaluate for pathologic fracture of the lesion.25,27 MRI is superior to both radiography and CT when lesions have soft tissue extension, allowing accurate delineation of soft tissue involvement, including involvement of adjacent compartments and neurovascular structures.25,28 On MRI, enchondromas typically show homogenous lobulated high signal intensity on T2-weighed images and peripheral and septal enhancement following gadolinium administration.25,28
Another benign osseous lesion which can present in the hand and fingers is giant cell tumor of bone. Giant cell tumor arises in the metaphysis, subsequently extends into the epiphysis, and will eventually involve the subchondral surface of the adjacent articular surface of the bone.29,30 Like enchondromas, giant cell tumors have characteristic features on radiographs, which typically allows for confident diagnosis. These tumors present as geographic lytic lesions with well-defined sclerotic margins, often associated with expansile remodeling of the involved bone.25,29,30 MRI shows nonspecific low signal on T1-weighted images and variable but often low signal on T2-weighted images (Figure 20). These tumors often hemorrhage and therefore contain hemosiderin deposition, contributing to the low signal on fluid sensitive sequences. Giant cell tumors of bone may be complicated by secondary aneurysmal bone cyst formation and MRI can be very useful to depict this finding.25
Malignant lesions involving the osseous structures of the hand and fingers are unusual. Statistically, chondrosarcoma is the most common malignant lesion.25 Lymphoma and metastatic disease, especially from a lung primary, can occasionally be seen in the distal upper extremities (Figure 21). Radiographs are again the initial imaging modality of choice, although MRI can be useful to further define the margins of the lesion and to gauge the extent of soft tissue involvement.25,28
Soft-tissue tumors
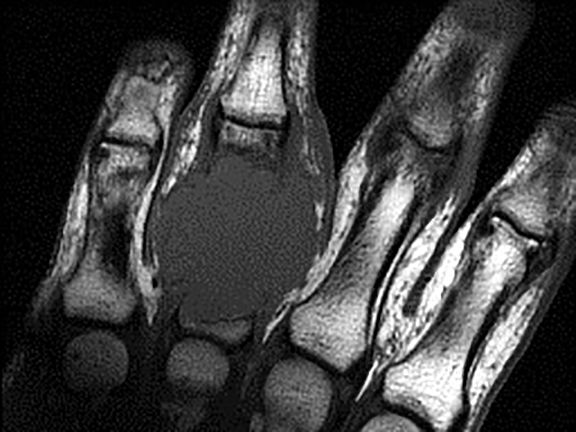
Benign soft tissue lesions in the hand and fingers are significantly more common than malignant soft tissue neoplasms, although malignant soft tissue lesions are significantly more common than malignant osseous lesions.1,22, 23, 24 Ganglia are the most frequently encountered soft tissue lesion in the hand and fingers accounting for between 33 and 60% of all hand lesions.21,25,32 Approximately 70% are found on the dorsum of the hand and fingers.25,33 Ganglia typically image similar to a cyst with high signal throughout the lesion on fluid sensitive sequences.34 They are typically rounded or multilobular in shape and are often associated with tendon sheaths or joint capsules.25,35 Peripheral or septal enhancement may be seen following contrast administration.25
Tenosynovial giant cell tumor or giant cell tumor of tendon sheath is also commonly seen about the hand and fingers, second only to ganglia.25,36 As the name implies, lesions will be intimately associated with a tendon sheath and most commonly involve the flexor tendons.25,36 Lesions are typically nodular in shape with low signal intensity on fluid sensitive sequences related to hemosiderin within the lesions.36 Giant cell tumor of the tendon sheath shows variable enhancement following intravenous gadolinium administration.
Hemangioma and other vascular anomalies can also be seen. Hemangiomas histologically appear similar to normal blood vessels and often contain significant nonvascular tissue including adipose tissue.25,38 MRI often allows confident diagnosis of soft tissue hemangiomas. T1-weighted images often show ill-defined lesions which are predominantly isointense in signal to skeletal muscle but often contain internal areas of fat signal, forming fibrofatty septa within the lesion.25,39 T2-weighted images depict hyperintense signal, which is often serpentine as would be expected of the vascular structures composing the lesion.25,39 Fluid-fluid levels and phleboliths can be seen in slower flow lesions.
Malignant soft tissue lesions are less common than benign lesions and have a more nonspecific MR imaging appearance.25 Lesions typically depict low signal on T1-weighted sequences and high signal on fluid sensitive sequences. Enhancement following contrast administration is also typically seen.1 Soft tissue sarcomas can be seen, similar to elsewhere within the body. Epithelioid sarcoma has a predilection for involvement of the upper extremity. Lymphoma can also uncommonly involve the distal upper extremity.1
Conclusion
Current MRI techniques of the hands and fingers provide a valuable tool for assessment and characterization of traumatic injuries to small structures, various arthropathies, and neoplastic processes. As imaging quality continues to improve, the practicality and value of MRI of the hand and fingers becomes more apparent in the evaluation and management of these entities.
REFERENCES
- Peterson JJ, Bancroft LW, Kransdorf MJ. Principles of bone and soft tissue imaging. Hand Clin. 2004 ;20(2):147-166.
- Thompson, JC. Netter’s Concise Orthopaedic Anatomy, 2nd ed. Philadelphia, PA: Saunders/Elsevier, 2010.
- Lutskey KF, Giang EL, Matzon JL. Flexor tendon injury, repair and rehabilitation. Orthop Clin North Am. 2015;46(1):67-76.
- Resnick D, Kang HS. Internal Derangements of Joints. 2nd ed. Philadelphia, PA: Saunders/Elsevier; 2007.
- Clavero, JA, Alomar X, Monill JM, et al. MR Imaging of ligament and tendon injuries of the fingers. Radiographics. 2002;22(2):237-256.
- De Maeseneer M, Van Roy P, Jacobson JA, et al. Normal MR imaging findings of the mid-hand and fingers with anatomic correlation. Eur J Radiology. 2005; 56: 278-285.
- Lifchez SD. Flexor tendon injuries. Orthopedics. 2011;34(9):710-711.
- Hauger O, Chung CB, Lektrakul N, et al. Pulley system in the fingers: normal anatomy and simulated sesions in cadavers at MR imaging, CT, and US with and without contrast material distention of the tendon sheath. Radiology. 2000; 217(1):201-212.
- Talwalkar SC. Ligament injuries of the hand. Orthopaedics and Trauma. 2014; 28(4): 225-229.
- Theumann NH, Pessis E, Lecompte M, et al. MR imaging of the metacarpophalangeal joints of the fingers: evaluation of 38 patients with chronic joint disability. Skeletal Radiol. 2005; 34(4):210-216.
- Jarraya M, Hayashi D, Roemer FW, et al. Radiographically occult and subtle fractures: a pictoral review. Radiology Research and Practice. 2013.
- Ostergaard M, Peterfy C, Conaghan P, et al. OMERACT rheumatoid arthritis magnetic resonance imaging studies. core set of MRI acquisitions, joint pathology definitions, and the OMERACT RA-MRI scoring system. J Rheumatol. 2003; 30(6):1385-1386.
- Haugen IK, Englund M, Aliabadi P, et al. Prevalence, incidence and progression of hand osteoarthritis in the general population: The Framingham Osteoarthritis Study. Ann Rheum Dis 2011, 70(9):1581-1586.
- Haugen IK, Slatkowsky-Christensen B, Bøyesen P, et al. MRI findings predict radiographic progression and development of erosions in hand osteoarthritis. Clin Epid Res. 2014.
- Myasoedova E, Crowson CS, Kremers HM, et al. Is the incidence of rheumatoid arthritis rising?: results from Olmsted County, Minnesota, 1955-2007. Arthritis Rheum. 2010;62(6):1576-1582.
- Boutry N, Morel M, Flipo R, et al. Early rheumatoid arthritis: a review of MRI and sonographic findings. AJR Am J Roentgenol. 2007;189(6): 1502-1509.
- McQueen FM, McHaffie A, Clarke A, et al. MRI osteitis predicts cartilage damage at the wrist in RA: a three-year prospective 3T MRI study examining cartilage damage. Arthritis Res Ther. 2014;16(1):R33.
- Turesson C, Jacobsson LT. Epidemiology of extra-articular manifestations in rheumatoid arthritis. Scand J Rheumatol. 2004;33(2):65-72.
- El-Noueam Kl, Giuliano V, Schweitzer ME, et al. Rheumatoid nodules: MR/pathological correlation. J Comput Assist Tomogr. 1997;21(5)796-799.
- Spira D, Kotter I, Henes J, et al. MRI findings in psoriatic arthritis of the hands. AJR Am J Roentgenol. 2010;195(5):1187-1193.
- Boutry N, Hachulla E, Flipo RM, et al. MR imaging findings in hands in early rheumatoid arthritis: comparison with those in systemic lupus erythematosus and primary Sjögren Radiology. 2005;236(2):593-600.
- Kransdorf MJ, Meis JM. From the archives of the AFIP. Extraskeletal osseous and cartilaginous tumors of the extremities. Radiographics. 1993;13(4):853-884.
- Garcia J, Bianchi S. Diagnostic imaging of tumors of the hand and wrist. Eur Radiol. 2001;11(8):1470-1482.
- Murphey MD, Flemming DJ, Boyea SR, et al. Enchondroma versus chondrosarcoma in the appendicular skeleton: differentiating features. Radiographics. 1998;18(5):12131237.
- Kransdorf MJ, Murphey MD. MR imaging of musculoskeletal tumors of the hand and wrist. Magn Reson Imaging Clin N Am. 1995;3(2):327-244.
- Milgram JW. The origins of osteochondromas and enchondromas. a histopathologic study. Clin Orthop Relat Res. 1983;174:264-84.
- Hudson TM, Hamlin DJ, Enneking WF, et al. Magnetic resonance imaging of bone and soft tissue tumors: early experience in 31 patients compared with computed tomography. Skeletal Radiol. 1985;13(2):134-146.
- Bohndorf K, Reiser M, Lochner B, et al. Magnetic resonance imaging of primary tumours and tumour-like lesions of bone. Skeletal Radiol. 1986;15(7):511-517.
- Kransdorf MJ, Sweet DE, Buetow PC, et al. Giant cell tumor in skeletally immature patients. Radiology. 1992;184(1):233-237.
- Dahlin DC. Giant-cell-bearing lesions of bone of the hands. Hand Clin. 1987;3(2):291-297.
- Bogumill GP, Sullivan DJ, Baker GI. Tumors of the hand. Clin Orthop Relat Res. 1975;(108):214-222.
- Butler ED, Hamill JP, Seipel RS, et al. Tumors of the hand. A ten-year survey and report of 437 cases. Am J Surg. 1960;100:293-302.
- Cardinal E, Buckwalter KA, Braunstein EM, et al. Occult dorsal carpal ganglion: comparison of US and MR imaging. Radiology. 1994;193(1): 259-262.
- Ogino T, Minami A, Kato H, et al. Entrapment neuropathy of the suprascapular nerve by a ganglion. A report of three cases. J Bone Joint Surg Am. 1991;73(1):141-147.
- Feldman F, Singson RD, Staron RB. Magnetic resonance imaging of para-articular and ectopic ganglia. Skeletal Radiol. 1989;18(5):353-358.
- Savage RC, Mustafa EB. Giant cell tumor of tendon sheath (localized nodular tenosynovitis). Ann Plast Surg. 1984;13(3):205-210.
- Narváez JA, Narváez J, Aguilera C, et al. MR imaging of synovial tumors and tumor-like lesions. Eur Radiol. 2001;11(12):2549-2560.
- Allen PW, Enzinger FM. Hemangioma of skeletal muscle. An analysis of 89 cases. Cancer. 1972;29(1):8-22.
- Buetow PC, Kransdorf MJ, Moser RP Jr, et al. Radiologic appearance of intramuscular hemangioma with emphasis on MR imaging. AJR Am J Roentgenol. 1990;154(3):563567.
Citation
JC M, KS P, HW G, JM B, DE W, JJ P.MRI of the hand and fingers. Appl Radiol. 2016; (2):9-21.
February 3, 2016