Paratesticular Solitary Fibrous Tumor Masquerading as Metastatic Prostate Cancer
Images


CASE SUMMARY
An 84-year-old male with a prior diagnosis of prostate adenocarcinoma (PCa) and increasing prostate-specific antigen (27.9 ng/mL) presented to our clinic. The patient had previously declined treatment for his prostate malignancy and now sought care for an increasingly bothersome scrotal swelling of two years’ duration. Physical examination revealed a solid intrascrotal mass superior and distinct to the left testis and otherwise normal genitourinary findings.
IMAGING FINDINGS
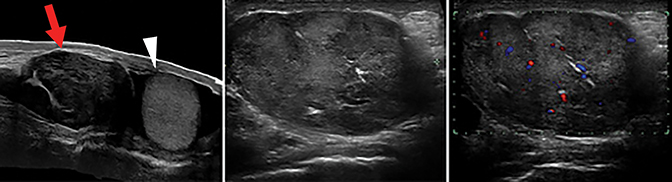
Scrotal ultrasound revealed an intrascrotal heterogeneous solid mass, in the left inguinal region adjacent to the left testis, measuring 8.2cm in diameter (Figure 1). Bilateral testes were without abnormality, and demonstrated normal vascular flow. Given the elevated PSA and finding of a solid left paratesticular mass, there was a clinical suspicion for metastatic prostate cancer. A 99mTc bone scintigraphy was performed and showed no evidence of bony metastatic disease.
Given the patient’s significant discomfort and uncertainty of the diagnosis, the patient elected to undergo excision of the mass. Through a left inguinal incision the mass and left testis were delivered. (Figure 2). Upon examination, the mass was distinct and uninvolved with the left testis and cord structures. Therefore, only the mass was excised, sparing the left testis.
Gross evaluation showed a well-circumscribed neoplasm with a homogeneous white-tan cut surface and composed of firm parenchyma. Microscopic evaluation demonstrated a proliferation of bland spindled and epithelioid cells with moderate amounts of pale eosinophilic cytoplasm and virtually absent mitotic activity. The cells were present without distinct pattern or architectural arrangement, within a highly vascular and collagenous stroma containing prominent hyalinized collagen bands. Immunohistochemistry was diffusely positive for CD34, BCL2, CD99, and negative for CD45, CD31, ERG, calretenin, pan-cytokeratin (OSCAR), desmin, SMA, and D2-40 (Figure 3).
DIAGNOSIS
Solitary fibrous tumor (SFT) in an extrapleural paratesticular location
DISCUSSION
Solitary fibrous tumors are mesenchymal neoplasms with pleural origins; most are benign.1 Extrapleural SFTs are observed in adults ranging in age from 20 to 70 years, with a median age of 50 years at diagnosis. They can be found in the subcutaneous tissues, the head and neck, and the meninges, as well as in the orbits, thoracic wall, mediastinum, pericardium, peritoneum, pelvis, adrenal glands, liver, and urogenital system.2 Genitourinary SFTs are very rare and their discovery in the paratesticular location is described in the literature sparingly.3 Zhou, et al, in 2015 described a paratesticular SFT and summarized 7 additional documented examples in the literature.4
Although most SFTs are benign,surgical excision remains the gold standard and can be curative; however, continued surveillance is warranted, as recurrences and metastases have been documented.5
CONCLUSION
Solitary fibrous tumor is a rare benign spindle cell neoplasm originating from mesenchymal cells typically arising from the pleura.6 Extrapleural sites have been described; however, the incidence of genitourinary SFTs is exceedingly low.7-9 We present a case of a paratesticular SFT that masqueraded as metastatic prostate cancer.
REFERENCES
- Gold JS, Antonescu CR, Hajdu C, et al. Clinicopathologic correlates of solitary fibrous tumors. Cancer. 2002; 94(4):1057-1068.
- Bruzzone A, Varaldo M, Ferrarazzo C, Tunesi G, Mencoboni M. Solitary fibrous tumor. Rare Tumors. 2010; 2(4): e64. doi: 10.4081/rt.2010.e64
- Park SB, Park YS, Kim JK, et al. Solitary fibrous tumor of the genitourinary tract. AJR Am J Roentgenol. 2011; 196(2): W132-7. doi: 10.2214/AJR.09.3787.
- Zhou Y, Gong G, Tang Y, Tang J, Gan Y, Dai Y. Paratesticular solitary fibrous tumor: a case report and review of literature. Int J Clin Exp Pathol. 2015; 8(3): 3358-3361.
- Ronchi A, Cozzolino I, Zito Marino F, et al. Extrapleural solitary fibrous tumor: a distinct entity from pleural solitary fibrous tumor. An update on clinical, molecular and diagnostic features. Ann Diagn Pathol. 2018;34 142-150. doi: 10.1016/j.anndiagpath.2018.01.004. Epub Apr 9, 2018.
- Lee GE, Rha SE, Byun JY, Lee K, Kim SW. Paratesticular solitary fibrous tumor: a rare cause of a hypervascular extratesticular mass. J Ultrasound Med. 2011; 30(2): 279-281.
- Hu S, Yi L, Yang L, Wang Y. Solitary fibrous tumor of the spermatic cord: a case report and literature review. Exp Ther Med. 2015; 9(1): 55-58.
- Westra WH, Grenko RT, Epstein J. Solitary fibrous tumor of the lower urogenital tract: a report of five cases involving the seminal vesicles, urinary bladder, and prostate. Hum Pathol. 2000; 31(1):63-68.
- Prunty MC, Gaballah A, Ellis L, Murray KS. Solitary Fibrous Tumor of the Pelvis Involving the Urinary Bladder. Urology. 2018;117: 27-30. doi: 10.1016/j.urology.2018.01.004. Epub Mar 12, 2018.
Citation
FC L, RE N, DR G, ER B. Paratesticular Solitary Fibrous Tumor Masquerading as Metastatic Prostate Cancer. Appl Radiol. 2020;(6):56A-56B.
November 6, 2020